March 12th, 2010 by Dr. Val Jones in Health Tips
1 Comment »
Allergists from the American College of Allergy, Asthma and Immunology (ACAAI) have some tips for reducing allergy symptoms this spring. I thought they were excellent and worth sharing… Enjoy!
Do:
1. Wear glasses or sunglasses when outdoors. Covering your eyes keeps pollen and other irritants away from this sensitive area, which reduces itchiness and redness.
2. Shower and wash your hair before bed. Cleaning up before getting into bed helps remove pollen from your hair and skin, which reduces irritation. You should also consider keeping pets out of the bedroom if they’ve been outside, as pollen can cling to their fur. Read more »
September 10th, 2009 by RamonaBatesMD in Better Health Network, Health Tips
No Comments »

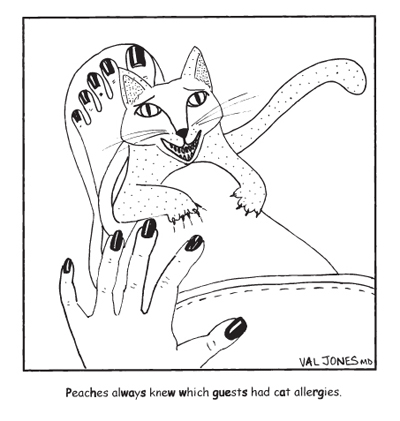
This past week I was once again asked about suture allergy. It has prompted me to revisit the issue which I have posted about twice now. (photo credit).
Sutures by their very nature of being foreign material will cause a reaction in the tissue. This tissue reactivity is NOT necessarily a suture allergy.
Many factors may contribute to suture reactivity.
- The length of time the sutures remain. The longer the sutures are in, the more reactivity occurs.
-
The size of the sutures used. The larger the caliber of the suture, the more reactivity. The increase of one suture size results in a 2- to 3-fold increase in tissue reactivity.
-
The type of suture material used. Synthetic or wire sutures are much less reactive than natural sutures (eg, silk, cotton, catgut). Monofilament suture is less reactive than a braided suture.
-
The region of the body the suture is used affects tissue reactivity. The chest, back, extremities, and sebaceous areas of the face are more reactive.
In general, accepted time intervals for superficial suture removal vary by body site, 5-7 days for the face and the neck, 7-10 days for the scalp, 7-14 days for the trunk, and 14 days for the extremities and the buttocks. The deeper placed sutures will never be removed.
Sutures meant to dissolve (ie vicryl sutures) placed too high in the dermis (which happens often when the dermis is thin) can “spit” several weeks to several months after surgery. This is a reactive process, NOT a suture allergy. It usually presents as a noninflammatory papule (looks very much like a pimple) and progresses with extrusion of the suture through the skin. The suture material may be trimmed or removed if loose, and it is not needed for maintaining wound strength. Rarely does this affect the scar outcome.
The remaining portion is a “repost” about suture allergies:
Allergic reactions to suture materials are rare and have been specifically associated with chromic gut. However, Johnson and Johnson mention known triclosan allergy as a contraindication for use of certain sutures (see below). Contact allergy to triclosan is uncommon.
Surgical gut suture (Plain and Chromic) is contraindicated in patients with known sensitivities or allergies to collagen or chromium, as gut is a collagen based material, and chromic gut is treated with chromic salt solutions.
MONOCRYL Plus Antibacterial suture should not be used in patients with known allergic reactions to Irgacare MP(triclosan).
PDS Plus Antibacterial suture should not be used in patients with known allergic reactions to Irgacare MP (triclosan).
VICRYL*suture should not be used in patients with known allergic reactions to Irgacare MP (triclosan). [In rechecking facts, I found that only Vicryl Plus has the triclosan, so simple vicryl or coated vicryl should be okay.]
Surgical Stainless Steel Suture may elicit an allergic response in patients with known sensitivities to 316L stainless steel, or constituent metals such as chromium and nickel. Skin staples are surgical steel so should be used with the same precautions.
Dermabond — Tissue glues should not be used in patients with a known hypersensitivity to cyanoacrylate or formaldehyde.
SO WHAT IS LEFT TO USE
So what is left to use in a patient who may have or has a proven allergy to suture or closure material?
Silk, Dexon, Nylon (monofilament or braided), Prolene, INSORB (absorbable staples), and any of the above listed (in the allergy section) to which the patient in question doesn’t react negatively.
The choice of a particular suture material will have to based further on the wound, tissue characteristics, and anatomic location. Understanding the various characteristics of available suture materials will be even more important to make an educated selection.
The amount of suture placed in a wound, particularly with respect to the knot volume, affects inflammation. The suture size contributes more to knot volume than the number of throws. The volume of square knots is less than that of sliding knots, and knots of monofilament sutures are smaller than those of multifilament sutures.
REFERENCES
Allergic Suture Material Contact Dermatitis Induced by Ethylene Oxide: G. Dagregorio, G. Guillet; Allergy Net Article
Johnson and Johnson Product Information
Current Issues in the Prevention and Management of Surgical Site Infection – Part 2; MedScape Article
MECHANICS OF BIOMATERIALS: SUTURES AFTER THE SURGERY; Raúl De Persia, Alberto Guzmán, Lisandra Rivera and Jessika Vazquez
Materials for Wound Closure by Margaret Terhune, MD; eMedicine Article
Product Allergy Watch: Triclosan; MedScape Article by Lauren Campbell; Matthew J. Zirwas
New References
-
Surgical Complications;
eMedicine Article, May 29, 2009; Natalie L Semchyshyn, MD, Roberta D Sengelmann, MD
-
Engler RJ, Weber CB, Turnicky R. Hypersensitivity to chromated catgut sutures: a case report and review of the literature.
Ann Allergy. Apr 1986;56(4):317-20.
[Medline].
-
Fisher AA. Nylon allergy: nylon suture test.
Cutis. Jan 1994;53(1):17-8.
[Medline].
Related Posts
Allergies from Suture Material (September 7, 2007)
Suture Allergies Revisited (April 30, 2008)
Suture (June 7, 2007)
Basic Suture Techniques (June 8, 2007)
*This blog post was originally published at Suture for a Living*
July 19th, 2009 by Nicholas Genes, M.D., Ph.D. in Better Health Network
No Comments »
There’s a satisfying post on WhiteCoat where he rants against patient-reported allergies. A sample:
When I ask patients about their medical allergies, more often than not patients suffer from at least one. During a recent shift, I had 17 people who told me that they had medication allergies. When someone has an allergy, I always ask what the allergic reaction is. The responses I received included the following:
* Seven people had allergies to various medications (most often penicillin) because their parents told them they had a reaction as a child. They didn’t know what the reaction was, but they have never taken the medication since.
* Four people had nausea and vomiting with medications that typically cause nausea and vomiting as one of their side effects…
He’s right — a lot of people have unwarranted concerns about mild or entirely predictable reactions, and sometimes this can be frustrating on a busy shift. But I also like the commenter who wrote:
I’m not sure how you think the patient is supposed to know which things actually require medical attention, especially when doctors and nurses refuse to give any guidelines over the phone. ‘Come on in, and if you’re aren’t seriously ill, then we can make fun of you on the blog tomorrow.’
Patient perceptions of allergies is a subset of a larger issue facing all of emergency medicine — patient perception of disease. We don’t expect patients to triage themselves, or figure out which symptoms are worrisome and which are benign. That’s our job. I try to look at proper allergy reporting as another opportunity for patient education (my favorite is explaining why someone can’t be allergic to the iodine atom).
More importantly, from the informatics perspective, allergy reporting is a big frustration as well (and one we can actually do something about, ourselves). Patient-reported allergies find their way into every EMR, and trigger the most inane alerts and stops, forever. If a patient reported vomiting once after codeine, every subsequent doctor who sees this patient will have to jump through electronic alert hoops just to order IV morphine. It doesn’t matter if the patient is taking oxycontin and wears three fentanyl patches. The same goes for antibiotics — I think most lay folks would be surprised that we have to wrestle, years later, with the inherited family warning of about penicillin reactions, even when ordering a 4th-generation cephalosporin with essentially no cross-reactivity…
There’s no intelligence built into the system, yet, I think because everyone’s afraid that if a patient has a bad outcome because that 14th medication alert was eliminated, they’d be liable. This line of thinking ignores the notion that bad outcomes are probably happening because there are so many useless alerts, they all tend to be ignored.
Someone told me recently (perhaps it was Dr. Reider?) that non-clinical folks involved in setting up electronic health information exchanges thought that communicated allergies to new providers would be the top priority, and were surprised when physicians considered allergies to be less important than, say, recent EKG’s, imaging, current med lists, and the like.
I wonder if this attitude toward allergy records is because we don’t think most allergies are that serious, because we can most often treat whatever arises… or because we’re overcome with alert fatigue.
Whatever the reason, there’s no doubt in my mind that if we had an intelligent, efficient system to process patient-generated allergy reports, we’d be less frustrated with this information, and more sympathetic to the patient’s concerns.
*This blog post was originally published at Blogborygmi*