June 28th, 2011 by American Journal of Neuroradiology in Research
No Comments »

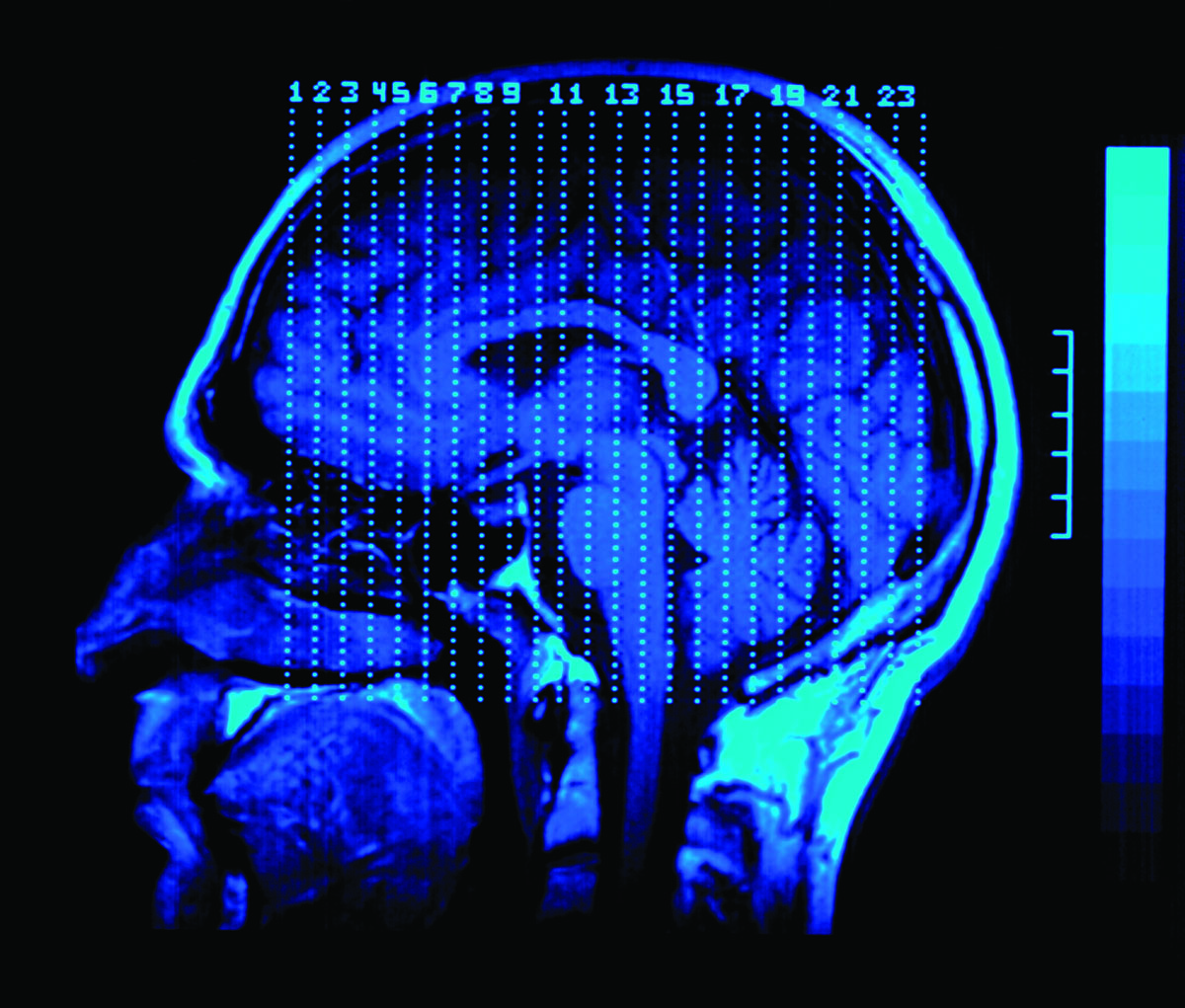
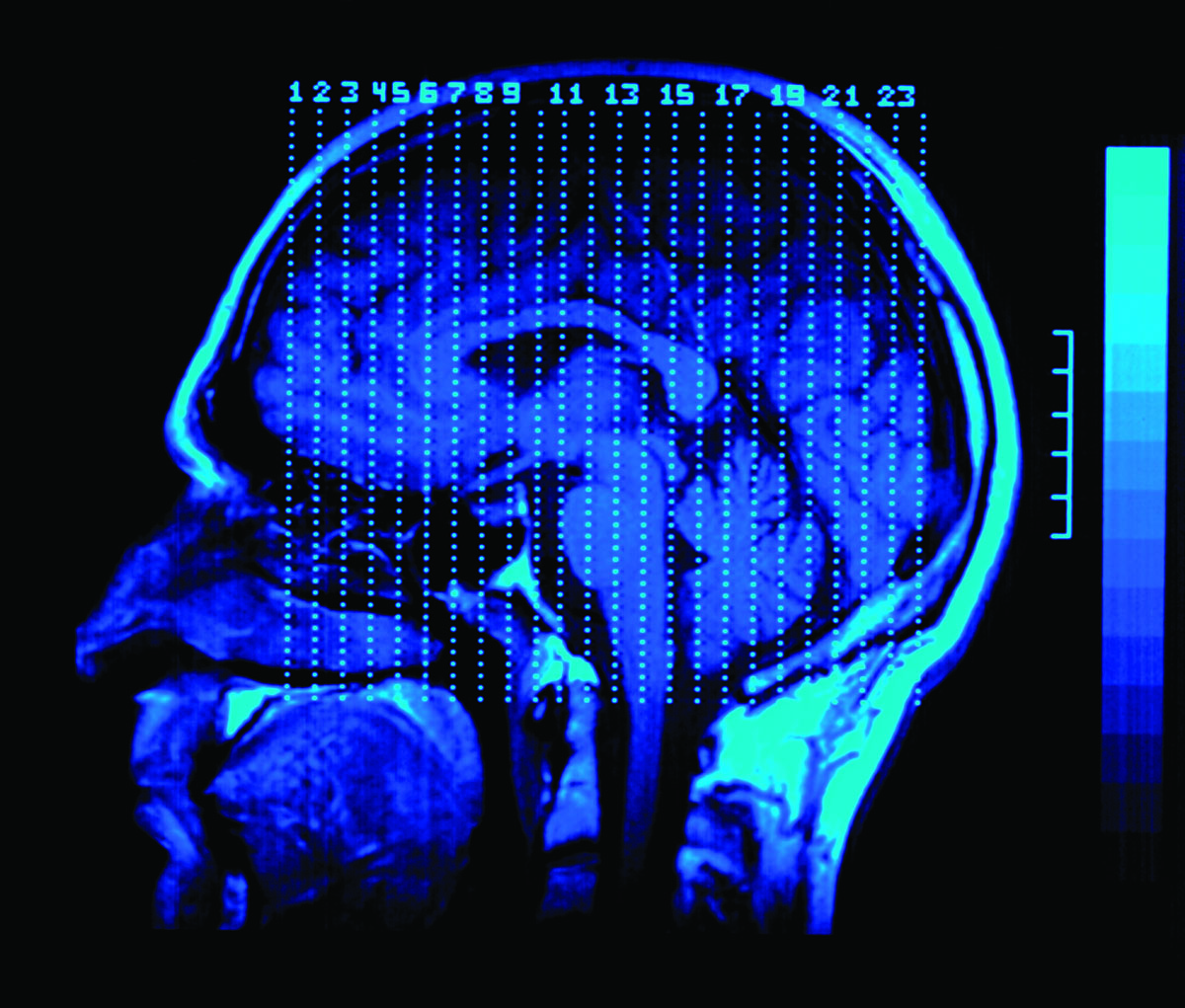
Gray matter (GM) damage, in terms of focal lesions,1 “diffuse” tissue injury, and atrophy is a well-known feature of multiple sclerosis (MS). Recently, T1-hyperintensity on unenhanced T1-weighted sequences has been found in the dentate nuclei of patients with MS with severe disability and high T2 lesion load.2 Such an abnormality has been interpreted as an additional sign of the neurodegenerative processes known to occur in the course of MS. This report describes a patient who, despite being mildly disabled and having a low T2 lesion load and no evident brain atrophy, showed a bilateral dentate nucleus T1 hyperintensity.
The patient was a 44-year-old man who had a diagnosis of relapsing-remitting MS (RRMS) in September 1997, after 3 relapses that occurred in June 1995, March 1997, and September 1997. Brain and cord MR imaging and CSF examination were suggestive of MS. After the diagnosis, he started treatment with interferonβ-1α, with clinical stability until January 2009, when he complained of vertigo, which gradually resolved after 5 days of steroidtreatment (methylprednisolone, 1 g daily intravenously). In September 2010, he entered a research protocol and underwent neurologic and neuropsychologic (Rao Brief Repeatable Neuropsychological Battery) evaluations and brain MR imaging on a 3T scanner. The neurologic examination showed Read more »
*This blog post was originally published at AJNR Blog*
May 28th, 2011 by GarySchwitzer in Health Tips
1 Comment »

On the NPR Shots blog, Scott Hensley writes, “Quality Prescription For Primary Care Doctors: Do Less,” about an article in the Archives of Internal Medicine. Excerpt:
“A group of docs who want to improve the quality and cost-effectiveness of primary care tinkered with some Top 5 lists for of dos and don’ts for pediatricians, family doctors and internists.
After testing them a bit, they published online by the Archives of Internal Medicine. Most of the advice falls in the category of less is more.
So what should family doctors not be doing? The Top 5 list for them goes like this:
1. No MRI or other imaging tests for low back pain, unless it has persisted longer than six weeks or there are red flags, such as neurological problems.
2. No antibiotics for mild to moderate sinusitis, unless it has lasted a week or longer. Or the condition worsens after first getting better.
3. No annual electrocardiograms for low-risk patients without cardiac symptoms.
4. No Pap tests in patients under 21, or women who’ve had hysterectomies for non-malignant disease.
5. No bone scans for women under 65 or men under 70, unless they have specific risk factors.”
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
April 1st, 2011 by admin in Book Reviews
No Comments »


Hall WA, Nimsky C, Truwit CL. Intraoperative MRI-Guided Neurosurgery. Thieme 2010, 272 pages, $159.95.
This book is a multiauthored text edited by three senior authors who have a tremendous experience in the use of intraoperative MRI technology. The book is divided into five sections that describe the various iterations of iMRIs that are available, its application for minor procedures, the resection of neoplastic lesions, and its role in the management of nonneoplastic disorders. The last section focuses on the future improvements in design that are likely to improve surgical access and utility of this burgeoning technology.
The first section describes the characteristics of iMRI machines that are available in the low, medium and high field strength. The reader gets a very good idea about the relative benefits and limitations of each of these machines. Hospitals that may be in the process of deciding which technology to go in for may use this information as a good guide. This section also highlights the optimal pulse sequences that may help differentiate tumor-brain interface, perform intraoperative fMRI and DTI tracking and detect complications related to brain ischemia and hematoma formation. The chapters in this section are well illustrated and show both the technology and the images obtained with various units. The chapter on optimal pulse sequences is very well written and discusses the specific pulse sequences that can help obtain the maximum intraoperative information with the least amount of time. These sequences can be tailored to provide not only anatomical details but also to help obtain both DTI and functional activation data for intraoperative neuronavigation, thereby accounting for brain shifts and movement of eloquent tracts during surgery. The authors describe the challenges of this methodology. Specific anesthetic challenges that restrict the use of standard monitoring equipment have been outlined. These include patient access, length of operative procedure, influence of magnetic field and RF currents on the functioning of the equipments and the images obtained, and risk of migration of ferromagnetic instruments, among others. This has led to the development of MR compatible anesthesia and monitoring equipment. Safety issues and steps needed to ensure reliability of equipment have been described. Read more »
*This blog post was originally published at AJNR Blog*
March 31st, 2011 by admin in Health Policy, Health Tips, Research
No Comments »
By Richard C. Hunt, MD, FACEP
Centers for Disease Control and Prevention
A 17 year-old athlete arrives on the sideline, at your office, or in the emergency department after hitting her head during a collision on the sports field and is complaining that she has a headache and “just doesn’t feel right.”
Can she return to play? If not, when can she safely return to school, sports, and to her normal daily activities? Does she need immediate care, a Head CT or MRI, or just some time to rest?
Do those questions sound familiar?
Each year thousands of young athletes present at emergency departments and in the primary care setting with a suspected sports- and recreation-related concussion. And every day, health care professionals, like us, are challenged with identifying and appropriately managing patients who may be at risk for short- or long-term problems.
As you know, concussion symptoms may appear mild, but this injury can lead to significant, life-long impairment affecting an individual’s ability to function physically, cognitively, and psychologically. Thus, appropriate diagnosis, referral, and education are critical for helping young athletes with concussion achieve optimal recovery and to reduce or avoid significant sequelae.
And that’s where you come in. Health care professionals play a key role in helping to prevent concussion and in appropriately identifying, diagnosing, and managing it when it does occur. Health care professionals can also improve patient outcomes by implementing early management and appropriate referral.
As part of my work at CDC, and as a health care professional, I am committed to informing others about CDC’s resources to help with diagnosing and managing concussion. CDC collaborated with several organizations and leading experts to develop a clinical guideline and tools for the diagnosis and management of patients with concussion, including:
For more information about the diagnosis and management of concussion, please visit www.cdc.gov/Concussion/clinician.html.
Also, learn more about CDC’s TBI activities and join the conversation at: www.facebook.com/cdcheadsup.
March 20th, 2011 by American Journal of Neuroradiology in Research
No Comments »

We report a pathologically proved craniopharyngioma in the prepontine cistern. A 50-year-old woman presented with swallowing difficulty for 1 month. She underwent brain MR and CT imaging.
T1-weighted, T2-weighted, and contrast-enhanced T1-weighted images showed a large peripheral enhancing cystic mass in the prepontine cistern. Inside the lesion, high signal intensity (SI) on T1 and low SI on T2-weighted imaging were noted (Fig 1). The CT scan showed features similar to those on the MR images, except for the addition of a peripheral small calcification in the cystic lesion. We could not find any connection between the mass in the prepontine cistern and the sellar or parasellar area. The mass was partially surgically removed, and histopathologic examination revealed craniopharyngioma in the prepontine cistern.

View larger version (102K):
[in this window]
[in a new window]- Fig 1. A 50-year-old woman with a craniopharyngioma in the prepontine cistern. A, Sagittal T1-weighted image shows a cystic mass in the prepontine cistern. B, Contrast-enhanced T1-weighted sagittal image shows a peripheral enhancing cystic mass in the prepontine cistern. Read more »
*This blog post was originally published at AJNR Blog*