May 29th, 2014 by Dr. Val Jones in Health Policy, Opinion
4 Comments »
 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In a policy environment where quality measures and patient satisfaction ratings are becoming the basis for reimbursement rates, one wonders how VMS software is getting traction. Perhaps desperate times call for desperate measures, and the challenge of filling employment gaps is driving interest in impersonal digital match services? Rural hospitals are desperate to recruit quality candidates, and with a severe physician shortage looming, warm bodies are becoming an acceptable solution to staffing needs.
As distasteful as the thought of computer-matching physicians to hospitals may be, the real problems of VMS systems only become apparent with experience. After discussing user experience with several hospital system employees and reading various blogs and online debates here’s what I discovered:
1. Garbage In, Garbage Out. The people who input physician data (including their certifications, medical malpractice histories, and licensing data) have no incentive to insure accuracy of information. Head hunter agencies are paid when the physicians/nurses they enter into the database are matched to a hospital. To make sure that their providers get first dibs, they may leave out information, misrepresent availability, and in extreme cases, even falsify certification statuses. These errors are often caught during the hospital credentialing process, which results in many hours of wasted time on the part of internal credentialing personnel, and delays in filling the position. In other cases, the errors are not caught during credentialing and legal problems ensue when impaired providers are hired accidentally.
2. Limitation of choice. The non-compete contracts associated with VMS systems typically prevent hospital physician recruiters from contacting staffing agencies directly to fill their needs. This forces the hospital to rely on the database for all staffing leads. At least 68% of staffing agencies do not participate with VMS systems, so a large portion of the most carefully vetted professionals remain outside the VMS, inaccessible to those who contracted to use it.
3. Extra hospital employee training required. There are hundreds of proprietary VMS systems in use. Each one requires specialized training to manage everything from durable medical equipment to short term surgical staff. In cases where hospital staff are spread too thin to master this training, some VMS companies are pleased to provide a “managed service provider” or MSP to outsource the entire recruitment process. This adds additional layers, further removing the hospital recruiter from the physician.
4. Providers hate VMS systems. As anyone who has read a recent nursing blog can attest, VMS systems are universally despised by the potential employees they represent. VMS paints professionals in black and white, without the ability to distinguish quality, personality, or perform careful reference checks. They force down salaries, may rule out candidates based on where they live (travel costs), and provide no opportunity to negotiate salary vis-a-vis work load. When a hospital opts to use a VMS system as a middle man between them and the staffing agencies, the agencies often pass along the cost to the providers by offering them a lower hourly rate.
5. Provider privacy may be compromised. Once a physician or nurse curriculum vitae (CV) is entered into the VMS database the agency recruiter who entered it has 1 year (I can’t confirm that this is true for all systems) to represent them exclusively. After that, the CV is often available for any recruiter who has access to that VMS to view or pitch to any client. There is a wide variety of agency quality in the healthcare staffing industry, with some being highly ethical and selective in choosing their clients (only quality hospitals) and providers (carefully screened). Others are transactional, bottom-feeders with all the scruples of a used car salesman. When your data is in a VMS, one minute you might be represented by a caring, thoughtful recruiter who understands and respects your career needs, and the next (without your informed consent) you’ll be matched to a bankrupt hospital undergoing investigation by the Department of Health by a gum-chewing salesman who threatens you with a lawsuit if you don’t complete an assignment for half the pay you usually receive.
6. No cost savings, only increased liability. In the end, some hospitals who have tried VMS systems say that their decreased hiring costs have not resulted in overall savings. While they may see a downward shift in salary paid to their temporary work force, they get what they pay for. Just one “bad hire” who causes a medical malpractice lawsuit can eat up salary savings for an entire year of VMS. Not to mention the increased costs associated with a slower hiring process, attrition from poor fits, and the inconvenience of having to re-recruit for positions over and over again. Providers also lose out on career opportunities while they’re “on hold” during a prolonged hiring process. And for those who layer on a MSP, they lose control of the most important hospital quality and safety line of defense – choosing your own doctors and nurses.
In summary, while the idea of using a software matching service for recruiting physicians and nurses to hospitals sounds appealing at first, the bottom line is that reducing care providers to a group of numerical fields removes all the critical nuance from the hiring process. VMS, with their burdensome non-competes, cumbersome technology, and lack of quality control are an unwelcome new middle man in the healthcare staffing environment. It is my hope that they will be squeezed out of the business based on their own inability to provide value to a healthcare system that craves and rewards quality and excellence in its staff.
Job matching requires thoughtful hospital recruiters in partnership with ethical, experienced agencies. Choosing one’s hospital gauze vendor should involve a different selection algorithm than hiring a new chief of surgery. It’s time for physician and nurse groups to take a stand against this VMS-inspired commoditization of medicine before its roots sink in too deeply and we all become mere line items on a hospital vendor list. So next time you doctors and nurses plan to work a temporary assignment, ask your recruiter if they use a VMS system. Avoiding those agencies who do may mean a much better (and higher paying) work experience.
*Locum tenens (filling hospital staffing needs with part time or traveling physicians and nurses) is big business. Here is a run down of the estimated market size and its key industry leaders (provided by CompHealth):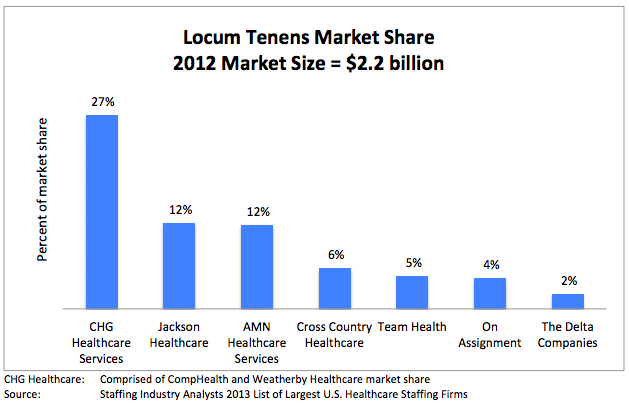
May 5th, 2014 by Dr. Val Jones in Expert Interviews, Health Policy, Opinion
1 Comment »
 It’s no secret that most physicians are unhappy with the way things are going in healthcare. Surveys report high levels of job dissatisfaction, “burn out” and even suicide. In fact, some believe that up to a third of the US physician work force is planning to leave the profession in the next 3 years – an alarming statistic.
It’s no secret that most physicians are unhappy with the way things are going in healthcare. Surveys report high levels of job dissatisfaction, “burn out” and even suicide. In fact, some believe that up to a third of the US physician work force is planning to leave the profession in the next 3 years – an alarming statistic.
Direct primary care practices are touted as the best way to restore patient and provider satisfaction. Those brave enough to cut out the “middle man” (i.e. health insurers, both public and private) find a remarkable reduction in billing paperwork, unrecovered fees, and electronic documentation requirements. I know many physicians who have made the switch and are extremely happy to be able to spend most of their time in direct patient care, unfettered by most rules, regulations, and coding systems. They can solve problems via phone, email, text, video chat, or in-office as the need arises without having to worry about whether or not their manner of interaction will be reimbursed.
Direct primary care is probably the best way to find freedom and happiness in practicing outpatient medicine. But where does that leave physicians who are tied to hospital care due to the nature of their specialty (surgeons, intensivists, anesthesiologists, etc.)? Is there any way for them to find a brighter way forward?
I have found that working as a locum tenens hospital-based physician has dramatically improved my work satisfaction, and it may do so for you too. Here’s why:
1. You can take as much time off as you want, anytime you want. Do not underestimate the power of frequent vacations on your mental health. The frenetic pace of the hospital is much more tolerable in short doses. My attitude, stamina, and ability to stay focused is dramatically improved by working only 2-3 week stretches at a time. When I feel good, I can spread the cheerfulness, and I am happy to spend longer hours at work to give my patients more of my time.
2. You can avoid most political drama. Hospitals are incredibly stressful environments filled with hierarchical and territorial land mines. Being a short-timer allows you to avoid many conflicts. Administrators never nag you, or hold you responsible for perceived departmental deficiencies. You don’t need to attend committee meetings or become involved in personality quirk arbitrage. You can stay above the fray, focusing purely on the patients.
3. You learn all kinds of new things. Exposure to different patient populations, hospital expertise and different peer groups exposes you to a broader swath of technology and humanity. No longer will you be tied to the regional practice idiosyncrasies of a single hospital – you’ll learn how to tackle problems from many different angles. That knowledge earns you respect, and serves to cross-pollinate your own specialty, making you – and those you learn from – better doctors.
4. You are free to leave. There’s something refreshing about knowing that you can leave a place that you don’t like without any repercussions. No matter how unpleasant a locums assignment, it will end, and you can saunter off to brighter pastures.
5. You make more money. Believe it or not, locums work can be quite lucrative if you find the right assignments. I know a team of hospitalists who travel the country together, negotiating higher rates since they are a “one stop” solution. Their housing, travel, and cars are paid for by the agency, and they have take home pay (before taxes) around $350K per year. I personally think that working that many hours as a locum tenens physician kind of defeats the purpose of avoiding burn out, but some people like to do it that way.
6. You can live in the warm states in the winter, and the cold ones in the summer. Enough said.
7. You can try before you buy. Maybe you’re not sure where you want to sink down career roots. Or maybe you’re not sure you’ll like living in a certain city or part of the world? Maybe your family isn’t sure they want to move to a new location? Locum tenens assignments are the perfect way to try before you buy.
8. You can use your experience to become an excellent consultant. With long term exposure to various hospital systems, you are in a unique position to develop an encyclopedic knowledge of best practices. Sharing how other hospitals have solved their challenges can spark reform at other institutions. You can become a real force for positive change, not just on a micro level, but system and state-wide.
Working as a locum tenens physician may enhance your career satisfaction and promote professional advancement. What it will not solve, however, is the following:
1. You still have to work within the framework of bureaucracy endemic to hospitals. You’ll need to learn to use multiple different EMR systems and fill out most of the same paperwork that you do as a full-timer. This is painful at first, but once you’ve mastered the most common EMR systems (I’ve only really encountered 5 different ones in 2 years of locum tenens work) you’ll find a clinical rhythm that fits into most frameworks.
2. You will be living out of a suitcase. If the disruption of frequent travel is too much for you (or your family) to bear, then perhaps the locums lifestyle is not for you.
3. You will be annoyed by the process of getting multiple medical licenses and hospital credentialing. Agencies try to help with this burden, but mostly, you’ll need to suffer through this part yourself.
4. You will have to live with some degree of uncertainty. Part of the nature of working as a locum tenens physician is that clients (hospitals) change their minds frequently. They try to fill open positions with local staff or hire additional full-timers, using locums as their more expensive back ups. Assignments fall through frequently, so you’ll need to be ready to change course quickly.
Overall, I believe that locum tenens work can provide the practice freedom that many hospital-based physicians crave. If you’re eager to get off the unrelenting clinical treadmill, this is an easy way to do it. At a recent assignment near New Hampshire, I mused at the license plates that I passed on my way to work: “Live free or die” is their state motto. And I think it captures my sentiments exactly.
August 15th, 2013 by Dr. Val Jones in Health Policy, Opinion
No Comments »
 As I travel around the country, working in the trenches of various hospitals, I’ve been struck by the number of errors made by physicians and nurses whose administrative burden distracts them from patient care. The clinicians who make the errors are intelligent and competent – and they feel badly when an error is made. However, the volume of tasks required of them in a day (many of which are designed to fulfill an administrative “patient safety” or “quality enhancement” process) makes it impossible for them to complete any task in a comprehensive and thoughtful manner. In the end, administrators’ responses to increased error frequency is to increase error tracking and demand further documentation that leads to less time with patients and more errors overall. It’s a vicious cycle that people aren’t talking about enough.
As I travel around the country, working in the trenches of various hospitals, I’ve been struck by the number of errors made by physicians and nurses whose administrative burden distracts them from patient care. The clinicians who make the errors are intelligent and competent – and they feel badly when an error is made. However, the volume of tasks required of them in a day (many of which are designed to fulfill an administrative “patient safety” or “quality enhancement” process) makes it impossible for them to complete any task in a comprehensive and thoughtful manner. In the end, administrators’ responses to increased error frequency is to increase error tracking and demand further documentation that leads to less time with patients and more errors overall. It’s a vicious cycle that people aren’t talking about enough.
As I receive patient admissions from various referral hospitals, I rarely find a comprehensive discharge summary or full history and physical exam document that provides an accurate and complete account of the patient’s health status. Most of the documentation is poorly synthesized, scattered throughout reams of EMR-generated duplicative and irrelevant minutiae. Interpreting and sifting through this electronic data adds hours to my work day. Most physicians don’t bother to sift – which is why important information is missed in the mad dash to treat more patients per day than can be done safely and thoroughly.
I have personally witnessed many critical misdiagnoses caused by sloppy and rushed medical evaluations. I have had to transfer patients back to their originating surgical hospitals (at some of America’s top academic centers) for further work up and treatment, and have uncovered everything from cancer to brain disorders to medication errors for patients who had been evaluated and treated by many other specialists before me. No one seems to have the time to take a long hard look at these patients, and so they end up undergoing knee-jerk treatments for partially thought through diagnoses. The quality of medical care in which I’ve been engaged (over the past 20 years) has taken a dramatic turn for the worse because of volume overload (fueled by diminishing reimbursement) in the setting of excessive administrative and documentation requirements.
To use an analogy – The solution to the healthcare cost crisis is not to increase the speed of the assembly line belt when our physicians and nurses are already dropping items on the floor. First, stop asking them to step away from the belt to do other things. Second, put a cap on belt speed. Third, insure that you have sufficient staff to handle the volume of “product” on the belt, and support them with post-belt packaging and procedures that will prevent back up.
What we require most in healthcare is time to process our thoughts and engage in information synthesis. We must give physicians the time they need to complete a full, comprehensive, evaluation of each patient at regular intervals. We need nurses to be freed from desk clerk and safety documentation activities to actually inspect and manage their patients and alert physicians to new information.
Until hospitals and administrators recognize that more data does not result in better care, and that intelligent information synthesis (which requires clinician time, not computer algorithms) is the foundation of error prevention, I do not foresee a bright future for patients in this manic assembly line of a healthcare system.
May 2nd, 2013 by Dr. Val Jones in Health Tips, Opinion, Research
No Comments »
 A recent, 358-person survey conducted by researchers at Yale University (and published in the International Journal of Obesity) suggested that patients may be less likely to follow the medical advice of overweight and obese physicians. Survey respondents were 57% female, 70% Caucasian, 51% had BMIs in the normal or underweight category (31% overweight and 17% obese), and were an average age of 37 years old.
A recent, 358-person survey conducted by researchers at Yale University (and published in the International Journal of Obesity) suggested that patients may be less likely to follow the medical advice of overweight and obese physicians. Survey respondents were 57% female, 70% Caucasian, 51% had BMIs in the normal or underweight category (31% overweight and 17% obese), and were an average age of 37 years old.
Respondents rated overweight and obese physicians as less credible than normal weight doctors, and stated that they would be less likely to follow advice (including guidance about diet, exercise, smoking cessation, preventive health screenings, and medication compliance) from such physicians. Although credibility and trust scores differed between the hypothetical overweight and obese providers and normal weight colleagues, the respondents predicted less of a difference between them in terms of empathy and bedside manner. Respondents said they’d be more likely to switch physicians based on their weight alone. There was no less bias against overweight and obese physicians found in respondents who were themselves overweight or obese.
The study authors note that this survey is the first of its kind – assessing potential weight bias against physicians by patients of different weights. Previous studies (by Puhl, Heuer, and others) have documented weight bias against patients by physicians.
While the study has some significant limitations (such as the respondents being disproportionately Caucasian, thin, and female), I think it raises some interesting questions about weight bias and physicians’ ability to influence patients to adopt healthier lifestyles.
Considering the expansion of pay-for-performance measures (where physicians receive higher compensation from Medicare/Medicaid when their patients achieve certain health goals -such as improved blood sugar levels), being overweight or obese could reduce practice profit margins. If patients are less likely to follow advice from overweight or obese doctors, then it stands to reason that patients’ health outcomes could suffer along with the doctors’ income.
I’m certainly not suggesting that CMS monitor physician waist circumferences in an attempt to improve patient compliance with healthy lifestyle choices (Oh no, did I just give the bureaucrats a new regulatory idea?), but rather that physicians redouble their efforts to practice what they preach as part of a commitment to being good clinicians.
Some will say that the problem here is not expanding provider waistlines, but bias against the overweight and obese. While I agree that weight has little to do with intellectual competence, it does have to do with disease risk. Normalizing and destigmatizing unhealthiness is not the way to solve the weight bias problem. We know instinctively that carrying around a lot of extra pounds is damaging to our health. It’s important to show grace and kindness to one another as we join together on the same health journey – a struggle to make good lifestyle choices in a challenging environment that tempts us to eat poorly and cease exercising.
To doctors I say, let’s fight the good fight and model healthy behaviors to our patients. To patients I say, show grace to your doctors who carry extra pounds – don’t assume that they are less competent or knowledgeable because of a weight problem. And to thin, female, 30-something, Caucasian survey respondents I say – Wait till you hit menopause before you judge people who are overweight! 😉
January 5th, 2012 by DavidHarlow in Health Policy, Opinion
No Comments »

There are at least two conversations going on in the health care marketplace today, each focused on one of two key questions. One is: How can we achieve the Triple Aim? The other is: Why do they get to do that? (It’s not fair! I want more!)
Until we stop asking the second question, we can’t answer the first question. Why? Because all too often the answer to the second question is the equivalent of: It’s OK, Timmy, I’ll buy you TWO lollipops; pick whichever ones you want.
It’s the tragedy of the commons, transposed to the health care marketplace.
Recent cases in point:
- Avastin
- Tufts Medical Center – Blue Cross Blue Shield of Massachusetts grudge match
- Mammography and PSA guidelines
1. Avastin. Late last year, Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
 In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.
In an effort to save on human resources costs, some hospitals have decided to make locum tenens* doctors and nurses line items in a supply list. Next to IV tubing, liquid nutritional supplements and anti-bacterial wipes you’ll find slots for nurses, surgeons, and hospitalist positions. This depressing commoditization of professional staffing is a new trend in healthcare promoted by software companies promising to solve staffing shortages with vendor management systems (VMS). In reality, they are removing the careful provider recruiting process from job matching, causing a “race to the bottom” in care quality. Instead of filling a staff position with the most qualified candidates with a proven track record of excellent bedside manner and evidence-based practice, physicians and nurses with the lowest salary requirements are simply booked for work.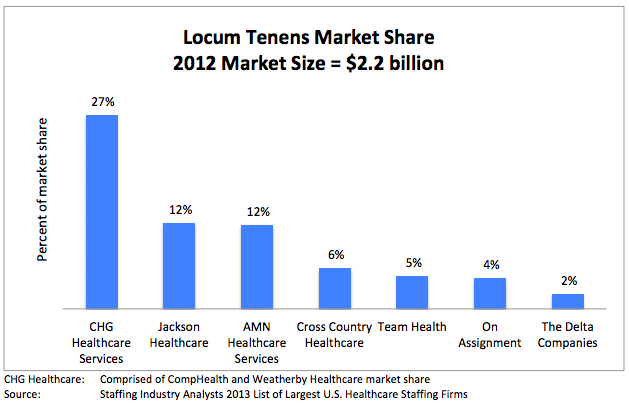


 It’s no secret that most
It’s no secret that most  As I
As I











