November 13th, 2012 by Dr. Val Jones in Announcements, Celebrity Interviews
No Comments »
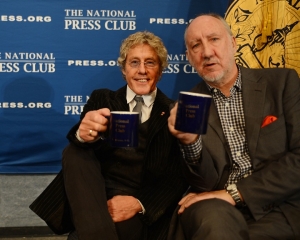 Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.
Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.
Sarah told the crowd what it was like to be a fifteen-year-old in a pediatric oncology unit populated by ukulele-playing clowns and screaming infants. The extreme age-related disconnect between her pscho-social needs and that of younger kids and babies served to make her feel even more isolated during her course of treatment. She longed for the companionship of others like her, but without any national cancer centers focused on the special needs of teens, she was on her own.
Roger Daltrey became interested in teen cancer when his personal physician took up the cause in the U.K. and turned to him for support. Daltrey’s decades of playing music to teen audiences made him keenly aware of their unique psycho-social needs. “When you’re a teenager, it’s horrifying if you have a spot on your nose. Imagine what it’s like if you have cancer!” said Daltrey.
Teen Cancer America began as a movement called the Teen Cancer Trust in the U.K. According to Daltrey, preliminary research (comparing teens treated in a typical NHS cancer ward versus a unit sponsored by the Teen Cancer Trust) suggests that there may be as much as a 15% survival advantage in being treated in the special units. Daltrey attributes this to increased morale that helps teens and families find the will to fight through life-threatening treatments.
When asked how American cancer centers compare to those in the U.K. Daltrey immediately responded that he believed the U.S. centers were far superior. He described the incredible resources available at UCLA and Duke, and how the facilities themselves were unbelievably beautiful, sporting plant-filled atria, massive skylights, and high tech imaging and radiation equipment. Nonetheless, he noted, “Teens don’t want to hang out in an atrium. There is just no place that appeals to teenagers at these centers.”
Whether specialized teen cancer treatment environments in the U.S. will dramatically improve survival rates remains to be seen, but there’s no doubt that recognizing the unique psycho-social needs of teenagers would be a boon for patients and families at pediatric cancer centers. Like post-traumatic stress disorder in military personnel, the psychological ravages of cancer may well be under recognized, especially in the teen and young adult populations.
Thank you Roger Daltry and Pete Townshend for bringing this to our attention.
***
Find out how to support Teen Cancer America here.
Check out The Who themed cookie from the press club event (delicious!):

September 1st, 2011 by EvanFalchukJD in Health Tips
No Comments »

Billionaire Teddy Forstmann has apparently been diagnosed with a serious form of brain cancer. There’s a tragic twist to the story: according to Fox Business News, Forstmann believes that for more than a year, he had been misdiagnosed with meningitis.
ABC News wonders:
How could such a misfortune befall a billionaire —- a man able to afford the best doctors, best technology and the most sophisticated diagnostic tests?
They’re missing the point. Misdiagnosis happens with shocking regularity – as much as Read more »
*This blog post was originally published at BestDoctors.com: See First Blog*
August 21st, 2011 by GarySchwitzer in News, Opinion
No Comments »

Right off the top, let me be clear that I am NOT minimizing the importance of this week’s news about an experimental treatment for leukemia – one that has drawn much news attention.
It is an important finding.
What I am commenting on herein is the news coverage.
The ABC television piece itself wasn’t bad, with good perspective from Dr. Len Lichtenfeld of the American Cancer Society. But the lead-in and the ending, both involving anchor Diane Sawyer, were hyperbolic. The following screenshot was part of Sawyer’s lead-in. Read more »
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
June 10th, 2011 by PJSkerrett in Health Tips, News
No Comments »


If the recent announcement by the International Agency for Research on Cancer (IARC) that cell phones may cause brain cancer has you worried, you might want to wait a bit before trashing your mobile phone and going back to a land line.
Last week, the IARC convened experts from around the world to assess what, if any, cancer threat cell phones pose to the 5 billion or so people who use them. After reviewing hundreds of studies, the IARC panel concluded that cell phone use may be connected to two types of brain cancer, glioma and acoustic neuroma.
That sounds mighty scary. But the IARC said the evidence for this conclusion was “limited.” Most studies have shown no connection between cell phone use and brain cancer. In the relatively small number of studies that have observed a connection between the two, the positive result could be due to chance, bias, or confounding.
The decision puts cell phones in IARC’s Group 2B category of agents that definitely or might cause cancer. Group 1 are things like asbestos, cigarette smoke, and ultraviolet radiation. Things in Group 2B are “possibly carcinogenic to humans.” Other denizens of this group include coffee, pickled vegetables, bracken ferns, and talcum powder.
I think the IARC decision puts cell phones on notice—a formal “we’ve got our eyes on you” warning—more than it fingers phones as a cause of brain cancer. For one thing, the evidence so far is pretty weak. Writing on the Cancer Research UK Web site, blogger Ed Yong offers a peak at the data through 2009, taken from a review by Swedish researchers. A graph from the paper shows that only one of 28 studies shows a statistically significant association between cell phone use and cancer. We’ll know more about the strength or weakness of the evidence when the panel publishes its report online later this week and in the July 1 issue of The Lancet Oncology.
For now, I’m far more concerned about being rammed by someone talking on his or her cell phone while driving than I am about getting brain cancer from a phone. If you think the IARC report warrants action, the FDA offers suggestions for reducing your exposure to radiofrequency energy from a cell phone, like using the phone less, texting instead of talking, and using speaker mode or a headset to place more distance between your head and the cell phone.
*This blog post was originally published at Harvard Health Blog*
February 26th, 2011 by PJSkerrett in Opinion, Research
No Comments »

 We all know that using a cell phone can stimulate the brain to work a bit harder. “Mr. Skerrett? This is Dr. LeWine’s office. Do you have a minute to talk about your test results?” or “Dad, a bunch of kids are going to Casey’s house after the dance. Can I go?” But a new study published in JAMA is making me wonder what the energy emitted by the phone itself — not just the information it delivers — is doing to my brain.
We all know that using a cell phone can stimulate the brain to work a bit harder. “Mr. Skerrett? This is Dr. LeWine’s office. Do you have a minute to talk about your test results?” or “Dad, a bunch of kids are going to Casey’s house after the dance. Can I go?” But a new study published in JAMA is making me wonder what the energy emitted by the phone itself — not just the information it delivers — is doing to my brain.
Here’s the study in a nutshell. Dr. Nora Volkow and her colleagues recruited 47 volunteers to have their brain activity measured twice by a PET scanner. Both times the volunteer had a cell phone strapped to each ear. During one measurement, both phones were turned off. During the other, one phone was turned on but muted so the volunteer didn’t know it was on; the other was left off. Each session lasted about an hour. The scans showed a small increase in the brain’s use of glucose (blood sugar) when the phone was on, but only in parts of the brain close to the antenna.
It was an elegant study. The researchers took pains to anticipate sources of error. They used a control (both phones off) against which to compare the effect of a “live” cell phone. They used cell phones on each ear, one on and one off, to see if the effect was localized. They muted the phone that was on to eliminate the possibility that any brain activation was due to listening to the sound of a voice coming through the phone’s speaker. So the result is probably a real one, not an artifact or measurement error.
What does this brain activation mean? No one really knows. As Dr. Volkow told NPR, “I cannot say if it is bad that they [cell phones] are increasing glucose metabolism, or if it could be good.” Read more »
*This blog post was originally published at Harvard Health Blog*
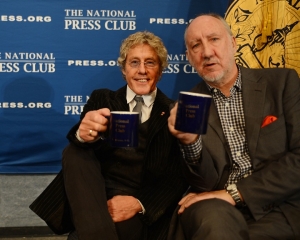 Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.
Rock superstars Roger Daltrey and Pete Townshend of “The Who” have a new cause: sparking a franchise of teen-oriented cancer treatment centers across America. To kick off the launch of Teen Cancer America, Daltrey & Townshend were featured at a conference held at the National Press Club in Washington, D.C. I was fortunate to be invited to sit at the head table next to teen cancer survivor Sarah Sterner – a bright and confident young woman from Atlanta who was cured of brain cancer two years ago.

















