December 10th, 2010 by DavidHarlow in Better Health Network, Health Policy, News, Opinion
No Comments »
I’ve seen at least half a dozen links to the op-ed coauthored by Newt Gingrich and neurosurgeon Kamal Thapar about how the doctor used information on Facebook to save a woman’s life. (It was published by AOL News. Really.)
In brief, a woman who had been to see a number of different health care providers without getting a clear diagnosis showed up in an emergency room, went into a coma and nearly died. She was saved by a doctor’s review of the detailed notes she kept about her symptoms, etc., which she posted on Facebook. The story is vague on the details, but apparently her son facilitated getting the doc access to her Facebook page, and the details posted there allowed him to diagnose and treat her condition. She recovered fully.
Newt and Dr. Thapar wax rhapsodic about how Facebook saved a life, and sing the praises of social media’s role in modern medicine. (I’m not sure how this really fits in with Newt’s stance on health reform, within his 12-step program to achieve the total replacement of the Left…but, hey, nobody has the patience these days for so many details anyway.)
Regular readers of HealthBlawg know that I would perhaps be the last to challenge the proposition that social media has a role to play in health care. However, I think Newt got it wrong here. Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
December 1st, 2010 by Felasfa Wodajo, M.D. in Better Health Network, News, Opinion, Research
No Comments »

 In the future your medical apps might come from your hospital, not your app store. So says a recently published report by Research2Guidance, a mobile technology research company based in Germany. In their report, titled “Health Market Report 2010-2015″ the market researchers came to the conclusion that the dominant mode of application distribution in the future will be from doctors, hospitals and other care providers.
In the future your medical apps might come from your hospital, not your app store. So says a recently published report by Research2Guidance, a mobile technology research company based in Germany. In their report, titled “Health Market Report 2010-2015″ the market researchers came to the conclusion that the dominant mode of application distribution in the future will be from doctors, hospitals and other care providers.
The report also painted a bullish picture of healthcare app adoption, estimating that the number of users of mHealth apps on smartphone phones will reach 500m by 2015. However, the revenue from this sector will still be driven mostly by device sales and through provision of services, rather than by paid downloads.
The report preview shows it to be organized into three “dimensions”: a) The smartphone market, b) The current state of the mHealth market & c) mHealth outlook to 2015. One would imagine that the last portion will be the most avidly read read as the numerous stockholders in mHealth — telecoms, device makers, insurance and pharmaceutical companies, hospitals and entrepreneurs jockey to position themselves in this rapidly-evolving land grab. Read more »
*This blog post was originally published at iMedicalApps*
November 18th, 2010 by StevenWilkinsMPH in Better Health Network, News, Opinion, Research
No Comments »

What do cell phones and health-information seeking have in common? Very little, at least among the chronically ill (e.g., the folks who are driving healthcare use and cost). An American Medical News article about the latest Pew Research Center’s Internet & American Life Project study on mobile phone use caught my eye. The introduction to the article reads:
Despite the proliferation of cell phones in the United States, the number of people using them to access health information is low. But experts believe the sheer number of people using mobile phones and wireless devices means that health information eventually will get more mobile as well.
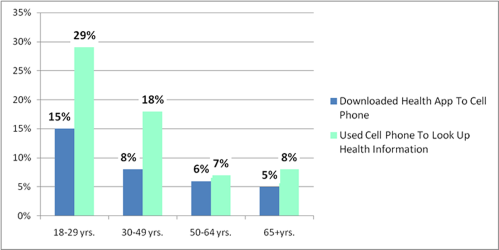
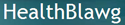
According to the study, 85 percent of Americans use mobile phones, but only 17 percent of cell phone owners have used them to look up health information. Nine percent of Americans have downloaded a health-related app on their cell phone.
Get this: The highest use of cell phone health-information seeking and downloading cell phone health apps was among 18- to 29-year olds at 29 percent and 15 percent respectively. With the exception of accidents, 18- to 29-year-old adults are generally among the most healthy demographic. Read more »
*This blog post was originally published at Mind The Gap*
October 31st, 2010 by DavidHarlow in Better Health Network, Health Policy, News, Opinion
No Comments »
I [recently] attended the Connected Health Symposium in Boston. I enjoyed many of the sessions (sometimes wished I could have attended two simultaneously, though the livetweeting — #chs10 — helped on that front), and as usual enjoyed the hallway and exhibit floor conversations too. As is often the case at conferences these days, I had the opportunity to meet several online connections in real life for the first time.
(I will not attempt to give a comprehensive report of the symposium here. Please see the livetweeting archive and other reports to get a sense of the rest of the event.)
This year’s exhibit floor included a diverse mix of distance health tools. Most striking from my perspective was the fact that most of these tools do one of two things: Enable patient-clinician videoconferencing, or upload data from in-home monitoring devices. The best of the second category also trigger alerts resulting in emails or PHR/EHR alerts to clinicians if vital signs are out of whack, or phone calls to consumers or their caregivers if, for example, meds aren’t taken on time (one company had a pill bottle with a transmitter in the cap that signals when it’s opened; another had a Pyxis-like auto-dispenser, that looked like you’d need an engineer — or a teenager — to program it). One tool — Intel’s — seemed to combine most of these functions, and more, into one platform, but it’s barely in beta, with only about 1,000 units out in the real world.
The speakers this year seemed to return again and again to several major themes: (1) Is any particular connected health solution scalable? (2) Who will pay for connected health, or mobile health (mHealth)? and (3) Does it work? Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
October 11th, 2010 by DavidHarlow in Better Health Network, Health Policy, News, Opinion, Research
No Comments »
Last month, PricewaterhouseCoopers (PwC) issued a report, Healthcare Unwired, examining the market for mobile health monitoring devices, reminder services, etc. among both healthcare providers and the general public. One of the big take-away points seems to be that 40% of the general public would be willing to pay for mobile health (or “mHealth”) devices or services ranging from reminders to data uploads — and the reaction by insiders is either joy (40% is good) or dismay (40% is not enough).
PwC estimated the mHealth market to be worth somewhere between $7.7 billion and $43 billion per year, based on consumers’ expressed willingness to pay. Deloitte recently issued a report on mPHRs, as well — and there is tremendous interest in this space, as discussed in John Moore’s recent post over at Chilmark Research. I agree with John’s wariness with respect to the mHealth hype — there is certainly something happening out there, but significant questions remain: What exactly is going on? Is there reason to be interested in this stuff or is it just something shiny and new? Can mHealth improve healthcare status and/or healthcare quality and/or reduce healthcare costs? Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*



 In the future your medical apps might come from your hospital, not your app store. So says a recently published report by Research2Guidance, a mobile technology research
In the future your medical apps might come from your hospital, not your app store. So says a recently published report by Research2Guidance, a mobile technology research