January 3rd, 2012 by Nicholas Genes, M.D., Ph.D. in Opinion
No Comments »

I’ve been using my iPad in the ED, with my white coat’s sewn-in iPad-sized pocket, for some time now — mostly for patient and resident education, and to look up dosages or rashes. Hitting up my Evernote database or Dropbox documents is also useful. Occasionally I’ll use my iPhone, for its LED light (when the otoscope can’t reach to where I need to see) or rarely, its camera (in compliance with my hospital and department photo policy, naturally).
Our ED’s EHR isn’t quite accessible enough via iPad for me to quickly check results or place orders at the bedside — right now it’s just too cumbersome. But there’s been progress — enough so that I start to wonder about the flip side: instead of reviewing iOS medical apps and pining for an optimized EHR experience on the iPad, what if there are features of the iPad that could limit the utility of medical apps?
Well, there are some product design issues, like impact resistance and bacterial colonization, that have been discussed. But the operating system, iOS 5, has some quirks, too. Some have received a lot of attention. Some are maddening in their capriciousness. Read more »
*This blog post was originally published at Blogborygmi*
February 17th, 2010 by Peggy Polaneczky, M.D. in Better Health Network, True Stories
No Comments »

I got a letter from an insurer the other day, warning me that my patient, who had just refilled a prescription for a bisphosphonate I had prescribed almost a year ago for severe osteoporosis (yes, I do still prescribe dugs, despite how I feel about Big Pharma marketing), also had a claims diagnosis in their system for a bleeding peptic ulcer, and was I really sure she should be taking this medication, which could worsen her ulcer?
So do what any conscientious physician would do – I call her. (Of course, no one is ever home when I call these days, so it’s another few days of phone tag before I get her.) No, she has not been diagnosed with anything of the kind. Feels great, in fact. Read more »
*This blog post was originally published at The Blog that Ate Manhattan*
July 20th, 2009 by Dr. Val Jones in Expert Interviews, Opinion
No Comments »
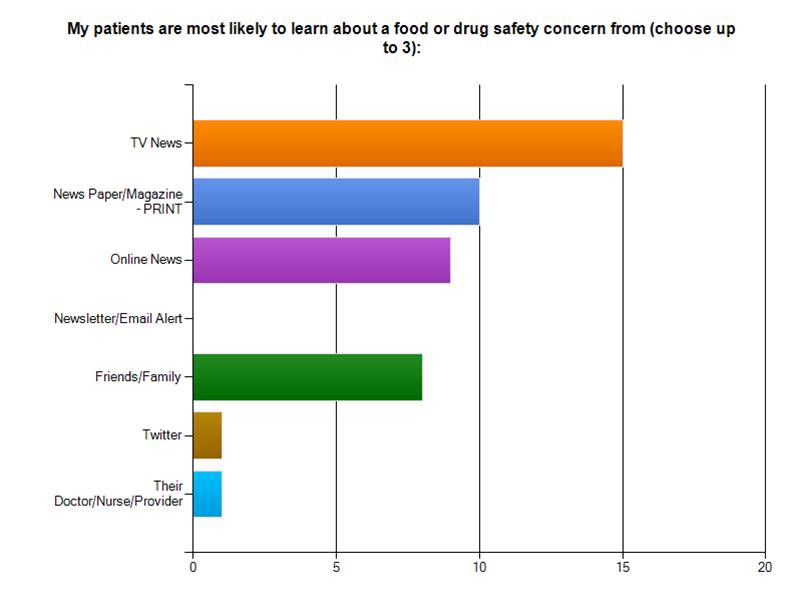
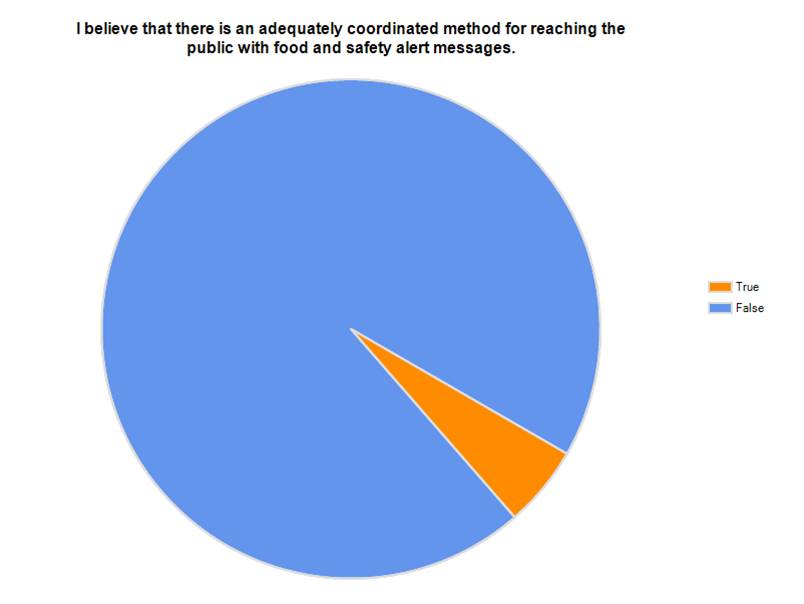
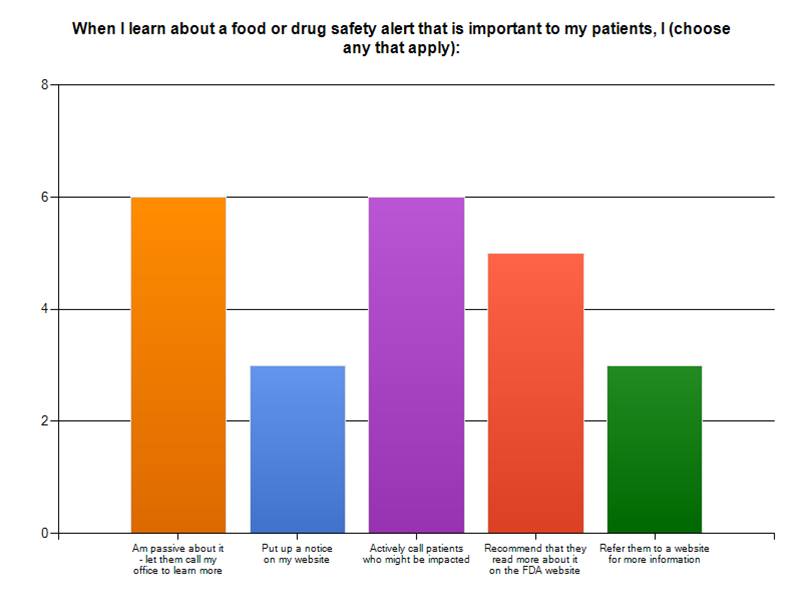
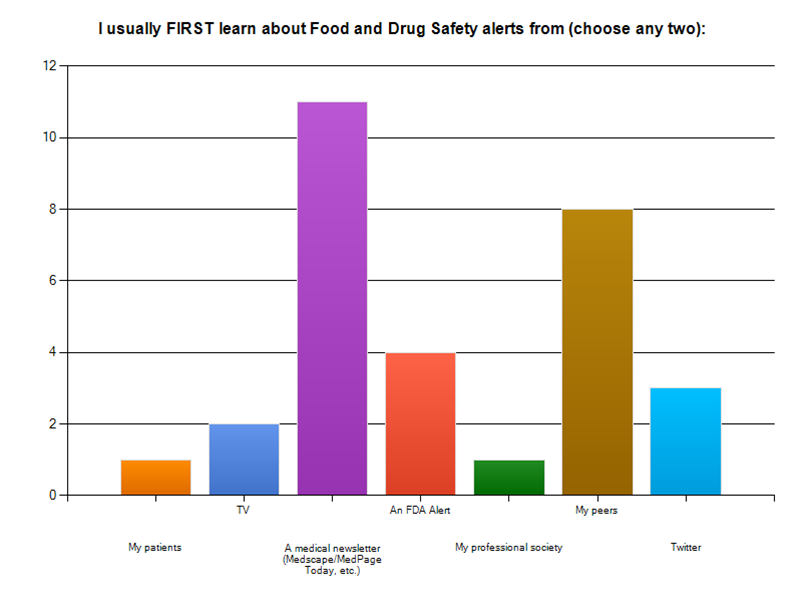
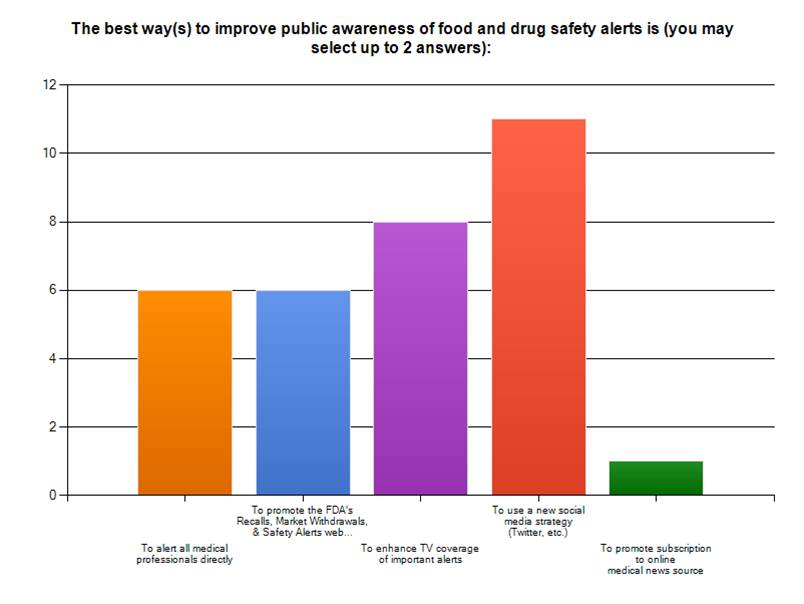
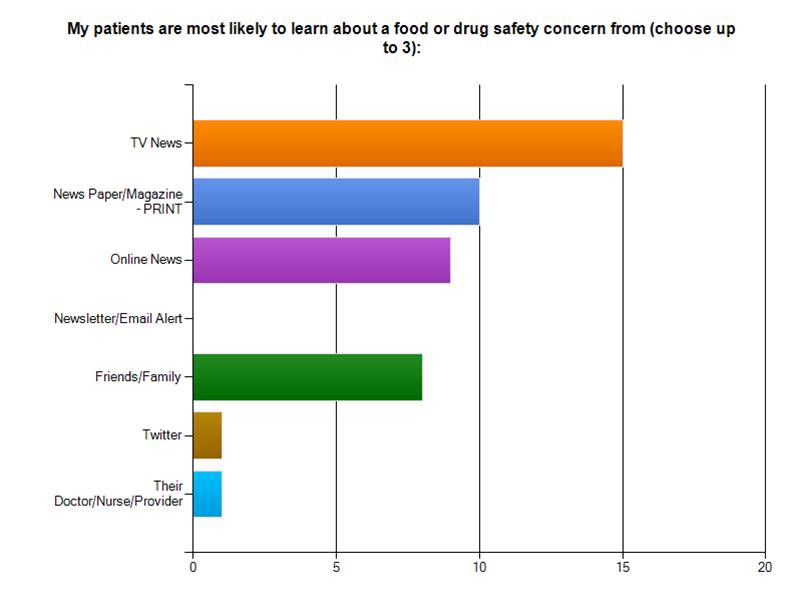
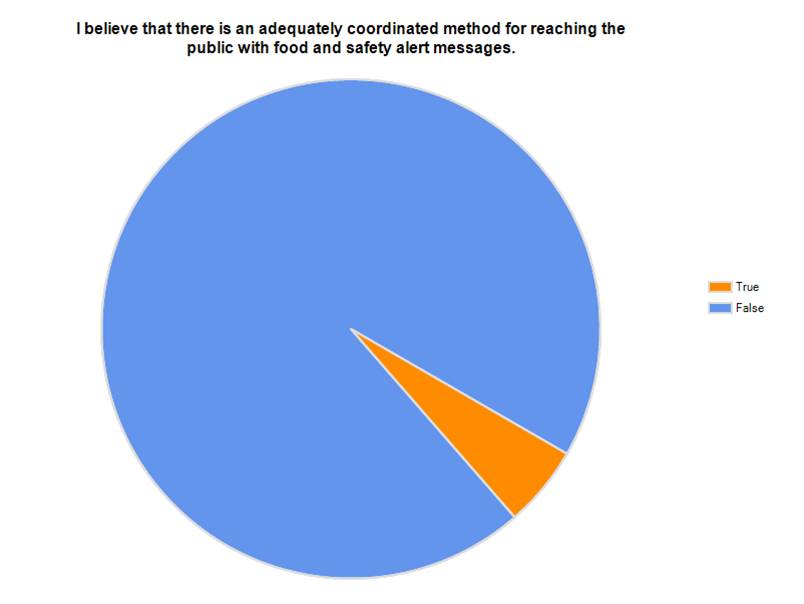
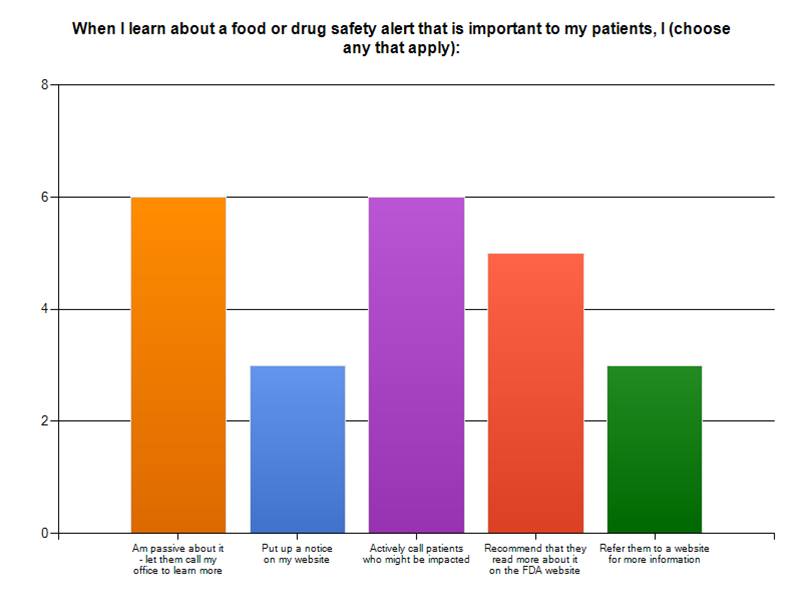
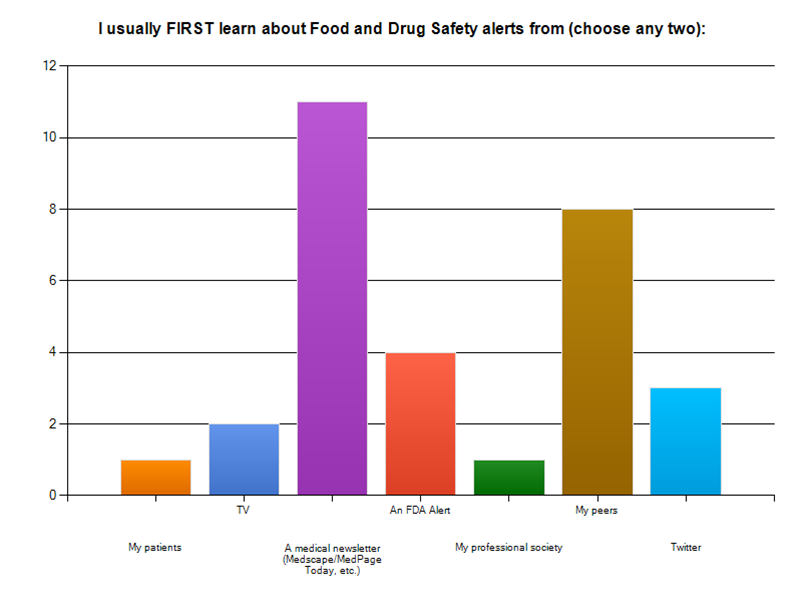
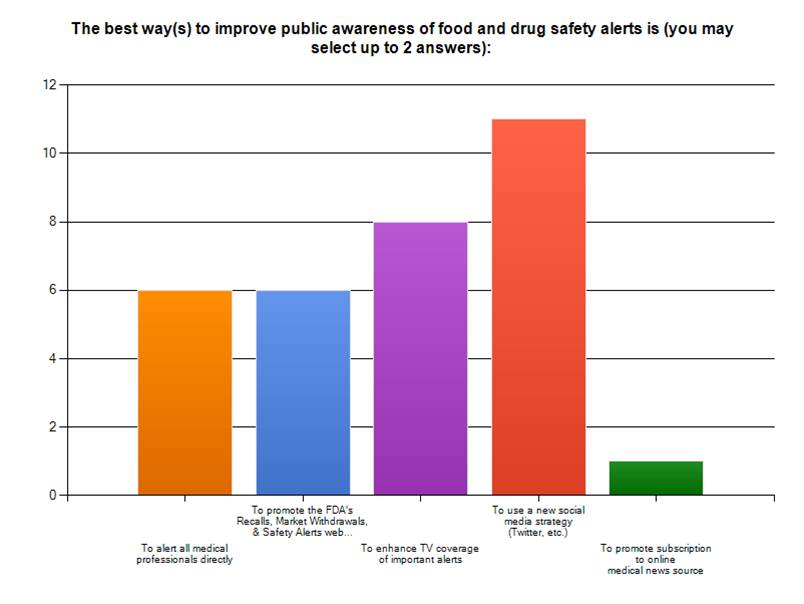
I recently created a focus group survey of physician bloggers to determine how they (and their patients) typically receive food and drug alerts. Twenty people responded. The results to 5 key questions are displayed below.
My most interesting take home messages:
1. Most physicians surveyed first receive drug alerts via eNewsletters from companies like MedPage Today and Medscape. (This is consistent with the large number of page views achieved by these sites/month).
2. Most patients find out about recalls via mainstream media – TV and newspapers.
3. EMRs, ePrescribing tools, coaching programs, and social media networks (like Twitter) are perceived to be the most valuable means of disseminating targeted recall information to the right person at the right time.
July 19th, 2009 by Nicholas Genes, M.D., Ph.D. in Better Health Network
No Comments »

There’s a satisfying post on WhiteCoat where he rants against patient-reported allergies. A sample:
When I ask patients about their medical allergies, more often than not patients suffer from at least one. During a recent shift, I had 17 people who told me that they had medication allergies. When someone has an allergy, I always ask what the allergic reaction is. The responses I received included the following:
* Seven people had allergies to various medications (most often penicillin) because their parents told them they had a reaction as a child. They didn’t know what the reaction was, but they have never taken the medication since.
* Four people had nausea and vomiting with medications that typically cause nausea and vomiting as one of their side effects…
He’s right — a lot of people have unwarranted concerns about mild or entirely predictable reactions, and sometimes this can be frustrating on a busy shift. But I also like the commenter who wrote:
I’m not sure how you think the patient is supposed to know which things actually require medical attention, especially when doctors and nurses refuse to give any guidelines over the phone. ‘Come on in, and if you’re aren’t seriously ill, then we can make fun of you on the blog tomorrow.’
Patient perceptions of allergies is a subset of a larger issue facing all of emergency medicine — patient perception of disease. We don’t expect patients to triage themselves, or figure out which symptoms are worrisome and which are benign. That’s our job. I try to look at proper allergy reporting as another opportunity for patient education (my favorite is explaining why someone can’t be allergic to the iodine atom).
More importantly, from the informatics perspective, allergy reporting is a big frustration as well (and one we can actually do something about, ourselves). Patient-reported allergies find their way into every EMR, and trigger the most inane alerts and stops, forever. If a patient reported vomiting once after codeine, every subsequent doctor who sees this patient will have to jump through electronic alert hoops just to order IV morphine. It doesn’t matter if the patient is taking oxycontin and wears three fentanyl patches. The same goes for antibiotics — I think most lay folks would be surprised that we have to wrestle, years later, with the inherited family warning of about penicillin reactions, even when ordering a 4th-generation cephalosporin with essentially no cross-reactivity…
There’s no intelligence built into the system, yet, I think because everyone’s afraid that if a patient has a bad outcome because that 14th medication alert was eliminated, they’d be liable. This line of thinking ignores the notion that bad outcomes are probably happening because there are so many useless alerts, they all tend to be ignored.
Someone told me recently (perhaps it was Dr. Reider?) that non-clinical folks involved in setting up electronic health information exchanges thought that communicated allergies to new providers would be the top priority, and were surprised when physicians considered allergies to be less important than, say, recent EKG’s, imaging, current med lists, and the like.
I wonder if this attitude toward allergy records is because we don’t think most allergies are that serious, because we can most often treat whatever arises… or because we’re overcome with alert fatigue.
Whatever the reason, there’s no doubt in my mind that if we had an intelligent, efficient system to process patient-generated allergy reports, we’d be less frustrated with this information, and more sympathetic to the patient’s concerns.
*This blog post was originally published at Blogborygmi*