November 30th, 2011 by StevenWilkinsMPH in Opinion
1 Comment »

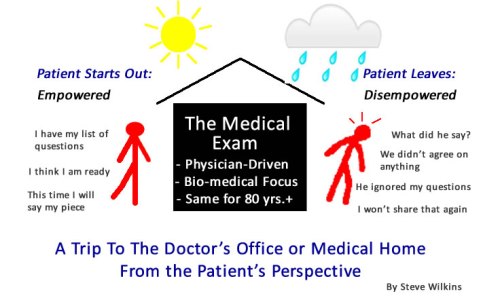
I may not know how to tell the difference between an empowered patient, an engaged patient, or an activated patient. But I do know that the fastest way to disempower, disengage, and de-activate any patient is a trip to the doctor’s office or the hospital. A visit to an average primary care physician (or specialist) is to an empowered/activated/engaged patient what Kryptonite is to Superman. It will stop all but the strongest willed patients dead in their tracks.
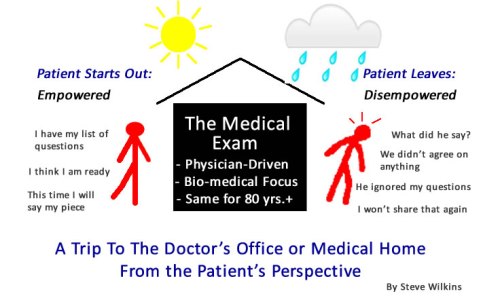 We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
Things haven’t changed much in the 40 years since I was a kid sitting in Dr. Adam’s office. Read more »
*This blog post was originally published at Mind The Gap*
November 18th, 2011 by StevenWilkinsMPH in Opinion, Research
No Comments »


Abraham Verghese, MD, Standford University
My wife has two world-class oncologists who help her manage her Stage 4 Lung Cancer. Both are excellent clinicians. Yet their skills differ in one very important way. Her radiation oncologist physically touches her a lot (in a good way of course!). There are the touches on her arm, a hand on the shoulder, hugs, and of course a thorough hands-on physician exam. Her medical oncologist not so much.
We all recognize the therapeutic value of touch. Dr. Abraham Verghese, a Stanford Physician and Professor, at the 2011 Med2.0 Conference, described the power of touch associated with the physical exam. In the following scenario he describes an interaction with a chronic fatigue patient who came to him after being seen by many other physicians: Read more »
*This blog post was originally published at Mind The Gap*
October 27th, 2011 by StevenWilkinsMPH in Opinion
No Comments »

Health care professionals are a cynical lot. We joke about the “fad or buzz word of the month”…usually some vague concept heralded by the powers on high. Our job is to promote the idea…knowing full well that the “next big thing” is probably right around the corner.
Take “Patient-Centered”…it sure feels like a buzz word. I suspect most hospital and physician executives, and their ad agency partners, would agree. But this time things are very different.
Why Hospitals and Physicians Should Get Serious About Patient-Centered Care
Reason #1 – Patients Are Starting To Discover That Their Doctors & Hospitals Are Read more »
*This blog post was originally published at Mind The Gap*
October 6th, 2011 by StevenWilkinsMPH in Opinion
No Comments »

Irrational exuberance was a term once used to describe the stock market before the last crash. It also seems an apt description for much of the talk these days about empowered health consumers.

To be sure, patients today have unprecedented access to health information. Patient decision-support tool can be found on just about every provider, payer and self-insured employer website. Consumers can go to any number of websites to find quality data about hospitals, physicians and health plans. Personal health records (PHRs) promise to make our personal health data portable for meaning that all our treating physicians will be “singing off the same song sheet.”
That’s what the industry experts tell us. But what’s really going on? Here I will describe what I see as the top 5 myths about empowered health consumers. Read more »
*This blog post was originally published at Mind The Gap*
September 27th, 2011 by StevenWilkinsMPH in Research
2 Comments »

Turns out there is an unintended consequence of many of the current efforts to standardize the way doctor’s practice medicine. It is called de-skilling. De-skilling can occur when physicians and other providers try to adapt to standardized, new ways of doing things. Examples of such standardization include clinical based care guidelines, electronic medical records (EMRs), Pay for Performance (P4P), Patient Centered Medical Home (PCMH) requirements and so on.
Examples of physician de-skilling were revealed in a recent study which consisted of in-depth interviews with 78 primary care physicians regarding EMR use. EMRs are all about standardization – what data is captured and recorded, how data is reported, how data is used, and so on.
Over the course of the interviews, physicians in the study described significant examples of de-skilling behavior. Most indicated that Read more »
*This blog post was originally published at Mind The Gap*
 We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…
We patients have been socialized that way. Think about your earliest memories of “going to the doctor.” For me, I remember my Mom taking me to the Pediatrician. Early on I learned by watching the interaction between my Mom and the doctor that they each had a role. The doctor’s role was that of expert – he spoke and my Mom listened. I was there just to have one or more extremities twisted and prodded. And oh the medicinal smell…












