October 27th, 2014 by Dr. Val Jones in Announcements, Medical Art
No Comments »
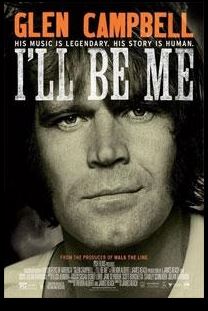 Country music legend Glen Campbell is dying of Alzheimer’s disease. In an effort to raise awareness of the illness he and his family made the brave decision to bare their lives by creating a documentary of Glen’s farewell tour. I highly recommend that you watch this film with your loved ones… and a box of Kleenex.
Country music legend Glen Campbell is dying of Alzheimer’s disease. In an effort to raise awareness of the illness he and his family made the brave decision to bare their lives by creating a documentary of Glen’s farewell tour. I highly recommend that you watch this film with your loved ones… and a box of Kleenex.
One of the most remarkable aspects of Glen’s disease was the preservation of his musical abilities despite severe cognitive impairment. Although he rarely knew where he was or even how to tie his shoes, he was able to perform songs in front of live audiences. With redirection and prompting, he managed to participate in 151 concerts across the United States within the span of ~18 months. Accompanied by his gifted guitarist son and daughter, and his doting fourth wife Kim, Campbell was able to maintain his musical self for longer than his physicians ever anticipated.
The documentary held nothing back – from violent outbursts brought on by paranoid delusions of golf club theft, to inappropriate table manners, to hypersexuality triggered by too high a dose of Aricept – the trials and tribulations of being a caregiver for someone with dementia were painfully acute. In brief moments of insight, Glen himself would manage to stammer a “Thank you. For being so nice to me. I have been an ass.”
One of the saddest moments of the movie was a brief clip of his daughter testifying before congress. She explains that memories are what lives are made of – and that although she is holding fast to the memories made with her dad, she knows that soon he will not even know who she is, and that their time together will be meaningless to him. Campbell listens silently next to her with a pained expression and misty eyes.
The movie’s final song, artfully strung together from clips of Glen singing repeat phrases into a studio mic, is haunting:
“I’m Not Going To Miss You”
I’m still here, but yet I’m gone
I don’t play guitar or sing my songs
They never defined who I am
The man that loves you ’til the end
You’re the last person I will love
You’re the last face I will recall
And best of all, I’m not gonna miss you.
Not gonna miss you.
I’m never gonna hold you like I did
Or say I love you to the kids
You’re never gonna see it in my eyes
It’s not gonna hurt me when you cry
I’m never gonna know what you go through
All the things I say or do
All the hurt and all the pain
One thing selfishly remains
I’m not gonna miss you
I’m not gonna miss you
Alzheimer’s is a terrible, cruel disease. I share the frustration of the Mayo Clinic neurologists who treated Glen Campbell – unable to do much more than simply document his decline and mentally prepare his family for the next stages of the disease. To all those who are taking care of people with Alzheimer’s I offer my sincere admiration and respect. To those who face a genetically higher-than-average chance of contracting the illness (such as myself), I tremble and hope for a cure.
November 15th, 2012 by admin in Health Tips
No Comments »
 Can we “train” our brains to be brighter, sharper, faster?
Can we “train” our brains to be brighter, sharper, faster?
A while back I wrote a post about a big study looking at “brain training”. The researchers wanted to know whether training programs that look like video games (like Brain Age andLumosity) could significantly improve brain performance on various tests. The results, in a nutshell, showed that while participants improved on the tasks they trained on (e.g., if the game involved ranking balls from smallest to biggest, the participants got *really* good at ranking balls from smallest to biggest), the improvement didn’t carry over to general brain function.Turns out ranking ball sizes doesn’t help you remember where you left your keys this morning.
Two years later, what’s the word?
I’m going to shift a little from how I normally do things (review a single article) and tell you about findings I learned about at the recent Aging and Society conference. At the conference, several researchers talked about brain training in the context of aging. We know that as we get older our cognitive abilities decline – we forget names and words, misplace our shopping lists, and process information a little bit more slowly. Wouldn’t it be fantastic if we could just spend ten minutes a day playing games on our iPad and successfully counter this decline? Of course it would be fantastic. Not just for us, but also for the companies who are trying very hard to convince us to buy their products to improve our cognition.
The problem is that skills are specific. If you want to become a fabulous jazz pianist, you have to play the piano (preferably jazz songs, too). If you want to become a star ballet dancer, you have to practice ballet. If you want to become a better mountain biker, you have to mountain bike – road biking will improve your leg strength and fitness, but ultimately it won’t make you a better mountain biker. So why should things be any different for brain skills?
As it turns out, they aren’t. Two years later, nearly all the research conducted in the field of brain training is turning up the same results: people only get better at the tasks they trained on – the improvement doesn’t cross over to more general skills, different skills, or everyday life. In one study, a researcher compared a commercially available brain training program with what she called an “active control” – a group that simply played regular video games like Tetris. She found that the group who spent time on the commercially available brain training program actually saw some aspects of their cognition decline compared with the control group. Bummer.
Now don’t throw out your Brain Age game yet – everyone at the conference agreed that engaging your brain in training programs is better than not doing anything. And most of the researchers felt that while the programs don’t work now, it’s not to say they’ll never work. We are increasingly more knowledgeable about how the brain works, what happens when we get old, and what different training tasks do. So it’s quite possible that sometime in the near-ish future (don’t ask me when) we could see the advent of brain training programs that do have a significant and lasting impact on cognition.
Until then, there is one thing you can do to have a significant and lasting impact on your brain health… And I’ll tell you in the next post.
***
Dr. Julie Robillard is a neuroscientist, neuroethicist and science writer. You can find her blog at scientificchick.com.
December 27th, 2011 by PreparedPatient in Health Tips
No Comments »

 Seeking Shelter
Seeking Shelter
The word hospice originated from the Latin hospitium, which means “to host or offer a place of shelter.” In 2009, an estimated 1.56 million patients, more than 40 percent of deaths, received hospice services in the United States. But many others who might have benefited from hospice care did not seek services, perhaps due to misconceptions, fears and the lack of information of patients, caregivers and even physicians.
“Hospice is a collection of services that are designed to support the patient and family through the course of a serious or terminal illness,” said Donald Schumacher, Psy.D, president and CEO of the National Hospice and Palliative Care Organization (NHPCO). The aim of hospice is to provide physical and emotional care and comfort in the months, weeks and days before death.
It’s often hard for patients and their loved ones to acknowledge that the time to consider hospice care has come. People come to that realization differently and there are some that might never seem to face that the end of life is near. But through the ups and downs of emotions and physical status, hospice team members Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
November 24th, 2011 by RyanDuBosar in Research
No Comments »

Sending dementia patients to the hospital could overwhelm the health care system and not offer them any better care at the end of life, researchers noted.
The researchers obtained data on all hospitalizations involving a dementia diagnosis for the 85 years and older group between years 2000 and 2008 from the nationally representative Nationwide Inpatient Sample database, a part of the Agency for Healthcare Research and Quality Healthcare Costs and Utilization Project.
Annual hospitalization data came from the U.S. Census Bureau. They projected the future volume of hospitalizations involving a dementia diagnosis in the 85 years and older group two ways, Read more »
*This blog post was originally published at ACP Internist*
November 21st, 2011 by HarvardHealth in Health Tips
No Comments »

No matter how sick my grandmother got or what her doctors said, she refused to go to the hospital because she thought it was a dangerous place. To some degree, she was right. Although hospitals can be places of healing, hospital stays can have serious downsides, too.
One that has been getting a lot of attention lately is the development of delirium in people who are hospitalized. Delirium is a sudden change in mental status characterized by confusion, disorientation, altered states of consciousness (from hyperalert to unrousable), an inability to focus, and sometimes hallucinations. It’s the most common complication of hospitalization among older people.
We wrote about treating and preventing hospital delirium earlier this year in the Harvard Women’s Health Watch. In the New York Times “The New Old Age” blog, author Susan Seliger vividly describes her 85-year-old mother’s rapid descent into hospital delirium, and tips for preventing it.
Although delirium often recedes, it may have long-lasting aftereffects. Read more »
*This blog post was originally published at Harvard Health Blog*
 Country music legend Glen Campbell is dying of Alzheimer’s disease. In an effort to raise awareness of the illness he and his family made the brave decision to bare their lives by creating a documentary of Glen’s farewell tour. I highly recommend that you watch this film with your loved ones… and a box of Kleenex.
Country music legend Glen Campbell is dying of Alzheimer’s disease. In an effort to raise awareness of the illness he and his family made the brave decision to bare their lives by creating a documentary of Glen’s farewell tour. I highly recommend that you watch this film with your loved ones… and a box of Kleenex.

 Can we “train” our brains to be brighter, sharper, faster?
Can we “train” our brains to be brighter, sharper, faster?
 Seeking Shelter
Seeking Shelter









