An Overview Of Misleading Health Information Found On WebMD
Consider this list:
- Sex Matters: tuning in to what turns you on.
- Ticker tune-up tips for guys.
- Manatomy explained.
- Burning down under? It’s time to fess up.
- Pumped Up: ED meds aren’t working? An implant could be the solution.
- When your hoo-ha’s burning, don’t use this common cure!
- Go Om: Meditation can be the healthy answer for type A’s.
- Sexy Seniors: The age-old pleasures and challenges of getting it on.
- Pain: Are your knees at ease?
- Retail Therapy: Four proven ways to battle the call of the mall.
- Detox Diets: The Scary New Skinny
Readers acquainted with popular culture know that such inane, annoying phrases are typical of American women’s magazines. Thus it may be surprising to learn that only three entries were quoted from sources clearly recognizable as such: numbers 3 and 6 from Cosmopolitan, and number 11 from Glamour. The rest were found in WebMD: the Magazine:
The magazine appears to have been introduced in 2005. According to its masthead page,
WebMD’s mission is to provide objective, trustworthy, and timely health information. Our website and magazine provide credible content, tools, and in-depth reference material about health subjects that matter to you. We are committed to providing information on a wide variety of health topics, all of which are reviewed by our board-certified physicians.
Every physician I know receives a “COMPLIMENTARY WAITING ROOM COPY” each month; the 3 or 4 waiting rooms that I’ve perused have been amply stocked. I suspect that most office managers are happy to be provided with free reading material that seems appropriate for patients, and that most physicians haven’t given the magazine more than a passing glance. The problem is that the magazine, like the consumer website of the same name, offers a mixture of accurate-if-mundane information, misleading health claims, exaggerated nutritional advice, unwarranted fear-mongering, and pseudoscientific nonsense. I’ll limit examples and comments to the final four categories.
Misleading Health Claims
In the July/August 2009 issue, which features Jimmy Fallon on the cover, is an article offering five Amazing Facts About Heart Health and Heart Disease. Under ‘fact’ #3 is this assertion:
Health experts now have proof that laughter is good medicine.
The proof?
A good belly laugh can send 20% more blood flowing through your entire body. One study found that when people watched a funny movie, their blood flow increased. That’s why laughter might just be the perfect antidote to stress. When you laugh, the lining of your blood vessel walls relaxes and expands, Krasuski says. So have a good giggle. Your heart will thank you.
Hmmm. I’m willing to believe, even without data, that a good belly laugh can increase cardiac output by 20% (not much compared to, say, exercise or fever). Blood vessel walls (not just the ‘lining’) relax and expand almost continuously, but I’ll grant that such changes are greater during periods of rapid changes in cardiac output than during periods of rest. What doesn’t follow from this is that laughter is an ‘antidote to stress’ (whatever that is); nor, whether it is or isn’t, will ‘your heart’ necessarily ‘thank you’ for laughing.
If your heart is healthy or even moderately diseased, laughing will be of no consequence to it; if it is extremely unhealthy—if you have severe coronary disease with unstable angina, for example, or severe valvular or myocardial (heart muscle) disease such that the slightest increase in demand for blood flow can result in congestive heart failure, laughing might get you into serious trouble. Few people are that fragile, but any magazine that claims to give trustworthy, in-depth health information should make the point.
“Amazing Fact” #3’s main implication, of course, is that laughing ‘might’ reduce your risk of some heart diseases, much as controlling high blood pressure and reducing LDL-cholesterol are known to do, and as regular exercise probably does. The article offers not an iota of credible evidence to support this implication. Nor is there a basis for its implicit corollary, that increasing cardiac output by whatever means is equivalent to the cardiovascular conditioning that occurs with regular exercise.
The article notes, correctly, that the frequency of ‘heart attacks’ is greater in the morning than during the remainder of the 24-hour cycle, but somehow leaps to unrelated and unsupported premises, conclusions and recommendations:
Add in the rise in blood pressure and increased heart rate from the stress of returning to work after the weekend, and you have the perfect recipe for a Monday morning heart attack. That’s why it’s important to reduce your stress levels as much as you can. Practice yoga, meditate, exercise, laugh (see tip No. 3), or spend more quality time with your family — whatever works best for you.
Oh well, at least it throws a bone to poor, sex-starved men:
5. How sex helps the heart
Having an active sex life could cut a man’s risk of dying from heart disease in half. For men, having an orgasm three or four times a week might offer potent protection against a heart attack or stroke, according to one British study.
Whether sex works as well for women’s hearts is unclear, but a healthy love life seems to equate to good overall health. For one thing, sexual activity is an excellent stress buster. It’s also great exercise — burning about 85 calories per half-hour session.
If you find it difficult to have sex, that could be a big red flag that something is wrong with your heart. For example, some researchers think erectile dysfunction might warn of a heart attack up to five years in advance.
A few years ago a friend confided to me that his new girlfriend was convinced of something that he was pretty sure was nonsense, but that he’d no intention of talking her out of: ingesting human semen on a daily basis was good for her health (yup, it’s out there). “Amazing Fact” #5 strikes me as a soft-core version of such a belief. I also wonder how WebMD’s board-certified physicians could stomach the claim that the penis acts as an early-warning system for heart attacks destined to occur five years later. It’s all a bit hard to swallow.
The cover story in the same issue promises to explain “why type A’s (sic) like Fallon tend to get sick on vacation”:
Urban legend, or does the body’s immune system intuitively understand how to sabotage your best-laid plans?
“It seems like we’ve all experienced it,” says Phyllis Kozarsky, MD, travel health expert for the Centers for Disease Control and Prevention. “Especially the type A personality, the real go-go-go kind of person who works very hard and takes very few vacations.
“From my 30 years of practice and observing my patients, I think it’s less about a mind-body connection — although I do believe there is one — and more about how stress plays a role in making us sick,” Kozarsky adds. “By the time we are on our so-called ‘break,’ we’re utterly drained and susceptible to catching whatever bug is floating by.”
Ah, but we were never told whether or not it’s an ‘urban legend’ (my guess is that it is). Why offer a theory in search of a phenomenon?
Exaggerated Nutritional Advice
From the June 2009 issue:
Tea Time
One habit you don’t want to bag? Drinking tea. Studies suggest that some teas might help with cancer, heart disease, and diabetes; lower cholesterol; and heighten mental alertness. Tea also appears to have antimicrobial qualities.
Tea is a name given to a lot of brews, but purists consider only green, black, white, oolong, and pu-erh teas the real thing. All are derived from the same plant and contain unique antioxidants called flavenoids. Potential health benefits include:
Green Tea: Its antioxidants could interfere with the growth of bladder, breast, lung, stomach, pancreatic, and colorectal cancers. Green tea might also prevent clogging of the arteries, burn fat, counteract oxidative stress on the brain, reduce risk of neurological disorders such as Alzheimer’s and Parkinson’s diseases, reduce risk of stroke, and improve cholesterol levels. [etc.]
Phew! But no. Drinking green tea has been associated with reduced mortality due to some of the above but not others, which may or may not have anything to do with the tea: correlation is not causation, whether the topic is tea, orgasms, or anything else. Consumers and board-certified physicians should be wary of panacea claims. After an early period of enthusiasm, trials of antioxidant supplements have been disappointing and worse, in spite of some of the purported benefits having been entirely plausible.
More of the same, from the March/April 2009 issue (pictured above):
[Shallots] also contain flavonoids, a type of antioxidant found in fruits and vegetables that helps protect the body and may reduce the risk of developing cancer, heart disease, and diabetes. (Garlic, leeks, and onions also have great cancer-fighting nutrients, by the way.) Plus, one tablespoon of chopped shallots is high in potassium, vitamin A, and folate.
Groan.
Unwarranted Fear-Mongering
The March/April issue has an article titled “Easy Being Green”:
You don’t need to call in a hazmat team. Try these tips to get rid of the harmful toxins in your home.
What harmful toxins? You’ve probably guessed already:
the products we use every day…cosmetics, antibacterial soaps and cleaners…’plasticizers’ used in plumbing, shower curtains, varnishes, vinyl floors…fragrances.”
Today, a growing group of environmental activists, scientists, and ordinary people is calling attention to the possible real-life risks of the products we swallow, spray, and smear on our bodies every day.
“It’s not in question that many consumer products contain toxins — they do,” says Alan Greene, MD, clinical professor of pediatrics at Stanford University and author of Raising Baby Green: The Earth-Friendly Guide to Pregnancy, Childbirth, and Baby Care. “Most are felt to be in too tiny of a quantity to pose any real risk. But sometimes, very small exposures can have large impacts.”
Spurred by recent research studies, some of which contradict established opinion about what’s safe, environmental advocates now have some of the most commonly used consumer products on their watch lists.
“The irony is, these products’ presumed safety has led them to be produced and consumed almost indiscriminately,” says Rebecca Sutton, PhD, senior scientist with the nonprofit Environmental Working Group. “We’re now all exposed to multiple chemicals on a continuous basis whose long-term health effects aren’t known.”
Certain personal care products have become so popular, they’re literally in our blood. The Centers for Disease Control (CDC) now monitors the levels of ingredients from cosmetics and other products in the bloodstream of random Americans, to help guide public health discussions.
Sigh. Don’t get me wrong: I favor elucidating and dealing with real environmental hazards as much as anyone else. What I’m against is the argument from ignorance (also called the “negative proof fallacy”) explicit or implicit in ‘toxin’ hysteria: that since we don’t know that ubiquitous substances that are clearly toxic at certain concentrations are not also toxic at vastly lower ones (perhaps in very subtle or even undetectable ways!), we ought to assume that they are. No: we ought, unless real evidence suggests otherwise, assume that they are not.
The reasons are several, beginning with the obvious problem of all arguments from ignorance: there is no basis for not being afraid of, well, almost everything. Where should people who are trying to live their lives draw the line? ‘Certain personal care products’ have literally been in our blood ever since we started using ‘personal care products’ back in Bedrock. Do WebMD’s board-certified physicians really think that this is a recent phenomenon? Speaking of, an editorial in a real journal notes that asbestos is a naturally occurring substance found in rocks all over the world:
…studies indicate that everyone is exposed to background levels of asbestos in the ambient air. Studies have shown that members of the general (non-occupationally exposed) population have tens of thousands to hundreds of thousands of asbestos fibers in each gram of dry lung tissue, which translates into millions of fibers and tens of thousands of asbestos bodies in every person’s lungs. However, the general population does not have an increased risk of asbestos-related lung cancers despite these background levels.
What are these “small exposures that can have large impacts”? Why haven’t I heard of them? Why didn’t the WebMD reviewers insist that they be explained?
A modicum of knowledge and a bit of common sense go a long way here. Famous examples of proven harms from environmental toxins have been distinguished by their clarity: both the sources of exposure and the outcomes have, typically, been discrete and specific to the toxin. The exposures have been substantial, not merely casual. Think: cigarette smoking and lung cancer; asbestos workers and mesothelioma; coal-mining and black-lung disease; eating lead paint and anemia/neurologic/kidney disease; eating radium and anemia/bone-necrosis/cancer; eating mercury and neurologic disease. But NOT, to any measurable extent: ‘passive smoking’ and lung cancer; asbestos in your basement and mesothelioma; a piece of coal on your coffee table and black-lung disease; changing the battery in your car and lead poisoning; mercury preservatives in vaccines and neurologic disease; etc.
Contrary to ‘conventional wisdom’, chemical and biological hazards in the household have become rarer recently, not more common. Popular patent medicines of the 18th, 19th and early 20th centuries were likely to contain large amounts of arsenic, mercury, acetanilide, radium, opium, digitalis, cocaine, or other poisons. Smoke from wood and coal stoves and from tobacco has become increasingly rare, as has lead in paint and gasoline. Food can be refrigerated or frozen at any time of the year. Water is safe. Plumbing exists. We know about germs. We know about rusty nails. We know how to kill botulinum spores in the process of canning. We have immunizations. See where this is going?
Sure, there might be some trace substance lurking out there that would be worth worrying about if only we knew what it was. If some people want to waste their own time, drive their family and friends crazy, and turn their children into paranoid neurotics, I suppose that’s their prerogative. What I don’t like is a consumer health magazine, ostensibly reflecting the views of board-certified physicians such as myself, erroneously Hyping Health Risks to every patient in every doctor’s office in the country.
Pseudoscientific Nonsense
And now for the pieces de resistance. Where to begin? Let’s start with an advertisement that ran in both the May and June issues:
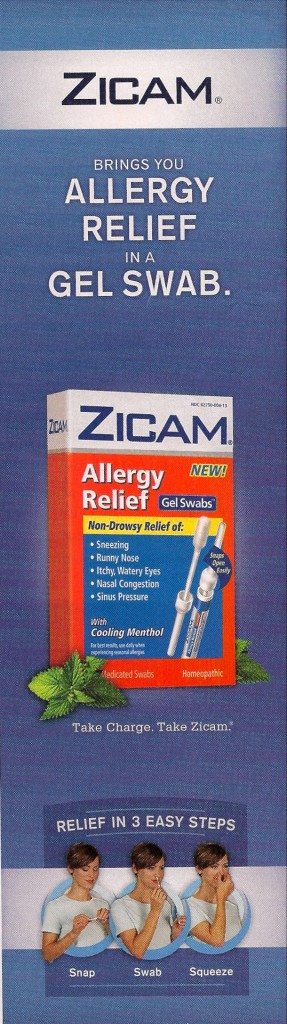
Look familiar? The ad appeared in the very month that the FDA warned consumers not to use another Zicam product because it might destroy their sense of smell. Funny: the following month’s issue of WebMD magazine made no mention of that. The website did report it without mentioning that Matrixx, the maker of Zicam, was one of WebMD’s sponsors. More worrisome to me is how WebMD’s board-certified physician reviewers could have overlooked “Homeopathic”—a sure sign of quackery—printed right on the picture of the Zicam Allergy Relief package.
Could it be that since this was merely an ad, the reviewers either didn’t feel obliged to examine it or were not given the opportunity? Perhaps, but that turns out to be moot. Consider this exchange between the Chief Medical Editor, Michael W. Smith, MD, and Dr. Jordan Josephson, an ear, nose, and throat specialist whom Dr. Smith interviewed about “Sinus Solutions”:
Q: What promise do alternative and complementary therapies hold for those who have spring allergies?
A: Besides irrigation, acupuncture seems to work well for some people through the rebalancing of chi (the energy forces in the body), which can help fortify the immune system to help alleviate the symptoms of sinusitis, allergies, and asthma.
Some of my patients want to try homeopathic remedies, so I send them to doctors who do integrative medicine. A very diluted amount of a particular medicine or combination of medicines is given on the theory that it will boost the immune system. The treatment is individual; each patient is carefully evaluated and receives a specific combination of homeopathic ingredients.
Neither Dr. Smith nor Josephson appeared hesitant to endorse such imaginary healing methods, just as neither appeared to know much about them.
Immune System Inanities
As exemplified above, fanciful statements about the immune system are almost as common in the magazine as are vacuous statements about ’stress’:
Q: Recent research shows that even mild stress or anxiety can worsen allergy symptoms.
A: It’s true: Mild stress or, in today’s economy, major anxiety weakens your resistance. So that does worsen allergies and leave you more susceptible to infections. It’s well known that stress has a relationship to your body’s immunity. —”Sinus Solutions”
…
Health benefits of meditation
Mitchell’s experience is borne out by studies showing that meditation not only lowers blood pressure but also can amp up your immune system — although the mechanism isn’t clear…
Raison participated in a study that indicated that meditation improved both physical and emotional responses to stress. In the study, people who meditated regularly for six weeks showed less activation of their immune systems…
Science hasn’t yet connected the dots between what happens in the meditating brain and the immune system. But a University of Wisconsin study saw increased electrical activity in regions of the left frontal lobe, an area that tends to be more active in optimistic people, after eight weeks of training in meditation. —Go Om
…
A pet is certainly a great friend. After a difficult day, pet owners quite literally feel the love.
In fact, for nearly 25 years, research has shown that living with pets provides certain health benefits. Pets help lower blood pressure and lessen anxiety. They boost our immunity.
… a growing number of studies have suggested that kids growing up in a home with “furred animals” — whether it’s a pet cat or dog, or on a farm and exposed to large animals — will have less risk of allergies and asthma…
If a dog lived in the home, infants were less likely to show evidence of pet allergies — 19% vs. 33%. They also were less likely to have eczema, a common allergy skin condition that causes red patches and itching. In addition, they had higher levels of some immune system chemicals — a sign of stronger immune system activation.
“Dogs are dirty animals, and this suggests that babies who have greater exposure to dirt and allergens have a stronger immune system,” Gern says.
People in stress mode get into a “state of dis-ease,” in which harmful chemicals like cortisol and norepinephrine can negatively affect the immune system, says Blair Justice, PhD, a psychology professor at the University of Texas School of Public Health and author of Who Gets Sick: How Beliefs, Moods, and Thoughts Affect Your Health. —”Animal Instinct“
…
“Like all living organisms, our bodies are making defective cells all the time,” Servan-Schreiber writes. “That’s how tumors are born. But our bodies are also equipped with a number of mechanisms that detect and keep such cells in check.” Supporting the processes that allow the body to recognize and destroy these errant cells is good medicine.—Book Review of Anticancer: A New Way of Life (I can’t find it on the website)
OK, let’s get this straight. “Fortifying” the immune system alleviates the symptoms of allergies and asthma. Even mild stress can worsen allergy symptoms; it weakens your resistance. It’s well known that stress has a relationship to your body’s immunity. So far, so good. Meditation amps up your immune system; that sounds about the same as fortifying or boosting it, no? Makes sense, because meditation improves emotional responses to stress. Oops: people who meditated regularly for six weeks showed less activation of their immune systems. Huh? Isn’t that like, uh, the opposite of amping it up?
Never mind: your pooch will both reduce your stress and boost your immunity, and you’ll have fewer allergies and asthma attacks. Fuggit: science hasn’t connected the dots yet anyway, so who cares?
Seriously, folks, this is a buncha oversimplified baloney. The immune system is a vast complexity of cells, molecules, and signals. It usually works quite well, as long as we aren’t starving or critically ill. It can get us into trouble by being inadequate to meet a challenge if, for example, it is weakened by a disease like AIDS. It can also cause trouble by being ‘overactive’ as is the case, almost by definition, for allergic reactions. Thus “boosting” the immune system seems like a bad idea if the goal is to reduce allergic reactions or to prevent exacerbations of other conditions that have allergic or auto-immune components, such as asthma, rheumatologic diseases, psoriasis, and inflammatory bowel disease. But this is also an oversimplifcation, because the immune system is complex and subtle: such diseases almost certainly reflect disturbances in modulations of various processes within it, rather than crude overactivity.
There are so many parts in the immune system that it’s a simple matter to demonstrate some change in the concentration of one or two (serum proteins, typically) after any of numerous interventions. In most instances, we have no idea what such changes mean or whether they have any importance. For an introductory critique of the ‘immune surveillance’ theory of cancer, read this essay.
“Boosting the immune system,” like “detoxification,” “holistic,” “integrative,” “complementary,” and “alternative,” are terms that in the context of popular medical treatises almost always herald pseudoscience and quackery. It’s regrettable that WebMD is chock full of them. On the website are more ads for homeopathic nostrums, numerous fanciful articles about acupuncture and ‘Eastern’ health wisdom, erroneous and misleading statements about naturopathy, chiropractic, and other quackery, and much more.
I wonder why. Is it just that fantasy is easier and more instantly gratifying than reality?
*This blog post was originally published at Science-Based Medicine*













