December 7th, 2010 by Bryan Vartabedian, M.D. in Better Health Network, Opinion
No Comments »

 We all want technology to improve communication between doctors and patients. We fantasize that social tools will open doors and bridge the expanding divide between doctors and patients.
We all want technology to improve communication between doctors and patients. We fantasize that social tools will open doors and bridge the expanding divide between doctors and patients.
I’m wondering if it’s a case of unicorns and rainbows: Fancy new tools to do the old thing in a less-effective way. I’m guessing that if Facebook was the old platform for doctor-patient dialog and the telephone was invented this year, everyone would be clamoring to use the phone (“Dude, this is amazing…you can hear them talk.”)
I like the telephone. Written copy misses intonation, timing, pitch, and all the other rich elements of human speech. Subtle changes in a parent’s voice tell me if I’ve made my point and exactly how I need to proceed [with caring for their child]. Unspoken words on a screen are so one-dimensional.
Of course, email has a tightly-defined place in patient communication. And real-time social interaction between patient and clinic will evolve to have a clear role in patient care. But for now, the phone remains one of the most effective tools for helping doctor and patient really understand one another.
[Image credit: Cemagraphics]
*This blog post was originally published at 33 Charts*
December 3rd, 2010 by Bryan Vartabedian, M.D. in Better Health Network, Opinion, True Stories
No Comments »

I just can’t imagine life today as a medical student. Every medical publication in the palm of your hand. The capacity to create an audience and publish at your own will. Real-time dialog between students, faculty, anyone. Global reach from your phone. It’s mind-boggling really.
This is in stark contrast to my experience. My world was centered on index cards, textbooks and pens with different colors. We communicated via Post-it notes on the door of the student lounge. There were no apps and our only game was foozball. As a first year I scheduled time to compose H&Ps on the library’s only Macintosh II computer. This was plugged into the new Apple LaserWriter with WYSIWYG. Hi tech we were. We thought.
Being distractible and restless, I’m going to guess that if I had access to the communication platforms and tools available to today’s students, I might not have made it through. The inputs must be staggering and I imagine that discipline with personal bandwidth has become a critical key to survival. Read more »
*This blog post was originally published at 33 Charts*
November 27th, 2010 by Bryan Vartabedian, M.D. in Better Health Network, Health Policy, Opinion
No Comments »

I [recently] participated in an interview for an upcoming publication. As the interview wound down, the dialog downshifted into small talk that included, among other things, hospital blogs.
The interviewer (who had recently been exploring the blogging community) asked me what I thought about Thrive’s (Boston Children’s Hospital blog) recent birthday nod to Seattle Mama Doc (Seattle Children’s Hospital blog). More specifically, did I think it was unusual that one children’s hospital would congratulate a competing institution on its one-year anniversary?
I thought the question was odd but it got me thinking: Do children’s hospitals compete in the social space? I don’t think so. They shouldn’t. And if they were competing, what would they be competing for?
Children’s hospitals are inherently regional. Parents of the northwest see Seattle Children’s as the end of the earth. In the northeast, Boston Children’s is the bee’s knees. And while specialty service lines like congenital heart surgery may draw patients from around the world, most kids come from their corner of the world.
Then there’s the broader question about the point of a blog for a children’s hospital. Is it a marketing gimmick or does it serve a higher function? Read more »
*This blog post was originally published at 33 Charts*
November 22nd, 2010 by Bryan Vartabedian, M.D. in Better Health Network, Health Policy, News
No Comments »

A new policy on professionalism in the use of social media was [recently] adopted by the American Medical Association (AMA). The AMA Office of Media Relations was kind enough to share a copy of the policy:
The Internet has created the ability for medical students and physicians to communicate and share information quickly and to reach millions of people easily. Participating in social networking and other similar Internet opportunities can support physicians’ personal expression, enable individual physicians to have a professional presence online, foster collegiality and camaraderie within the profession, provide opportunity to widely disseminate public health messages and other health communication. Social networks, blogs, and other forms of communication online also create new challenges to the patient-physician relationship. Physicians should weigh a number of considerations when maintaining a presence online:
(a) Physicians should be cognizant of standards of patient privacy and confidentiality that must be maintained in all environments, including online, and must refrain from posting identifiable patient information online.
(b) When using the Internet for social networking, physicians should use privacy settings to safeguard personal information and content to the extent possible, but should realize that privacy settings are not absolute and that once on the Internet, content is likely there permanently. Thus, physicians should routinely monitor their own Internet presence to ensure that the personal and professional information on their own sites and, to the extent possible, content posted about them by others, is accurate and appropriate. Read more »
*This blog post was originally published at 33 Charts*
November 16th, 2010 by Bryan Vartabedian, M.D. in Better Health Network, Health Policy, Opinion, True Stories
1 Comment »

When perusing my Twitter feed [one] morning, I stumbled onto this post directed to me:
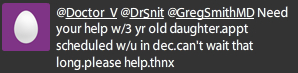
Patients reaching me in public social spaces is becoming a regular thing. I’ve discussed this in the past, but I think it bears repeating. So here’s what I did:
I understood the mom’s needs. Patients resort to “nontraditional” means of communication when the traditional channels fail to meet their needs. Recognize that these patients (or parents in my case) are simply advocating for themselves. My specialty struggles with a shortage of physicians, so we’re dependent upon phone triage to sort out the really sick from the less-than-sick. It’s an imperfect system and consequently parents find themselves having to speak up when the gravity of their child’s condition hasn’t been properly appreciated.
I took the conversation offline. I don’t discuss patient problems in places where others can see, so my first order of business in this case was to get the conversation to a place where it can be private. I called the mom, found out what was going on, and rearranged her appointment to a time appropriate to the child’s problem. Read more »
*This blog post was originally published at 33 Charts*
![]() We all want technology to improve communication between doctors and patients. We fantasize that social tools will open doors and bridge the expanding divide between doctors and patients.
We all want technology to improve communication between doctors and patients. We fantasize that social tools will open doors and bridge the expanding divide between doctors and patients.