December 9th, 2013 by Dr. Val Jones in Opinion, True Stories
Tags: Acute Inpatient Rehab, anorexia, Downward Spiral, Ex-military, Infection, Motivation, Patient Autonomy, Physical Medicine And Rehabilitation, Physical Therapy, Police Officers, Psychiatry, rehab, Stubbornness, Veterans, Wives
1 Comment »
 Over the years that I’ve worked in acute inpatient rehab centers, I have been truly vexed by a particular type of patient. Namely, the stubborn patient (usually an elderly gentleman with a military or armed forces background). I know that it’s not completely fair to generalize about personality types, but it seems that the very nature of their work has either developed in them a steely resolve, or they were attracted to their profession because they possessed the right temperament for it. Either way, when they arrive in the rehab unit after some type of acute illness or traumatic event, it is very challenging to cajole them into health. I suspect that I am failing quite miserably at it, frankly.
Over the years that I’ve worked in acute inpatient rehab centers, I have been truly vexed by a particular type of patient. Namely, the stubborn patient (usually an elderly gentleman with a military or armed forces background). I know that it’s not completely fair to generalize about personality types, but it seems that the very nature of their work has either developed in them a steely resolve, or they were attracted to their profession because they possessed the right temperament for it. Either way, when they arrive in the rehab unit after some type of acute illness or traumatic event, it is very challenging to cajole them into health. I suspect that I am failing quite miserably at it, frankly.
Nothing is more depressing for a rehab physician than to see a patient decline because they refuse to participate in activities that are bound to improve their condition. Prolonged immobility is a recipe for disaster, especially in the frail elderly. Refusal to eat and get out of bed regularly can make the difference between life and death within a matter of days as leg clots begin to form, and infectious diseases take hold of a body in a weakened state. The downward spiral of illness and debility is familiar to all physicians, but is particularly disappointing when the underlying cause appears to be patient stubbornness.
Of course, the patient may not be well enough to grasp the “big picture” consequences of their decisions. And I certainly do not pretend to understand what it feels like to be elderly and at the end of my rope in regards to prolonged hospital stays. Maybe I’d want to give up and be left alone too. But it’s my job to get them through the tough recovery period so they can go home and enjoy the highest quality of life possible. When faced with a patient in the “wet cat” phase of recovery (I say “wet cat” because they appear to be as pleased to be on the rehab unit as a cat is to being doused against their will), these are the usual stages that I go through:

1. I explain the factual reasons for their admission to rehab and what our goals are. I further describe the risks of not participating in therapies, eating/drinking, or learning the skills they need to care for themselves with their new impairments.
2. I let them know that I’m on their side. I understand that they don’t want to be here, and that I will work with them to get them home as soon as possible, but that I can’t in good conscience send them home until it’s safe to do so.
3. I give them a projected discharge date to strive towards, with specific tasks that need to be mastered. I try my best to give the patient as much control in his care as possible.
4. I ally with the family (especially their wives) to determine what motivates them, and request their presence at therapy sessions if that seems fruitful rather than distracting. (Helpful spouse input: “Mike only wants to walk with me by his side, not the therapist.”)
5. I ask loved ones how they think the patient is doing/feeling and if there is anything else I can do to make his stay more pleasant. (Helpful input: “John loves ice cream. He hates eggs” or “John usually goes to bed at 9pm and gets up at 4am every day.”)
6. I meet with nursing and therapy staff to discuss behavioral challenges and discuss approaches that are more effective in obtaining desired results. (For example, some patients will always opt out of a task if you give them a choice. However, they perform the task if you state with certainty that you are going to do it – such as getting out of bed. “Would you like to get out of bed now, Mr. Smith?” will almost certainly result in a resounding “No.” Followed perhaps by a dismissive hand wave. However, approaching with a “It’s time to get out of bed now, I’m helping you scoot to the edge of the bed and we’re going to stand up on 3. One, two, three!” Is much more effective.)
7. If all else fails and the patient is not responding to staff, loved ones, or doctors, I may ask for a psychiatric consult to determine whether or not the patient is clinically depressed or could benefit from a medication adjustment. Typically, these patients are vehemently opposed to psychiatric evaluation so this is almost the “nuclear” option. Psychiatrists can be very insightful regarding a patient’s mindset or barriers to participation, and can also help to tease out whether delirium versus dementia may be involved, and whether the patient lacks capacity to make decisions for himself.
8. If the patient still does not respond to further tweaks to our approach to therapy or medication regimen, then I begin looking for alternate discharge plans. Would he be happier in a skilled nursing home environment where he can recover at a slower rate? Would he be amenable to an assisted living or long term care facility? (The answer is almost always a resounding “no!”) Is the patient well enough to go home with home care services and round-the-clock supervision? Does the family have enough support and can they afford this option?
9. At this point, after exhausting all other avenues, if the patient is still declining to move or eat or be transferred elsewhere, some sort of infection might set in. A urinary tract infection, a pneumonia, or bowel infection perhaps. Then the patient becomes febrile, is started on antibiotics, becomes weaker and less responsive, and is transferred to the medicine floor or higher level of care. Alternatively at this phase (if he is lucky enough not to become infected) the patient might have a cardiac event, stroke, blood clot with pulmonary embolus (especially if he is a large man), kidney failure, or develop infected pressure ulcers. Any of which can be cause for transfer to medicine. In short, if you stay in the hospital long enough, you can find a way to die there.
10. After much hand-wringing, angst, and generalized feelings of helplessness the wives and I review the course of events and ask ourselves if we could have done anything differently. “If I had acted like a drill sergeant, do you think he would have responded better?” I might ask. “No dear, that would only have made things worse.” She’ll reply. I’ll see how disappointed she is in his deterioration, staring off towards pending widowhood, engaging in self-blame and what-ifs (E.g. “If we had only had more money perhaps we could have taken him home with 24 hour nursing care until he was better…” “If I had cooked all his meals, maybe he would have gained enough strength to avoid the infection…” etc.) I try to be reassuring that none of this would have made a difference, myself reeling from the failure to get the patient home.
This 10 step process happens far more often than I’d like, and I certainly wish there were a way to head off the downward spiral with some kind of effective intervention. Would it help to have a volunteer unit of ex-military peer counselors in the hospital who could visit with my patients and help to motivate them to get better? (Operation “wet cat” perhaps?) Should I change my approach and put on my drill sergeant hat at the earliest stages of recovery to force these guys out of bed? Can educating younger law enforcement and military workers about illness help to prepare them to be more compliant patients one day?
I don’t know the cure for stubbornness, but it sure leaves a lot of widows in its wake.
August 11th, 2013 by Dr. Val Jones in Opinion, True Stories
Tags: Advice, Clients, Hospitals, How To Negotiate With Locum Tenens Agencies, Internal Medicine, Locum Tenens, Physical Medicine And Rehabilitation, Primary Care, Tips For Physicians, Traveling Physician
No Comments »

On Assignment In California Vineyard
This post is the continuation of my personal thoughts and reflections about what it’s like to work as a Locum Tenens (traveling temp) physician.
Q: Where are the most favorable locums jobs?
This is an interesting question and depends a little bit upon personal taste and priorities. While most locums physicians choose their work based on location (see this nice survey of locum priorities), more experienced locums docs choose their work based on circumstance. What I mean is that it’s more important WHY the hospital needs you, than where the hospital is physically located. It only takes one really bad assignment to learn that lesson the hard way. For instance, if a hospital is recruiting a locum tenens physician because the place is so bad that no one will stay in the job, then I can pretty much guarantee that it won’t matter how nice the city/town/countryside is nearby, you will not enjoy your time there.
Positive prognostic indicators for a good locums assignment include:
1. The person you’re filling in for needs vacation coverage or are on maternity/paternity leave. They are happy with their job and are eager to come back.
2. The hospital is undergoing a growth phase and needs help staffing new wings/wards.
3. The hospital is operating in the black but happens to be in a rural area where it is challenging to find enough physicians to meet the patient needs.
Red flags:
1. The medical director/staff physician “doesn’t have time” to talk to you about the assignment before you commit to doing it.
2. There is more than a second-long pause when you ask the medical director why he/she would want to work there as a locums.
3. The person you’re filling in for was fired due to incompetence or negligence.
4. The person you’re filling in for is on the verge of a nervous break down from overwork, and a locums agency was called in to prevent implosion/explosion type scenarios.
5. There have been multiple staff (nursing usually) strikes at the hospital in the past 6 months.
7. The group with whom you would work is not culturally diverse – and you can imagine having difficulty gaining acceptance by them.
In my experience, you can enjoy living anywhere temporarily if the people and circumstances are pleasant. A nice post-work dinner/coffee with friendly, competent staff – even in a “backwater” setting – trumps a solo trip to a high end, big city restaurant when you are emotionally and mentally exhausted by the misery of a bad hospital. Trust me on this.
As one locums hospitalist put it: “Generally I’ve found the rural hospitals to be the nicest, especially in the midwest. But I’m never going back to South Dakota in the winter.”
Q: How can I negotiate the best salary?
First of all, you need to know that this is a negotiation. When I first started, I just assumed the salary I was offered required a binary response: “Yes, I’ll accept the position,” or “No I’ll keep looking for other opportunities.” That’s why I’m a physician and not a business woman, I guess! Just ask my husband.
Anyway, after a few experiences of getting paid a lower salary than my peers at the same job, I realized the error of my ways. In many cases you can lobby for up to 25% higher pay rate, so you should keep that in mind. In summary, here is where the salary “wiggle room” is:
1. How much overhead your agency charges. Remember the “platinum” agency I referred to in my last post? If you’re working with one of the agencies that is known to be “expensive” then they have more money that they could share with you. If you’re working with a budget agency who competes based on low overhead fees (such as 20% above your base salary rate), then you’ll never get more than $5-10 more/hour from them.
2. If you have a good track record. Once you’ve proven yourself to be an excellent physician, well-liked by the hospital staff where you’ve been assigned, the agency is going to want to keep sending you to new assignments because you’re more likely to get requests to return and will stay longer at each gig. The agency (and the recruiters) make money based on how many hours you bill, so they’d rather send a “sure thing” to a new client than an unknown. They will be more likely to up your salary to seal the deal, knowing they’ll probably get more hours with you in the long run.
3. How desperate the client/hospital is. This is sad to say, but desperate clients will pay higher rates to fill a need. If you’re being offered an unusually high salary for a certain assignment, don’t rejoice, worry (see notes above about “red flags.”)
4. If you bundle. Some enterprising primary care locums docs get together to negotiate group rates. That means, if you have a friend or two who can agree to travel together to a particular place, the agency can pay a higher salary to each of you because they’re getting a larger volume of hours overall. This works really well for internal medicine locums, for example, where hospitals often need multiple docs at a time. It’s actually a brilliant plan, because the people who do it are already sympatico, they have similar work ethics, can share call, sign out to each other, have built in friends to enjoy after work adventures, and arrive as a well-oiled machine. I think this is probably the future of primary care locums. However, if you’re like me (a specialist in a small field) there’s no way to bundle because no hospital ever needs more than one of you at a time. 😉
5. If you take longer assignments. This stands to reason. If you are going to be working for months (rather than weeks) at a certain hospital, then you have more room to negotiate a larger hourly rate based on the volume principle I described above.
Q: How do locums agencies decide how to match you with a given job opportunity?
Based on my experience, the agencies’ order of priorities for matching physicians with clients are:
1. Whoever is available and answers their phone first. The Locums world is very dog-eat-dog for the agencies. It’s a daily race to see who can present physicians to fill needs the fastest. Hospitals are looking for the lowest cost solution to their staffing gaps, and will shop multiple agencies for the same positions at once. The agency who brings the first acceptable C.V.s wins the work. Sometimes when there is controversy over which agency gets the job, the client has to review email time/date stamps to verify which came first. Sometimes it’s a matter of minutes. So… if your recruiter’s voice sounds a little tense, you’ll understand what’s going on in his/her world. And if you’re hungry for locums work, be sure to respond promptly for consideration. That being said, once you’ve established a track record with a few agencies, you’ll have turn away business year-round (especially in primary care).
2. Client preference. Once your C.V. has been presented to the client, they will choose their preferred candidate (if there is more than one option). Usually, they are looking for someone local or whomever will generate the lowest travel expenses. I wish that clients delved a little deeper than that, but my experience is that cost trumps coolness for them most of the time. And when I say “coolness” I mean – wouldn’t you rather have a candidate who writes well, has an unusual background (say – someone who has built medical websites and has been a food critic and cartoonist? Ahem?) than just another chem major straight out of IM residency? Apparently most would say no thanks. Just give me the cheaper one.
3. If they know and like you. Let’s say there are two equally qualified physicians for the same position already screened and signed up for work at a certain agency. If one of you has a track record of being flexible and easy to work with (rather than a demanding, entitled brat – like a few doctors you may know) then the recruiter will put the “nice” person’s CV on top and market you more strongly to the client. Why? Because she doesn’t want to receive whiny phone calls every other day during your assignment about how you don’t like the hospital food. The recruiters have “quality of life” issues too. If you’re lucky and you develop a good, long term relationship with your recruiter, they’ll probably even do YOU a favor and give you a head’s up about upcoming opportunities at the “good” hospitals. And we all know what that means.
4. Whoever will take the lowest hourly rate. In the end, it’s still all about the Benjamins so if there are 2 equally qualified physicians who are similarly “non whiny” then if one will work more days or at a lower rate, then they are more likely to get the job (due to recruiter influence on client preference). But given the large number of positions and the small number of locums to choose from, this game is 80% about who’s available first. Then the rest of the variables follow.
Q: What is the licensing and credentialing process like? How do I make it easier?
The state licensing and hospital credentialing is the most painful administrative part of the whole locum tenens assignment process. If you’re considering an opportunity in say, North Dakota, then you’ll need to get a state license there (Unless you already have one?) as well as passing the scrutiny of the rural hospital credentialing committee where you’ll be working. And yes, everyone seems to want original copies of the intern year you did 15 years ago at the hospital that has since closed. You feel my pain?
There is good news and bad news about this. The good news is that the Locums agencies have hired staff to complete the medical license and credentialing paperwork for you. That is part of the “value” they bring to you as an agency. The bad news is that some of their staff can’t spell. Or they get the chronological order of your residency/fellowship years wrong, etc. thus generating MORE work for you in the long run, correcting errors rather than filling in blanks.
The middle road is to fill out the paperwork correctly yourself the first time, and then offer copies to the agency staff for future licensure/credentialing. They can transcribe better than synthesize, so this seems to be the best way to go, IMO.
Hospital credentialing is nuanced, and depends on the culture of the local hospital in terms of how many references they require and how much documentation detail they request. Some hospitals are swift and lean, others comb through your background as if you are a likely convicted felon.
That being said, one thing is certain – if you plan to work several different locums assignments your referrers are going to be nagged TO DEATH. Everyone needs 2-3 professional references who will be called/contacted mercilessly, first by the Locums agency to make sure you’re not a “problem person” (as described in Part 1), then by the hospital who is considering hiring you (not that they’ve committed yet), then by the credentialing committee (if you pass approval in the first round), then by the state licensing body. So for every potential locums assignment, your professional reference will likely be contacted 4 times, and asked to vouch for you verbally or on paper/via fax. Imagine how many assignments you’ll do in a year and the math gets pretty scary. Be sure your references are ok with all this attention… and give them fair warning. If you can, spread the pain and broaden your reference base.
Q. What advice do you have for Locums agencies?
1. Physicians talk. Whatever sneaky deal-making you’re doing (such as paying people different rates for the same gig or getting a 50% premium at a desperate hospital and then not sharing it with us in salary upgrade) is going to come to light at some point, so keep your nose clean. Please be honest about problem hospitals and work conditions. I know that clients mislead you about work conditions and expectations so as to lure locums to their facility – but try to go the extra mile to figure out in advance if the doctors are really going to be asked to see 16 patients a day or 26 patients a day. Because if we get to the site and we’re being abused and overworked, we associate the negative experience with the agency that put us there. Then you try to wheedle and cajole us into finishing the assignment based on the contract we signed so you can make your cut. Meanwhile we’re putting our careers in danger because we can’t do a thorough job and might miss something important. Not good for physician retention. Better yet, just say no to crisis clients. The money isn’t worth it.
2. Treat us right and you’ll make more money in the long run. I know you’re under pressure to save money on our travel and hotels, but you also have some flexibility in the room rate that you’ll consider. Put us in a nicer hotel for a few bucks extra per night and the whole experience will seem a little brighter. Put us on the preferred rental car program so we don’t have to wait for 2 hours in a rental car line after a full day of cross-country travel. Upgrade us to a full size car rather than the beige Corolla we have to live in for months. These little things end up costing you only a few hours of our total billing, but make your agency our go-to employer.
3. Pay us on time. It’s so simple, and costs you nothing. If an agency takes 3-4 months to pay me for an assignment, and then the billing is inaccurate (missing hours)… I’m going to choose another agency next time. Your value to me is partly in the ease of payment – a direct deposit a week from when I fax my time sheets sends me the message that you have your act together and are respectful of my time. Making me sift through miss-billed records from half a year ago is just not acceptable.
4. Try to understand why we whine. Locums work is not easy. We are often separated from our friends and family, in an unfamiliar setting, learning complicated hospital processes with patients who are sick and dying. We don’t know if the nurses or consultants are competent while we ourselves are under intense scrutiny until the staff gets to know us. We have to build trust, navigate complicated electronic medical records systems, satisfy hospital coding and billing demands, and keep a ward full of patients (with their team of specialists whom we’ve yet to meet) on the path to healing. All this, and we are legally responsible for everything that goes on in the lives of those under our care. When we get home to our Days Inn at the end of our 15 hour shift in our beige Toyota Corolla to find their exercise equipment broken and the lobby overrun with monster-truck rally participants, we may be a tad whiny. Please don’t think ill of us for that. Just do what you can to help us feel better. We, and our patients, will thank you.
***
Dr. Jones is available on a consulting basis through Better Health LLC. She may be reached at val.jones@getbetterhealth.com
August 4th, 2013 by Dr. Val Jones in Opinion, True Stories
Tags: Costs, Hospital, How To, How To Find The Best Locums Agency, Internal Medicine, Locum Tenens, Physician, Salary, Traveling Physician
2 Comments »

On Assignment In Idaho
It’s been a couple of months since my last post because I’ve been traveling around the United States working as a locum tenens (in Latin, “place holder” – a more elegant name than “temp”) physician. We’ve all heard of traveling nurses, but more and more physicians are also “living la vida locums,” as it were. There are actually over 100 agencies who find/provide temporary physician coverage for hospitals who need to fill gaps in their full timers’ schedules. You can find out more about these agencies at their trade organization site, the National Association of Locum Tenens Organizations (NALTO).
For those of my peers who’ve been curious about locums work, but haven’t tried it, I thought I’d provide you with some personal thoughts and insights in the form of Q&A. Please feel free to ask your own questions in the comments section and maybe we can generate a nice, interdisciplinary discussion about locums work. I’d love to hear from others who have worked locums!
Q: Why should I work as a locum tenens physician?
If you don’t mind travel and are a fairly adaptable individual (i.e. can learn new EMR systems, staff idiosyncrasies, and navigate hospital politics without excessive angst), then you can expect to make at least 33% more in salary working as a locum (with professional liability insurance, housing and travel covered included). In addition, you have no administrative or teaching responsibilities, coding/billing hassles, or staff management issues. You’re paid an hourly rate for a minimum number of hours, with overtime negotiable. You get to see different parts of the country, and can control where you go and how much you work. (E.g. Summers in Sonoma, winters in Florida… not a bad lifestyle choice.)
Q: What kind of physicians do locums work?
In my experience, there are four kinds of people who do locums work: 1) Retirees – those who have essentially retired from full time medicine and want to keep their hand in clinically without overwhelming responsibilities and work hours 2) Salary Seekers – those who want to make 33-50% more salary and don’t care where they live to do it (they work 22 days/month or more as a locums doc) 3) Dabblers – those who want to work part time because they are busy with another job or family responsibilities and 4) Problem People – those who have personality issues and/or a legal history that make it difficult to hold down a regular job.
I don’t know the relative numbers of these 4 subtypes of physicians who do locums, but I’d guess that 20% are Retirees (Rs), about 10% are Salary Seekers (SS’s), 60% are Dabblers (D’s), and 10% are Problem People (PP’s). I’m a D, and I have met Rs, SSs, and PPs on the work circuit. I’ve also spent time talking to internists and specialists who work as locums physicians so I have an idea of what others outside my specialty are up to.
Q: What’s the difference between locums agencies?
Each locums agency has its own “corporate culture” and some are more attentive to their physicians than others. For example, when you’re traveling en route to an assignment and your flight gets cancelled on a weekend, you suddenly realize how nice it is to have a responsive agency to help with travel triage. Choosing an agency is more than just finding the one that offers the best hourly wage, it’s about how they choose and negotiate with clients (hospitals), how many staff they have to help with payroll and travel, and if the recruiters themselves are patient and attentive. All of this is primarily learned by trial and error – alas. And I think it’s probably time to create a “Yelp” destination of sorts for physicians who are interested in locums work. I wish I had had one!
That being said, what I’ve learned is that agencies vary A LOT in what they offer you and that there is usually about 25% wiggle room in hourly rate negotiation, especially for highly-sought after specialties such as Internal Medicine. In one case, a client (hospital) confirmed to me that two different locums agencies presented the same candidate to them – one was charging $90/hour more for the physician, but the physician had been quoted the same hourly rate by both agencies.
One would think that there would be an advantage to being represented by the “Platinum level” locums agency because they’d negotiate higher pay rates for you, but what happens is that they negotiate high pay rates and then don’t pass it along. In the end, the only hospitals that use those companies are ones who’ve exhausted every other avenue. So if you work for a Platinum agency, you end up with an average salary working in the most difficult situations (i.e. where no one else would go and the hospital, in an act of desperation, had to pay through the nose for you.) In addition, I’ve had a Platinum agency take 3 months to pay me, whereas another agency regularly turned my time sheet into direct pay in 7 days.
So be forewarned – the biggest, shiniest agency might not be your best bet.
Unfortunately, smaller agencies (who may be more generous with salary rates) sometimes suffer from skeleton crew staffing and fall short of being able to triage travel disasters and manage client-related problems (e.g. the hospital said you’d see 12 patients a day but when you arrive they ask you to see 24) as needed.
When it comes to a locum agency, you want someone who’s not too big, not too small, and where you can establish a relationship with a recruiter who is responsive and smart. I cannot stress this enough. Your recruiter is your lifeline while you are on the job. Recruiters don’t just spend their time finding physicians to fill positions, they are the key point of contact between you and the hospital where you work. Their role is to lobby for you, and keep the hospital accountable for your work load and work environment. If the hospital promised that you’d only need to see X number of patients/day, then your recruiter is the one to hold them to that standard. If you are concerned about patient safety because staff members are incompetent in some way, then (believe it or not) your recruiter will convey those concerns to the hospital and get the problem solved.
So overall, your locums experience depends on the corporate culture of your agency, the size and number of travel/credentialing staff they have available 24/7, and the quality of recruiter assigned to your case.
In my next post I’ll cover the following questions:
Q: Where are the most favorable locums jobs?
Q: How can I negotiate the best salary?
Q: How do locums agencies decide how to match you with a given job opportunity?
Q: What is the licensing and credentialing process like? How do I make it easier?
May 6th, 2013 by Dr. Val Jones in Health Tips, Opinion, True Stories
Tags: Best Case Scenario, Body Impedance, Clothing Fit, Diet, Eight Week Plan, Extreme Weight Loss, fat loss, Female, Is It Worth It, Middle-aged, Percent Body Fat, Strength Training, Wedding Diet, Weight Training
7 Comments »

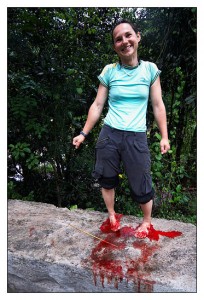
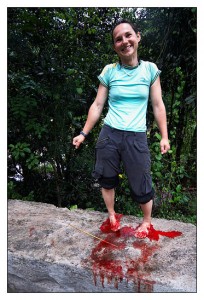
Dr. Val "After" Photo #1
I just completed 8 weeks of what I’d call “extreme dieting and exercise.” I don’t mean dangerous starvation and constant exercise, I mean the hardest “medically safe” amount of diet and exercise possible. It involved about 3 hours of exercise per day (6 days/wk), along with a calorie-restricted diet of 1500 calories/day (no refined carbs, only healthy fats, relatively high protein). My exercise consisted of heavy weight lifting, kettle bell sets, kickboxing, and sprints on the bike, summit trainer, and on an outdoor track, with long walks each afternoon. Trust me when I say – I pushed myself to the very limits of what my body could handle without becoming sick or injured. I did this with the help of my dear friend and trainer Meredith Deckert.
Why on earth would I do something so extreme? Well, first of all, I wanted the “right to bare arms” on my wedding day. I just woke up and realized I was getting married in 8 weeks and that I’d have photos of the event memorialized for my future kids and grand kids… so the “bat wings” had to go (you know what I’m talking about, ladies), and the time till “lift off” was pretty short – hence the need for maximum effort.
Secondly, I was scientifically curious to know what a “best case scenario,” two month, physique optimization strategy might produce. I knew I wouldn’t cheat on the diet or fall off the exercise wagon, so at least I could be sure that results were based upon strict adherence. Self-reports of diet and exercise regimens are notoriously inaccurate, so this doubting Thomas had to see for herself! (Of course n=1 in this experiment and won’t correlate exactly with others’ experiences due to differences in starting fitness, body fat, age, genetics and gender).
And Thirdly, I wanted to experience (first hand) what is possible so that I could empathize with my patients who were trying to lose weight, and provide personal anecdotes of encouragement. Since America’s biggest health challenge (pun intended) is obesity, I feel obliged to do my part to model lean living. Otherwise, what right do I have to teach others what to do? (Note that heavier physicians are less likely to educate overweight patients about weight loss).
So what did I learn? Each of these probably merits its own blog post, so I’ll summarize briefly and dig into the details with you soon…
1. Calorie math doesn’t necessarily work with the bathroom scale. We’ve all heard that a pound of fat equals 3,500 calories, so that if you decrease your calorie intake (or increase your calorie burn) by that much, you WILL lose a pound on the scale. That has not been my experience (I lost an average of only 30% of what the scale should have shown based on the math). I have some theories as to why that might be (which I’ll share later), but suffice it to say that if you are “doing everything right” and the scale is not rewarding you – take heart!
2. Weight training improves how you look MUCH more effectively than cardio. Before my extreme diet, I was running 1/2 marathons and spending hours on the spin bike. I was in excellent cardiovascular shape, but I had a relatively high percent body fat (about 30%) and I was certainly not getting “skinny” from all the running. I was actually losing muscle and looking softer and more “out of shape.” Dialing down the cardio and increasing the weight training had a rapid, visible impact on how athletic I looked.
3. Your leaner self may not look the way you think it will. When I first began my weight loss journey, I imagined that I would slowly melt away all the excess fat to reveal a lovely ballerina inside. What I found was that after the fat was gone, I wasn’t a ballerina at all. I looked a lot more like a wrestler! People really have different genetically determined body types – and no amount of diet and exercise will make us look like someone else. We’ll just look like our best selves, which is ok! Don’t fall into the trap of thinking that success only looks like a Sports Illustrated swimsuit model. After all, Olympic athletes all have very different bodies, and are at the top of their respective games! (This fun, height and weight database shows how you compare to recent Olympians.)
4. Clothing size is the most helpful measure of success. After 2 months of intense diet and exercise the scale only changed by about 6 lbs. The body impedance analyzer told a little different story (the InBody 520 estimated that I had lost about 10 lbs of fat and gained 5 lbs of muscle with an overall percent body fat loss of about 4%.) But the truth is, that nothing measured my success as well as clothing. I dropped nearly two dress sizes and had to buy a new wedding dress a week before the event! So if your scale isn’t showing you love, what are your jeans saying? Listen to them.
Conclusion: In my experience, the best a slightly overweight, middle aged woman can do (safely) in 8 weeks is lose 10 lbs of pure fat and gain 5 lbs of muscle. It is extremely difficult to achieve that much, and I would highly recommend doing it over a longer period of time. Is the pain worth the effort? Here are my “before” and “after” photos. What do you think?
Before: (151 lbs)

After (145 lbs):

November 26th, 2012 by admin in Quackery Exposed, True Stories
Tags: Alternative Medicine, Ayurvedic Medicine, Blood Letting, Bloodletting, CAM, Collagen, Glue, History, Horses, Leech, Leeches, Medicinal Leeches
No Comments »
 What did the jockey who never lost a race whisper into the horse’s ear? “Roses are red, violets are blue, Horses that lose are made into glue!” OK, so it’s a groaner. But until the advent of polyvinyl acetate (PVA) and other synthetic glues in the twentieth century, the destiny of aging horses was indeed the glue factory. The collagen extracted from their hides, connective tissues and hooves made for an ideal wood adhesive. Our word “collagen” for the group of proteins found in these tissues actually derives from the Greek “kolla” for “glue.”
What did the jockey who never lost a race whisper into the horse’s ear? “Roses are red, violets are blue, Horses that lose are made into glue!” OK, so it’s a groaner. But until the advent of polyvinyl acetate (PVA) and other synthetic glues in the twentieth century, the destiny of aging horses was indeed the glue factory. The collagen extracted from their hides, connective tissues and hooves made for an ideal wood adhesive. Our word “collagen” for the group of proteins found in these tissues actually derives from the Greek “kolla” for “glue.”
Not all aging horses were dispatched to the glue factory after their plow-pulling days came to an end. Some farmers found they could squeeze a little more profit out of the animals by assigning them another duty. They would become leech collectors! The elderly horses were driven into swampy waters only to emerge coated with the little bloodsucking worms. It seems the creatures found horses to be a particularly tasty treat! Since for many people suffering from various ailments, the little parasites were just what the doctor ordered, the harvesting of leeches made for a lucrative business.
Leeches have actually been used in medicine since they were first introduced around 1500 BC by the Indian sage Sushruta, one of the founders of the Hindu system of traditional medicine known as “Ayurveda.” That translates from the Sanskrit as “knowledge of life.” Sushruta recommended that leeches be used for skin diseases and for various musculoskeletal pains. Ancient Egyptian doctors extended the indications, treating headaches, ear infections and even hemorrhoids in this peculiar fashion. Galen, the famous Roman physician, used leeches to balance the four “humors,” namely blood, phlegm, black bile and yellow bile. Swollen, red skin, for example, was thought to be due to too much blood in the body and the answer was to have leeches slurp the excess.
Curiously, despite having no evidence for efficacy, bloodletting, either with leeches or by making an incision with a “lancet,” became part of standard medical practice for more than 2500 years! Monks, priests and barbers got into the act along with physicians. In 1799 George Washington had more than half his blood drained in ten hours, certainly hastening his demise.
Many British doctors preferred leeches, especially in areas around the mouth, ears and eyes where lancing was a tricky procedure. They even learned how to encourage a leech to bite by stimulating its appetite with sugar or alcohol. But the creatures were in short supply, and had to be imported by the millions from France, Germany, Poland and Australia where they were often caught in nets using liver as bait. Sometimes poor children earned a little extra money by wading into infested waters to emerge, like the horses, with leeches attached to their legs. A gentle tug or a pass with a flame then relaxed the bloodsucker’s grip before much damage ensued. Good thing, because leeches can be pretty nasty once they latch on. Remember Humphrey Bogart flailing about in African Queen while trying to rid himself of the little vampires?
The lack of leeches caused some physicians to explore recycling techniques. Usually a single leech becomes satiated after filling up on about 15 milliliters of blood and then falls off. But then if it is plunked into salt water, it will disgorge the blood and is soon ready for another round. A German physician even developed a technique to encourage continued sucking by making an incision in the leech’s abdomen allowing for the ingested blood to drain out as fast as it came in. It seems the leech wasn’t much bothered by this affront to its belly and would go on sucking for hours. Amazingly, leeches were sometimes used internally. To treat swollen tonsils, a leech with a silk thread passed through its body would be lowered down the throat and withdrawn when it had finished its meal. Sometimes the creatures were even introduced into the vagina to treat various “female complaints.” The literature is vague about how this was done but one account suggests that the technique required a clever nurse.
While bloodletting as a general treatment for ailments has been drained out of the modern medicine chest, there is still work for leeches. That’s because their saliva is a complex chemical mix of pain killers and anticoagulants. Hirudin, for example, is the protein that keeps the blood flowing steadily after the initial bite is made, and is so effective that the blood will not coagulate for quite some time even after the leech falls off. Indeed, these bloodsucking aquatic worms have received approval from the U.S. Food and Drug Agency as a “medical device.”
Surgeons have been known to use leeches after reattaching ears, eyelids or fingers that have been severed, as well as after skin grafts. This has to do with the fact that arteries are easy to reconnect but veins are not. Eventually new capillaries do form to reconnect veins, but in the meantime the finger or ear fills with blood which then clots and causes problems with circulation. A leech will drain the excess blood at just the right rate and can prevent blood clot formation by injecting hirudin. This is such a potent anticoagulant that it holds hope for dissolving blood clots after a heart attack or stroke. Unfortunately hirudin is too difficult to extract from leeches but can potentially be produced through genetic engineering techniques.
Where do physicians get leeches today? No need for horses. They can order them directly from the French firm Ricarimpex. One would think that after helping to save a finger or an ear the useful little critters would be rewarded. But their destiny is death in a bucket of bleach. Not any better than ending up in a glue factory.
***
Joe Schwarcz, Ph.D., is the Director of McGill University’s Office for Science and Society and teaches a variety of courses in McGill’s Chemistry Department and in the Faculty of Medicine with emphasis on health issues, including aspects of “Alternative Medicine”. He is well known for his informative and entertaining public lectures on topics ranging from the chemistry of love to the science of aging. Using stage magic to make scientific points is one of his specialties.
 Over the years that I’ve worked in acute inpatient rehab centers, I have been truly vexed by a particular type of patient. Namely, the stubborn patient (usually an elderly gentleman with a military or armed forces background). I know that it’s not completely fair to generalize about personality types, but it seems that the very nature of their work has either developed in them a steely resolve, or they were attracted to their profession because they possessed the right temperament for it. Either way, when they arrive in the rehab unit after some type of acute illness or traumatic event, it is very challenging to cajole them into health. I suspect that I am failing quite miserably at it, frankly.
Over the years that I’ve worked in acute inpatient rehab centers, I have been truly vexed by a particular type of patient. Namely, the stubborn patient (usually an elderly gentleman with a military or armed forces background). I know that it’s not completely fair to generalize about personality types, but it seems that the very nature of their work has either developed in them a steely resolve, or they were attracted to their profession because they possessed the right temperament for it. Either way, when they arrive in the rehab unit after some type of acute illness or traumatic event, it is very challenging to cajole them into health. I suspect that I am failing quite miserably at it, frankly.