June 28th, 2009 by Bongi in Better Health Network, True Stories
Tags: Anger, Anger Management, Chemo, Residency, Surgery
No Comments »

 In the old days sometimes confrontation was the only way to get things done. But sometimes anger lead one into useless and unnecessary confrontation. I recently spent some time with my old friend, swimmer’s chest and a story came to mind when that swimmer’s chest saved me from my own anger.
In the old days sometimes confrontation was the only way to get things done. But sometimes anger lead one into useless and unnecessary confrontation. I recently spent some time with my old friend, swimmer’s chest and a story came to mind when that swimmer’s chest saved me from my own anger.
We were on call together. Quite early in the day the chemotherapist called me. He had apparently put a patient on the emergency list the previous day for a portacath and the case didn’t get done. This was due to the fact that the emergency list first did critical cases like actively bleeding patients before they did relatively stable patients. Something like a portacath would tend to get shifted down the list and may even stand over to the next day. This is what had happened here. He now wanted me to do the case.
“Sure I’ll do it” I said. “As long as it’s on the list as soon as it comes up I’ll be there.”
“I want it done now!” he retorted. I was not impressed.
“Well phone the anaesthetist on call and motivate for him to move it up the list.” I said helpfully.
“That is not my job! You will do that!”
It was clear we had a communication problem. Whenever I had a telephonic communication problem I would put down the phone and take the effort to go to the relevant person to sort it out face to face. Not only does it help to speak things out in person but the walk usually gave me time to calm down (there was more than enough residual anger in those old days to go around). This is what I did here. I turned to swimmer’s chest and told him to accompany me. Off we set at speed.
We walked into the chemotherapy ward and asked to see the relevant doctor. Soon he was there in front of me. swimmer’s chest hung back. I introduced myself and explained that I was more than willing to do the surgery but I had no control over the order of the list. That was entirely in the hands of the anaesthetists. If he felt the case needed to be done before the other cases on the emergency list then he should phone the anaesthetist and discuss it with him.
“You will phone the anaesthetist yourself and you will do this case right now!” he said.
I could feel my anger slowly turning into fury.
“No! you will!” as I said it I clenched my fists and took a step towards him. Swimmer’s chest realised things were on the verge of going south. He later told me he thought I was going to punch the guy. I denied this, but the thought was going through my mind at the time, I confess.
So my good friend stepped in front of me with his broad chest and nudged me backwards. He then started speaking to the chemo doc in a calm diplomatic voice. He also subtly and slowly (almost so one didn’t notice) ushered the guy further and further away from me. By the end of it we left with the chemo guy feeling that we were there for him and would do all we could. I don’t think he even had an idea of how enraged he had made me.
Walking away swimmer’s chest asked me if I was mad. I had only a few month’s of training left and something stupid like getting into a fight was just about all that could stand in the way of me becoming a surgeon.
Those times in the end brought out the worst in me. By the end of my studies I knew I needed to get away from it all. I had very nearly become something I did not like. After leaving pretoria I gradually rediscovered the true me again. It was still there to my relief.

*This blog post was originally published at other things amanzi*
June 26th, 2009 by scanman in Better Health Network, True Stories
Tags: Death, ICU, MVA, Radiology, Surgery, Trauma, Ultrasound
2 Comments »

…
I was called to do an urgent bedside ultrasound scan of the abdomen for a trauma victim.
The patient was a young man of twenty-four who had been involved in a road traffic accident (RTA = MVA in US medical terminology). He had been brought – without any kind of basic life support – after sustaining a major trauma at a village about two hours away. The intensivist in the ICU told me that he was in severe hypovolemic shock on admission with a GCS of 4. Preliminary examination and radiographs had shown a comminuted fracture of the right femur (thigh bone) with a large hematoma and some facial bone fractures. After initial assessment and resuscitation in the casualty, a CT scan was done. He had a fracture in the frontal bone and a few small contusions in the brain, that raised the possibility of Diffuse Axonal Injury, nothing that could explain a GCS of 4 though. The assumption was that it was all due to extensive blood loss and hypovolemia. He was shifted straight to the ICU after the CT scan and I was called to do an ultrasound scan to check for hemoperitoneum (ie, abdominal injury and blood loss).
The scan was normal. As I was doing the scan, the intensivist was busy trying to put in a Subclavian central line. He secured the line just as I finished my scan, which incidentally was normal. As I was stepping away from the bed, the patient had a cardiac arrest, as evidenced by sudden bradycardia on the monitor. I moved out of the way as the intensivist, orthopaedic surgeon and ICU nurses went through a full resuscitation protocol. After a while, even I realized that it seemed like a futile exercise.
I was not particularly busy, so I peeped into to the Cardiac ICU next door as there seemed to be some commotion there. My cardiologist colleague, a normally friendly soul was peering intently at a very fast heart rhythm on a monitor over the bed of a young girl of about six or seven. There were a couple of nurses injecting something slowly into an intravenous cannula in the kid’s forearm. In passing, I noted that the kid was very calm and seemed very interested in what the nurse was doing. I stepped close to my friend and asked what was up. He turned, gave me a quick nervous smile and said he was trying to revert an SVT (supraventricular tachycardia, a very nasty fast heart rhythm). Honestly, I had never seen an SVT in someone so young, so I asked him what was the history. He told me the kid was brought by her mother to his outpatient clinic a short while ago because she complained of palpitations (I forgot the exact description used by the kid, but it was quite descriptive). My friend said he was sure it was an SVT after a quick examination in the clinic, so he rushed the kid upstairs to the Cardiac ICU, connected her to a monitor, confirmed the diagnosis and had ordered Adenosine IV stat for reversal. He maintained his intent survey of the monitor as he recounted the story and the nurse continued her slow IV injection. At one particular point when the line on the monitor became particularly squiggly, he shouted, “STOP!” and the nurse stopped injecting.
…
It was almost magical.
…
The squiggles became a recognizable cardiac rhythm, albeit very fast – about 160 to 170 beats per minute. My friend called out to one of the superfluous nursing attendants and asked them to get the kid’s mother inside. A very anxious young lady who had obviously been weeping was led in. My friend showed her the monitor and explained to her that the nasty rhythm had been made to behave itself or something to that effect and told her that the kid was out of any imminent danger.
Happy with the positive outcome, I strolled out to be confronted by a wailing family, including two young girls, maybe a year or two older than the calm kid inside, who had just been told that their older brother who fell off his motorbike was dead.
It was past my work hours. I went out and had a drink and reflected.
Such is life.
…
*This blog post was originally published at scan man's notes*
June 24th, 2009 by Emergiblog in Better Health Network, True Stories
Tags: Emergency Medicine, Nursing, Patient Care, Shifts
No Comments »

 Well, somebody likes their job, I must say.
Well, somebody likes their job, I must say.
Although I can’t figure out why she is smiling.
Her cap looks like conjoined coffee filters!
Conjoined coffee filters that somebody sat on!
Maybe she doesn’t realize it’s squished, and would die of embarrassment if she knew!
********************
The emergency department “regular”.
Every emergency department has them.
A patient can become a “regular” for many reasons. Maybe they are a recurrent cardiac patient. Perhaps they suffer from chronic pain. Sometimes, they become a “regular” because they utilize the ER as a clinic and bring the whole family in over the course of a month. Some regulars are drug seekers. Others are homeless and know they can find respite in the department for at least a couple of hours and maybe get something to eat.
If you work in an emergency department long enough, you will know who they are.
And you will get to know them.
*****
Recently, it dawned on me just how well you get to know them.
I work in a community hospital. It’s one of those hospitals that patients actually request to go to from all over the county. We have our shifts from hell, but it is far from the county-trauma-eight-hour-wait-time environment of the huge medical centers. There is time to talk to the patients, find out more about them than what hurts, what is swollen or what prescription they have lost.
Over time, the conversation stops being scripted and “starts getting real”, as they say.
*****
This particular shift was steady, but not crazy. And almost all the patients I cared for were “regulars”. Easily 90%. For some, it was their usual health issue. For others, something different.
I found out a lot that night over the course of that shift
Someone’s youngest would be starting kindergarten in September; someone’s oldest had just graduated from high school. Someone had gotten into a recovery program and had been clean for a month. Someone had just welcomed their first grandchild, another was mourning the loss of their mom the week before. Someone had lost their job earlier in the week. Someone had gotten married since their last visit. A baby sister was on the way for one of my patients. Another patient had enrolled in the local junior college.
We saw them, treated them and sent them on their way with a wave and a prescription.
Hopefully they left in better shape then they arrived, even if all they needed was reassurance.
All I know is that I thoroughly enjoyed that shift.
*****
I had done all the usual things. Saline locks, blood draws. Medications and re-evaluations. IVs and education.
But I had also congratulated success, commiserated over frustrations and offered consolation over losses. We covered birth and death, struggles and successes, dropping old lifestyles and starting new beginnings.
That shift, I saw my patients in a different light.
*****
The best part of nursing has nothing to do with disease or diagnoses or procedures or prescriptions.
The best part of nursing is the patients themselves.
I thoroughly enjoyed catching up with my “regulars”.
I hope I was therapeutic for them.
They were most certainly therapeutic for me.
*This blog post was originally published at Emergiblog*
June 23rd, 2009 by KerriSparling in Better Health Network, True Stories
Tags: Diabetes, Endocrinology, Pediatrics, Type 1 Diabetes
No Comments »

I saw my niece over the weekend. She just turned seven. She had a bit of a fever and wasn’t feeling very well, so when I saw her snuggled up on the couch under a blanket, she looked every bit the little kid she is. Poor little peanut, hiding out until she felt better.
I remembered that I was about her age when I was diagnosed.
I found an old school photo from second grade, with me sitting next to my friend Bobby (who I still talk to, which is a very surreal experience, hanging out with someone I’ve known longer than I’ve known insulin injections). I was diagnosed in September, right as second grade started.
I’m in the blue dress, second row from the bottom, third from the left.
Swinging my feet. Not much for sitting still, even in second grade.
Over the last few days, I’ve been reading some emails from the CWD parents as they gear up for the Friends for Life conference in Orlando in a few weeks. These emails are sent out to a whole mailing list of attendees, and somehow I ended up on the list with all the parents. (Or maybe the list just happens to be mostly parents and I just happen to be an adult “kid” with diabetes.) These parents are comparing notes and reaching out to one another, looking forward to other parents who understand what they’re going through every day as they care for their kid with diabetes.
And I wish that my mother had this kind of support when she was dealing with my diagnosis over twenty years ago. My mom had a lackluster team of doctors at the Rhode Island Hospital (where I went for a few months before going to Joslin) and Eleanor (the only other mother of a diabetic kid that we knew of in our town and the woman who just happens to be my local Dexcom rep), leaving her with little to manage the enormous learning curve.
This weekend, I went on a bike ride with my sister-in-law, my father-in-law, and my husband. I had to remember to test beforehand, bring my meter, stash some glucose sources on several people, and monitor as re rode. A lot of thought for maybe an hour long bike ride. And it made me wonder what kind of preparation and worry my mother went through when she sent me out to play for a whole Saturday afternoon. Lot of work on my mom’s part just to keep things normal.
I forget this sometimes, how many people are really involved in keeping me healthy.
I need to call my mom.
(Granted, my diabetes diagnosis hasn’t kept me from doing much at all. And it definitely didn’t keep me from being … um, a bit of a goofball.)
*This blog post was originally published at Six Until Me.*
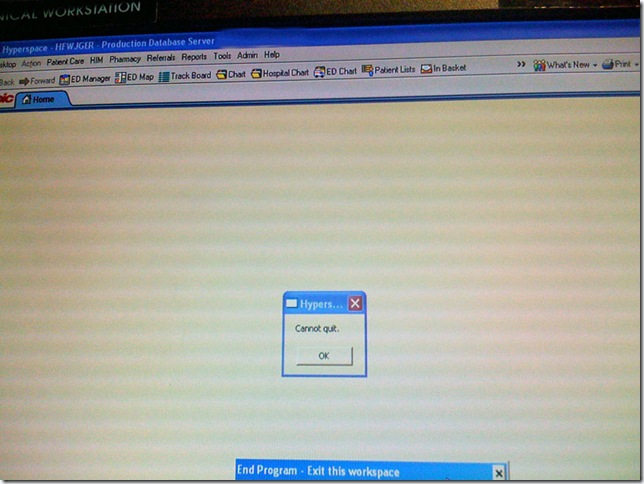
June 21st, 2009 by GruntDoc in Better Health Network, Humor, True Stories
Tags: Crash, Electronic Medical Record, EMR, Error Message, System Failure
No Comments »

Even when it crashes:
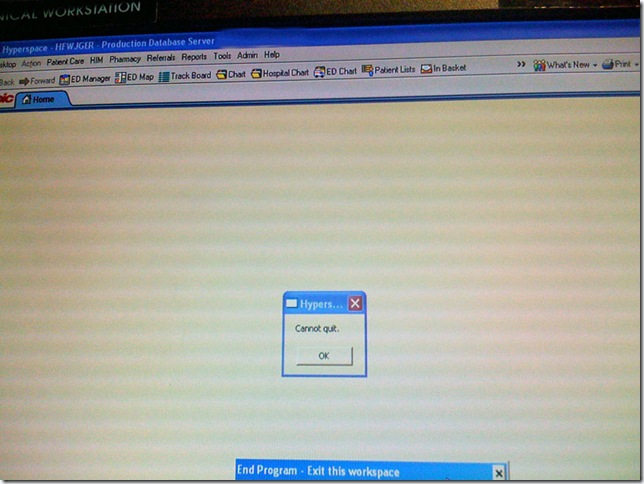 (it says “Cannot Quit”).
(it says “Cannot Quit”).
*This blog post was originally published at GruntDoc*
 In the old days sometimes confrontation was the only way to get things done. But sometimes anger lead one into useless and unnecessary confrontation. I recently spent some time with my old friend, swimmer’s chest and a story came to mind when that swimmer’s chest saved me from my own anger.
In the old days sometimes confrontation was the only way to get things done. But sometimes anger lead one into useless and unnecessary confrontation. I recently spent some time with my old friend, swimmer’s chest and a story came to mind when that swimmer’s chest saved me from my own anger.





 Well, somebody likes their job, I must say.
Well, somebody likes their job, I must say.