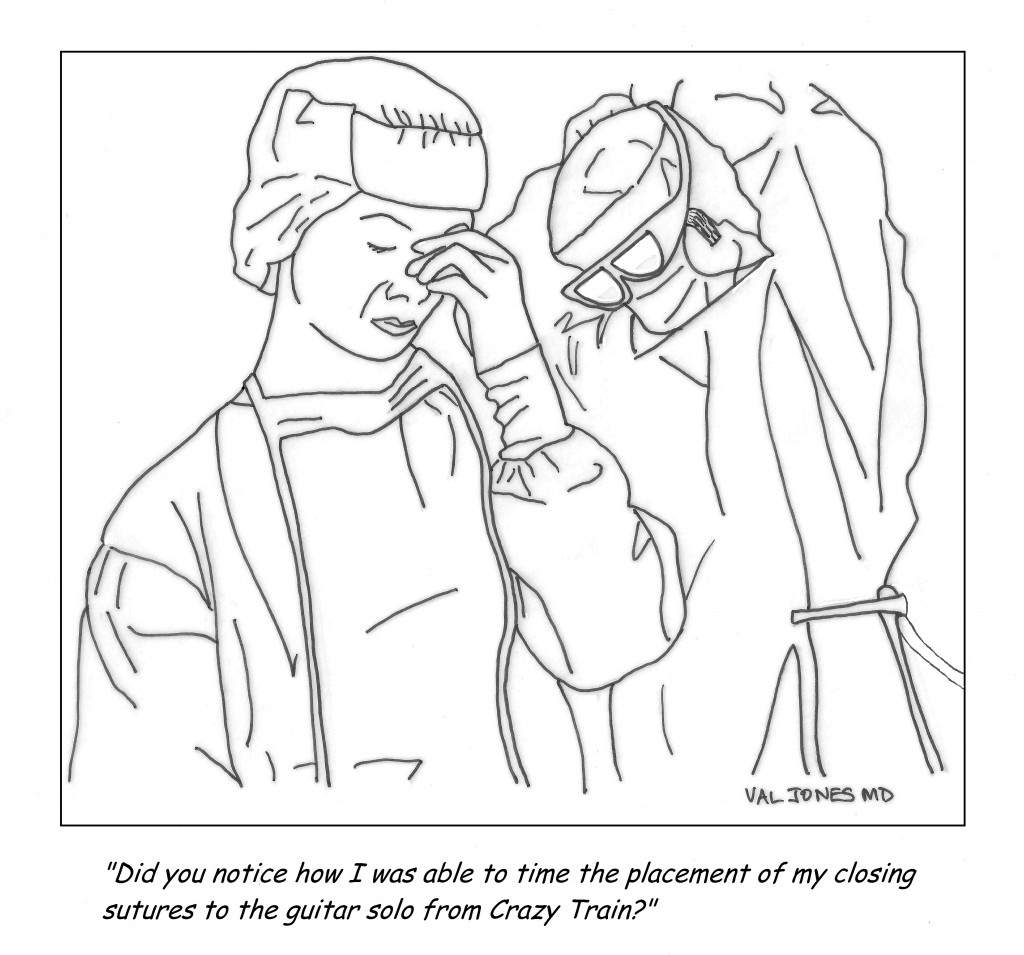
Cartoon: How Some Surgeons Behave In The O.R.

 As I travel the country providing coverage for inpatient rehab units, I have been struck by the generally high quality of nursing care. Excellent nurses are the glue that holds a hospital unit together. They sound the first alarm when a patient’s health is at risk, they double-check orders and keep an eye out for medical errors. Nurses spend more time with patients than any other hospital staff, and they are therefore in the best position to comment on patient progress and any changes in their condition. An observant nurse nips problems in the bud – and this saves lives.
As I travel the country providing coverage for inpatient rehab units, I have been struck by the generally high quality of nursing care. Excellent nurses are the glue that holds a hospital unit together. They sound the first alarm when a patient’s health is at risk, they double-check orders and keep an eye out for medical errors. Nurses spend more time with patients than any other hospital staff, and they are therefore in the best position to comment on patient progress and any changes in their condition. An observant nurse nips problems in the bud – and this saves lives.
Not only are nurses under-appreciated and under-paid, they are suffering as much as physicians are with new digital documentation requirements. Just as patients are receiving less face time with their physicians, they are also suffering from a reduction in bedside attention from nurses. The need to record data has supplanted our ability to listen to the patient, causing anguish for patients, physicians, and nurses alike.
This being our lot (and with continued “quality improvement” policies that will simply add to the documentation burden) we must find ways to optimize patient care despite inane bureaucratic intrusions. I believe that there are some steps that nurses and doctors can take to improve patient care right now:
1. Minimize “floating.” (Floating is when a nurse is pulled from one part of the hospital to fill in for a gap in coverage in a different unit). It is extremely difficult for nurses to take care of a floor full of patients they’ve never met before. Every time that care of a patient is handed off to someone else (be they MD or RN), there is a risk of forgetting to follow through with a test, procedure, or work up. Simply knowing what “normal” looks like for a given patient can be incredibly important.
For example, left sided weakness is not concerning in a patient with a long-time history of stroke, but what if that is a new finding? If you’ve never met the patient before, you might not realize that the weakness is new and constitutes an emergency. How does a nurse know if a patient’s skin ulcer/rash/pain etc. is better or worse than yesterday? Verbal reports don’t always clarify sufficiently. There are endless advantages to minimizing staff turnover during a patient’s hospital stay. Reducing the total number of nurses who care for individual patients should be a number one priority in hospitals.
2. If you see something, say something. There are a host of reasons why nurses may be hesitant to report patient symptoms. Either they don’t know the patient well and think that the new issue could be “normal” for that patient, or perhaps the physician managing the patient has been unreceptive to previous notifications. However, I am always grateful when a nurse goes out of her way to tell me her concerns, because I generally find that she’s on to something important. My general rule is to over-communicate. If you see something, say something – because that episode of patient anxiety in the middle of the night could be a heart attack. And if I don’t know it’s happening, I can’t fix it.
3. Please don’t diagnose patients without input. I’ve found that nurses generally have excellent instincts about patients, and many times they correctly pinpoint their diagnosis. But other times they can be misled, which can impair their care priorities. For example, I had a patient who was having some difficulty breathing. The nurse told me about it immediately (which was great) but then she proceeded to assume that it was caused by a pulmonary embolism. I explained why I didn’t think this was the case, but she was quite insistent. So much so that when another patient began to have unstable vital signs (and I requested her help with preparing for a rapid response) she stayed with the former patient, believing that his problem was more acute. This doesn’t happen that frequently, but I think it serves as a reminder that physicians and nurses work best as a team when diagnostic conundrums exist.
4. Help me help you. Please do not hesitate to come to me when we need to clean up the EMR orders. If the patient has had blood glucose finger stick checks of about 100 at each of 4 checks every day for 2 weeks, then by golly let’s reduce the checking frequency! If the EMR lists Q4 hour weight checks (because the drop down box landed on “hour” instead of “day” when it was being ordered) I’d be happy to fix it. If a digital order appears out of the ordinary, ask the doctor about it. Maybe it was a mistake? Or maybe there’s a reason for Q4 hour neuro checks that you need to be aware of?
5. Let’s round together. Nurses and physicians should really spend more time talking about patients together. I know that some physicians may be resistant to attending nursing rounds due to time constraints, but I’ve found that there’s no better way to keep a unit humming than to comb through the patient cases carefully one time each day.
This may sound burdensome, but it ends up saving time, heads off problems, and gives nurses a clearer idea of what to look out for. Leaving nurses in the dark about your plan for the patient that day is not helpful – they end up searching through progress notes (for example) to try to guess if the patient is going to radiology or not, and how to schedule their meds around that excursion. Alternately, when it comes time to update your progress note, isn’t it nice to have the latest details on the patient’s condition? Nurses and doctors can save each other a lot of time with a quick, daily debrief.
6. Show me the wounds. Many patients have skin breakdown, rashes, or sores. These are critically important to treat and require careful observation to prevent progression. Doctors want to see wounds at regular intervals, but don’t always take the time to unwrap or turn the patient in order to get a clear view. Alternatively, some MDs simply unwrap/undress wounds at will, leaving the patient’s room without even telling the nurse that they need to be re-wrapped. In some cases, it takes a lot of time to re-dress the complex wound, adding a lot of work to the nurse’s already busy schedule (and offering little benefit, and some degree of discomfort, to the patient).
Nurses, on the other hand, have the opportunity to see wounds more frequently as they provide dressing changes or peri-care at regular intervals. Most nurses and doctors don’t seem to have a good process in place for wound checks. I usually make a deal with nurses that I won’t randomly destroy their dressing changes if they promise to call me to the patient’s bedside when they are in the middle of a scheduled change. This works fairly well, so long as I’m willing/able to drop everything I’m doing for a quick peek.
These are my top suggestions from my most recent travels. I’d be interested in hearing what nurses think about these suggestions, and if they have others for physicians. I’m always eager to improve my patient care, and optimizing my nursing partnerships is a large part of that. 😆
 One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a locum tenens physician, traveling across the country to “cover” for my peers on vacation or when hospitals are having a hard time recruiting a full-time MD. This type of work is particularly vulnerable to gaps in continuity of care, and has heightened my awareness of the prevalence of poor sign-outs.
One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a locum tenens physician, traveling across the country to “cover” for my peers on vacation or when hospitals are having a hard time recruiting a full-time MD. This type of work is particularly vulnerable to gaps in continuity of care, and has heightened my awareness of the prevalence of poor sign-outs.
Recent research suggests that communications lapses are the number one cause of medical errors and adverse events in the healthcare system. An analysis published in the Archives of Internal Medicine suggests various kinds of consequences stemming from inadequate transfer of information, including missed diagnoses, incomplete work ups, ICU admissions, and near-miss errors. I have personally witnessed all manner of problems, including medication errors (the patient’s full list of medical conditions was not known by the new physician), lack of follow up for incidental (though life-threatening) findings discovered during a hospital stay, progression of infection due to treatment delay, inappropriate antibiotic therapy (follow up review of bacterial drug resistance results did not occur), accidental repeat fluid boluses in patients who no longer required rehydration (and had kidney or heart failure), etc.
It has long been suspected, though not unequivocally proven, that sleep deprivation (due to extended work hours and long shifts) is a common cause of medical errors. New regulations limiting resident physician work hours to 80 hours a week have substantially improved the quality of life for MDs in training, but have not made a remarkable difference in medical error rates. In my opinion, this is because sleep deprivation is a smaller contributor to the error problem than incomplete information transfer. If we want to keep our patients safe, we need to do a better job of transferring clinical information to peers assuming responsibility for patient care. This requires more than checklists (made popular by Atul Gawande et al.), it’s about creating a culture of carefulness.
Over the past few decades, continuity of care has been undermined by a new “shift worker” or “team” approach. Very few primary care physicians admit patients to local hospitals and continue to manage their care as inpatients. Instead, hospitalists are responsible for the medical management of the patient – often sharing responsibility as a group. This results in reduced personal knowledge of the patient, leading to accidental oversights and errors. The modern shift-worker model is unlikely to change, and with the rise of locum tenens physicians added to the mix – it’s as if hospitalized patients are chronically cared for by “float staff,” seeing the patient for the very first time each day.
As a physician frustrated with the dangers of chronically poor sign-outs, these are the steps that I take to reduce the risk of harm to my patients:
1. Attend nursing change of shift as much as possible. Some of the most accurate and best clinical information about patients may be obtained from those closest to them. Nurses spend more face-to-face time with patients than any other staff members and their reports to one another can help to nip problems in the bud. I often hear things like, “I noticed that Mr. Smith’s urine was cloudy and smelled bad this morning.” Or “Mrs. Jones complained of some chest pain overnight but it seems to be better now after the Percocet.” These bits of information might not be relayed to the physician until they escalate into fevers, myocardial infarctions, or worse. In an effort to not “bother the physician with too much detail” nurses often unwittingly neglect to share subtle findings that can prevent disease progression. If you are new to a unit or don’t already know the nursing staff well, join their morning or evening sign out meeting(s). They (and you) will be glad you did.
2. Pretend that every new patient needs an H&P (complete history and physical exam). When I pick up a new patient, I comb through their medical chart very thoroughly and carefully. I only need to do this once, and although it takes time, it saves a lot of hassle in the long run. I make note of every problem they’ve had (over the years and currently) and list them in a systems-based review that I refer to in every note I write thereafter.
3. Apply the “trust but verify” principle. I read other physicians’ notes with a careful eye. Electronic medical records systems are notorious for “copy and paste” errors and accidentally carrying over “old news” as if it were an active problem. If a physician notes that the patient has a test or study pending, I’ll search for its result. If they are being treated empirically for some kind of infection, I will look for microbiologic evidence that the bug is sensitive to the antibiotics they are receiving. I’ll ask the patient if they’ve had their radiology study yet, and then search for the result. I’ll review the active medication list and see if one of my peers discontinued or started a new medicine without letting me know. I never assume that anything in the medical record is correct. I try my best to double check the notes and data.
4. Create a systems-based plan of care, reconcile it each day with the active medication list. I like to organize patient diseases and conditions by body systems (e.g. cardiovascular, endocrine, gastrointestinal, neurologic, dermatologic, etc.) and list all the diseases/conditions and medications currently being offered to treat them. This only has to be done thoroughly one time, and then updated and edited with additional progress notes. This helps all consultants and specialists focus in on their particular area of interest and know immediately what is currently being done for the patient (both in their system of interest and as a whole) with a glance at your note. Since medications often have multiple purposes, it is also very helpful to see the condition being treated by each medication. For example, if the patient is on coumadin, is it because they have a history of atrial fibrillation, a prosthetic heart valve, a recent orthopedic procedure, or something else? That can easily be gleaned from a note with a systems-based plan of care.
5. Confirm your assessment and plan with your patient. I often review my patients’ medication and problem list with them (at least once) to ensure that they are aware of all of their diagnoses, and to make sure I haven’t missed anything. Sometimes a patient will have a condition (otherwise unmentioned in their record) that they treat with certain medications at home that they are not getting in the hospital. Errors of omission are not uncommon.
6. Sign out face-to-face or via phone whenever possible. These days people seem to be less and less eager to engage with each other face-to-face. Texting, emailing, and written sign-outs often substitute for face-to-face encounters. I try to remain “old school” about sign-outs because inevitably, something important comes up during the conversation that isn’t noted in the paper record. Things like, “Oh, and Mr. Smith tried to hit the nursing staff last night but he seems calmer now.” That’s something I want to know about so I can preempt new episodes, right nursing staff?
7. Create a culture of carefulness. As uncomfortable as it is to confront peers who may not be as enthusiastic about detailed sign-outs as I am, I still take the initiative to get information from them when I come on service and make sure that I call them to provide them with a verbal sign-out when I’m leaving my patients in their hands. By modeling good sign offs, and demonstrating their utility by heading off problems at the pass, I find that other doctors generally appreciate the head’s up, and slowly adopt some of my strategies (at least when working with me). I have found that nurses are particularly good at learning to tell me everything (no matter how small it may seem at the time) and have heard time and again that things “just run so much more smoothly” when we communicate and even “over-communicate” when in doubt.
“The Devil is in the details.” This is more true at your local hospital than almost anywhere else. Reducing hospital error rates is possible with some good, old-fashioned verbal handoffs and a small dose of charting OCD. Let’s create a culture of carefulness, physicians, so we don’t get crushed with more top-down bureaucratic rules to solve this problem. We can fix this ourselves, I promise.
Health care facilities should take five steps to ensure staff aren’t becoming sleep fatigued, according to a Sentinel Event Alert from The Joint Commission.
Shift length and work schedules impact job performance, and in health care, that means patient safety, the alert stated. A study of 393 nurses over more than 5,300 shifts showed that nurses who work shifts of 12.5 hours or longer are three times more likely to make an error in patient care.
Furthermore, residents who work traditional schedules with recurrent 24-hour shifts:
–make 36 percent more serious preventable adverse events than individuals who work fewer than 16 consecutive hours,
–make five times as many serious diagnostic errors,
–have twice as many Read more »
*This blog post was originally published at ACP Hospitalist*
 A Little History:
A Little History:
It’s 1958 and Ensign Thomas Eggleston is giving an inservice to US Navy Nurses LT. Frances Hogan, LCDR Magie Ziskovsky, and LCDR Edna Schnips about the Van Der Graaff teletherapy machine. The nurses were participating in the Nuclear Nursing Course at the National Naval Medical Center, Bethesda, MD. This machine was considered a medical breakthrough in its day. It looks antiquated now doesn’t it? I can only imagine what these Navy nurses were thinking while they stood next to this medical wonder.
Things have changed since I became a nurse. There were no CAT Scans or MRI machines when I graduated from school. There were no IV pumps either. We ran our IVs by counting drops that flowed into a drip chamber, and we monitored the hourly flow rate by glancing at a strip of medical tape that we marked off in CCs and ran down the side of each IV bottle. The nursing text books were different back then, too. There was no mention of AIDS and a diagnosis of Read more »
*This blog post was originally published at Nurse Ratched's Place*
It’s no secret that doctors are disappointed with the way that the U.S. healthcare system is evolving. Most feel helpless about improving their work conditions or solving technical problems in patient care. Fortunately one young medical student was undeterred by the mountain of disappointment carried by his senior clinician mentors…
I am proud to be a part of the American Resident Project an initiative that promotes the writing of medical students residents and new physicians as they explore ideas for transforming American health care delivery. I recently had the opportunity to interview three of the writing fellows about how to…
Book Review: Is Empathy Learned By Faking It Till It’s Real?

I m often asked to do book reviews on my blog and I rarely agree to them. This is because it takes me a long time to read a book and then if I don t enjoy it I figure the author would rather me remain silent than publish my…
The Spirit Of The Place: Samuel Shem’s New Book May Depress You

When I was in medical school I read Samuel Shem s House Of God as a right of passage. At the time I found it to be a cynical yet eerily accurate portrayal of the underbelly of academic medicine. I gained comfort from its gallows humor and it made me…
Eat To Save Your Life: Another Half-True Diet Book

I am hesitant to review diet books because they are so often a tangled mess of fact and fiction. Teasing out their truth from falsehood is about as exhausting as delousing a long-haired elementary school student. However after being approached by the authors’ PR agency with the promise of a…