March 27th, 2017 by Dr. Val Jones in Health Policy, True Stories
No Comments »
 We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
Take for example, the elderly woman who was leading an active life in retirement. She was the chairman of the board at a prestigious company, was an avid Pilates participant, and the caregiver for her disabled son. A new physician at her practice recommended a higher dose of diuretic (which she dutifully accepted), and several days later she became delirious from dehydration. She was admitted to the local hospital where it was presumed, due to her age, that she had advanced dementia. Hospice care was recommended at discharge. All she needed was IV fluids.
I recently cared for an attorney in her 70’s who had a slow growing brain tumor that was causing speech difficulties. She too, was written off as having dementia until an MRI was performed to explore the reason for new left-eye blindness. The tumor was successfully removed, but she was denied brain rehabilitation services because of her “history of dementia.”
Of course, I recently wrote about my 80-year-old patient, Jack, who was presumed to be an alcoholic when he showed up to his local hospital with a stroke.
Hospitalized patients are often very different than their usual selves. As we age, we become more vulnerable to medication side-effects, infections, and delirium. And so, the chance of an elderly hospitalized patient being acutely impaired is much higher than the general population. Unfortunately, many hospital-based physicians and surgeons — and certainly nurses and therapists — have little or no prior knowledge of the patient in their care. The patient’s “normal baseline” must often be reconstructed with the help of family members and friends. This takes precious time, and often goes undone.
Years ago, a patient’s family doctor would admit them to the hospital and care for them there. Now that the breadth and depth of our treatments have given birth to an army of sub-specialists, we have increased access to life-saving interventions at the expense of knowing those who need them. This presents a peculiar problem – one in which we spend enormous amounts of resources on diagnostic rabbit holes, because we aren’t certain if our patients’ symptoms are new or old. Was Mrs. Smith born with a lazy eye, or is she having a brain bleed? We could ask a family member, but we usually order an MRI.
My plea is for healthcare staff to be very mindful of the tendency to profile seniors. Just because Mr. Johnson has behavioral disturbances in his hospital room doesn’t mean that he is like that at home. Be especially suspicious of reversible causes of mental status changes in the elderly, and presume that patients are normally functional and bright until proven otherwise.
Last month I hit a new age record at my rehab hospital – I admitted a charming, active, 103-year-old woman after a small stroke caused her some new weakness. She was highly motivated in therapy, improved markedly and was discharged to an independent living center. I bet she will live many more years. When I joked that she didn’t look a day over 80, she winked and told me she had stopped counting birthdays years ago. She said, “It doesn’t matter how old you are, it matters what you can do. And I can do a lot.”
March 24th, 2015 by Dr. Val Jones in Opinion
No Comments »
 It’s no secret that physicians are experiencing burnout at an exponentially increasing rate in our progressively bureaucratic healthcare system. Many are looking for “alternative careers” as their salvation. I receive emails from physicians all the time, asking for advice about getting out of clinical medicine, since I have spent a few years outside it myself. As my own career pendulum has swung from full time clinical work to full time editorial and/or consulting work, I’ve found that the best mix is somewhere in between.
It’s no secret that physicians are experiencing burnout at an exponentially increasing rate in our progressively bureaucratic healthcare system. Many are looking for “alternative careers” as their salvation. I receive emails from physicians all the time, asking for advice about getting out of clinical medicine, since I have spent a few years outside it myself. As my own career pendulum has swung from full time clinical work to full time editorial and/or consulting work, I’ve found that the best mix is somewhere in between.
If you’re like me, you’re happiest using both halves of your brain. You have a creative side (I’m a cartoonist and blogger) and an analytic side (hospital-based physician). It’s not easy to make a living as a cartoonist or writer, and it’s soul-sucking to work 80 hour weeks in the hospital without rest. So how do you make a living, but participate in all the things you love? You work as a traveling physician (aka locum tenens) one third of your time, and spend the other two-thirds doing the creative things you also enjoy.
“But I couldn’t survive on 1/3 of my salary,” you say. Actually, I make the equivalent of a full-time academic physiatrist salary while working ~14 weeks a year as a traveling physician. Really? Yes, really. Because when I’m filling in at a hospital with an acute need, the work hours are long, and I’m paid by the hour. It can be grueling, but it is short, and the pay is fair so morale remains high. Drawing a flat employee salary (and then often discovering that the work load requires double the time estimated by the employer) can cause a lot of unconscious resentment. But when you are paid for your time, long hours aren’t as dread-worthy. This is what attorneys have been doing from day one, so why not physicians?
“But if all physicians suddenly dropped to half or 1/3 time, wouldn’t that do irreparable damage to patient access?” you cry. Yes, it could be catastrophic. However, if physicians stay the course and do nothing about our burnout, then the powers that be will continue tightening the vice – targeting physician reimbursement, increasing the burden of bureaucratic monitoring, pay for performance measures, and meeting “meaningless abuse” requirements for our electronic medical records systems. If there are no consequences to their actions, why would they ever stop?
I don’t think that most physicians will read this blog post and quit their jobs. I’m not worried about a sudden reduction in the physician work force. What I am offering is a suggestion for those of you who have a secret passion outside of clinical practice – a pathway that allows you to continue practicing medicine, and also enjoy cultivating your other talents. I’m hoping my advice will actually reduce the full drop out rate (if you believe the polls, up to 60% of PCPs would retire today if they had the means) to partial drop out rate (keeping those wanting to quit completely working part time).
So if there’s something you’ve always wanted to do (A non-profit endeavor? A low-paying, but rewarding job? Running a small business that can’t pay all the bills but is fun to do?) I say do it! Life is too short to get caught on the clinical treadmill, driving your spirits into the ground. You love your patients but can’t tolerate the work pace? Don’t quit altogether… you can still be a fantastic, caring, clinician in fewer hours/week and make the salary you need to maintain a reasonable lifestyle.
Please see my previous blog post to gain more insight into whether or not locum tenens might work for you.
And here’s a video of my recent thoughts about locum tenens work:
The Benefits Of Locum Tenens Work
January 21st, 2015 by Dr. Val Jones in Opinion, True Stories
1 Comment »
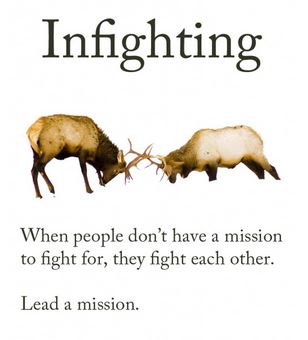 In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
Interestingly, the credibility question was raised in a different light when I was recently contacted by a prestigious medical organization that was seeking expansion of its board membership. I presumed that this was a personal invitation to join the cause, but soon realized that the caller wanted to use my influence to locate “more credible” candidates with academic gravitas.
When I asked what sort of candidate they wanted my help to find, the response was:
“A physician with an academic appointment at a name brand medical school. Someone who isn’t crazy – you know, they have to be respected by their peers. Someone at Harvard or Columbia would be great. You must know someone from your training program at least.”
While I appreciated the honesty, I began thinking about the age-old “town versus gown” hostilities inspired by academic elitism. In medicine, as with many other professions, it is more prestigious to hold an academic position than to serve in a rural community. But why do we insist on equating credibility with academics?
Another facet of credibility lies in physicians’ tendencies to admire only those at the top of their specific specialty. Dr. Lucy Hornstein described this phenomenon in her powerful essay on “How To Drive Doctors To Suicide:”
“Practice that condescending look and use it at hospital staff events. Make it a point to ignore newcomers. Concentrate on talking just with your friends and laughing at inside jokes, especially when others are around. Don’t return their calls, and don’t take their calls if you can possibly help it. If you accidentally wind up on the phone with the patient’s primary physician, just tell them you’ve got it all under control, and that he (and the patient) are so lucky you got involved when you did.”
A reader notes:
“And perhaps those of us who do see patients should get some self esteem and stop fawning all over [physician thought leaders] at conferences like needy interns.”
And finally, there seems to be an unspoken pecking order among physicians regarding the relative prestige of various specialties. How this order came about must be fairly complicated, as dermatology and neurosurgery seem to by vying for top spots these days. I find the juxtaposition almost amusing. Nevertheless, it’s common to find physicians in the more popular specialties looking down upon the worker bees (e.g. hospitalists and family physicians) and oddballs (e.g. physiatrists and pathologists).
While I try very hard not to take offense at my peers’ dismissiveness of my career’s value, it becomes much more concerning when funding follows prejudicial lines in the medical hierarchy. As a sympathetic family physician writes:
“I have observed the inequitable distribution of resources from the less glamorous to the sexy sub specialties despite obvious patient needs. Unfortunately, the administridiots who usually lack any medical training, opt to place resources where they are most likely to attract headlines.”
Yes, caring for the disabled (PM&R) is “less glamorous” than wielding a colonoscope (GI) (again, not sure who made that decision?) but it should not be less credible, or become a target for budget cuts simply because people aren’t informed about how rehab works.
It is time to stop specialty prejudice and honor those who demonstrate passion for patients, regardless of which patient population, body part, or organ system they serve. Excellent patient care may be provided by academics, generalists, or specialists, by those who practice in rural areas or in urban centers. The best “thought leaders” are those who bring unity and an attitude of peer respect to the medical profession. With more of them, we may yet save ourselves from mutually assured destruction.
April 30th, 2014 by Dr. Val Jones in Announcements
No Comments »
 In case you hadn’t seen this announcement in my Twitter stream – there are a number of writing fellowships available for US medical students and residents. (Bloggers and those heavily engaged in social media are preferred.) Join The American Resident Project Writing Fellows in brainstorming about how to make the healthcare system better for future generations. Fellowships are awarded on a rolling basis. Opportunities for travel are included. From their website:
In case you hadn’t seen this announcement in my Twitter stream – there are a number of writing fellowships available for US medical students and residents. (Bloggers and those heavily engaged in social media are preferred.) Join The American Resident Project Writing Fellows in brainstorming about how to make the healthcare system better for future generations. Fellowships are awarded on a rolling basis. Opportunities for travel are included. From their website:
The American Resident Project is a platform for future physician leaders – medical students, residents and physicians newly in practice – to connect, explore ideas for transforming American health care delivery, and exchange these views with other health care providers and opinion leaders across the country.
Sponsored by ThinkWellPoint, The American Resident Project focuses on key issues affecting today’s frontline physician workforce, including:
New care coordination models
Strategies for patient engagement
Innovations in health technology
Join our growing community, lend your voice and share your ideas on these and other important topics shaping the future of health care delivery in America.
I will be playing a mentorship role in the program going forward, and look forward to meeting some of my young Writing Fellows in the near future!
Apply for the fellowship here.
 We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.

 It’s no secret that physicians are
It’s no secret that physicians are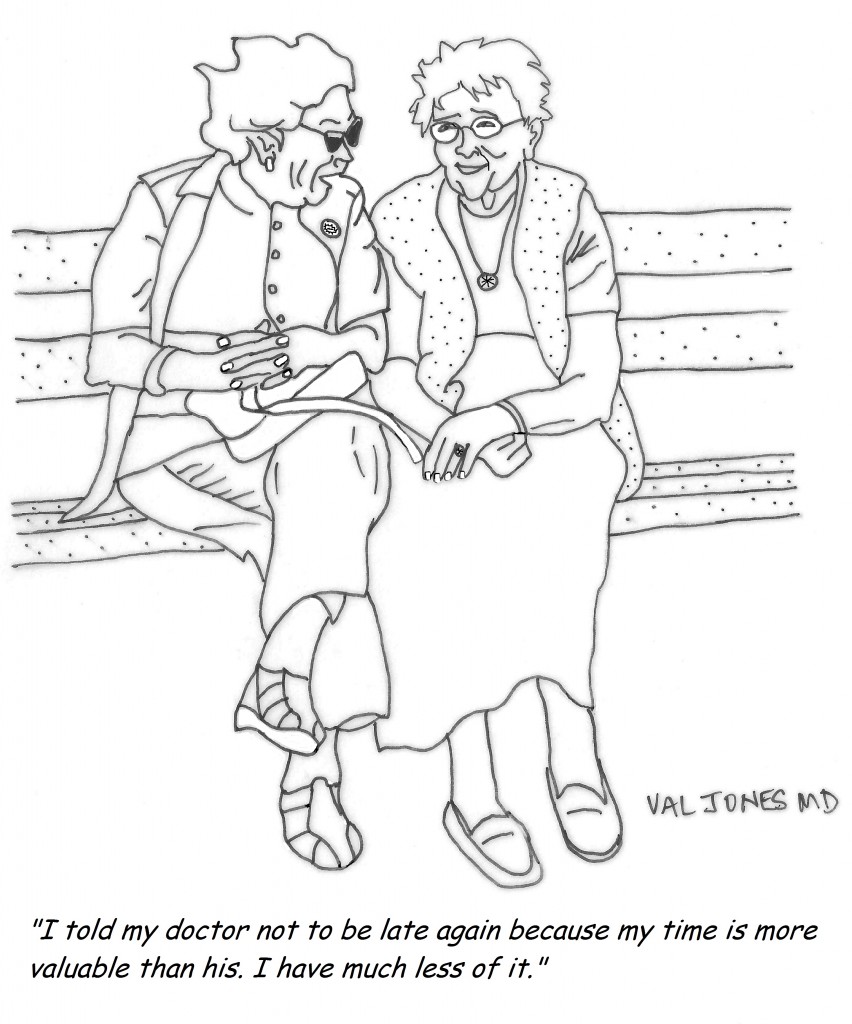
 In my
In my










