October 28th, 2011 by DavidHarlow in Opinion
No Comments »

I’m back from my pilgrimage to Rochester, MN for the Third Annual Health Care Social Media Summit at the Mayo Clinic, presented by Ragan Communications. I had a great time, and want to share the experience with you. So please take a look at the archived #mayoragan tweets, my presentation on health care social media and the law, and my blog posts about the pre-conference and the summit itself posted at HealthWorks Collective. Here are some excerpts:
Mayo Ragan Social Media Summit Pre-Conference:
A recurring theme in my hallway conversations [today] was that it is impossible to transplant a successful program from one location to another without taking into account myriad local conditions (social media program, heart transplant program – same problem). As I always say to folks Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
July 13th, 2011 by admin in News, Opinion
No Comments »

In Keeping Score on How You Take Your Medicine, Tara Parker-Pope of the New York Times, reports on a new initiative from the Fair Isaac Corporation (FICO) known previously for its credit score ratings. FICO has developed a Medication Adherence Score, using publicly identifiable information (like employment status, age and gender) to determine a patient’s score, which it says “can predict which patients are at highest risk for skipping or incorrectly using prescription medications.”
Parker-Pope reports, “By the end of the year, an estimated two million to three million patients will have been given a FICO medication adherence score and a total of 10 million patients are expected to be scored during the next 12 months…FICO officials say insurance companies and other health care groups will use the score to identify those patients who could benefit the most from follow-up phone calls, letters and e-mails to encourage proper use of medication.”
The FICO medication adherence score has not received a universally warm reception: e-Patient Dave and Society for Participatory Medicine member Alexandra Albin point out that the score only accounts for whether prescriptions are purchased, not whether the pills have actually been taken.
In a related effort, Geisinger Health Systems and CVS Caremark are conducting a study to assess whether enhanced doctor-pharmacist communication can help with medication adherence. Shefali S. Kukarni reports in Tracking Down Patients Who Skip Their Drugs that, “The 18-month investigation will track a prescription from the moment it is submitted electronically to the pharmacy until it reaches the patient. If the patient does not pick up the prescription a ‘red flag’ or some form of notification will be sent to the doctor.”
But as Jessie Gruman recently blogged, there is no magic pill to cure poor medication adherence. Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
March 11th, 2011 by DavedeBronkart in Research, True Stories
No Comments »

 [Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.
[Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.
It’s a good combination: Pat speaks from the heart about her own experience and her passion for community, and Susannah, as usual, speaks as an “internet geologist” — as she once put it, “A geologist doesn’t have opinions about the rocks, she just observes and describes them.” Susannah spoke about her newly-released report “Peer-To-Peer Healthcare,” about which she recently wrote here.
Listener comments begin around 13:00. Examples:
— A woman describes how she started a Facebook group for her painful chronic condition (ankylosing spondylitis) and it’s grown into a website, HurtingButHelpful.org. (Spoonies, take note!) What drove her to create a patient community? “There’s no one else who can understand what I’m talking about.”
— The mother of a newborn with a heart defect found similar parents online. Hearing their stories — and even seeing an upsetting photo — helped her prepare for the surgery.
— On the downside, the daughter of an ovarian cancer patient said her now-cured mom keeps going online to patient communities and getting scared by what she reads. (Host Neal Conan’s observation: “There other parts of the computer that can be addictive, and I guess this one can, too.”)
It’s heartening to hear coverage of online patient communities, including the risks and challenges, in a respected outlet like NPR. (Time covered it, too, a year ago.) And there’s no equal for the reality check of Pew’s data. Some patient activists suggest (and some people fear) that the Internet “frees” patients from doctors, but Pew says that’s not what people are doing. Read more »
*This blog post was originally published at e-Patients.net*
February 1st, 2011 by DavedeBronkart in Better Health Network, Opinion
No Comments »

I have a Google alert for “e-patient,” and sometimes I’m surprised what it catches. [Recently] it was this:
3 Reasons Steve Jobs Will Be The Ultimate e-Patient
Steve Jobs’ medical leave sets the stage for the upcoming revolution in the production and delivery of medical information at time of diagnosis. 3 things you need to know.
So I’m thinking: “Oh, wow: Is the term ‘e-patient’ going mainstream?” That would be a hoot, because indeed the Society for Participatory Medicine is engaged in spreading the word.
*This blog post was originally published at e-Patients.net*
January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
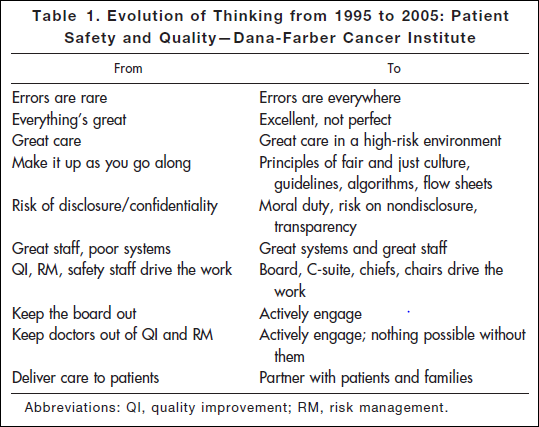
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
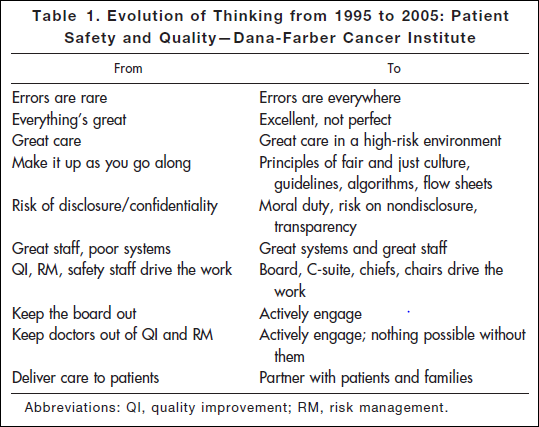
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*