March 21st, 2010 by Toni Brayer, M.D. in Better Health Network, True Stories
No Comments »


I can’t get the stories of Haiti out of my mind. A patient showed up at the Port au Prince hospital ward with a massive left sided paralysis: an obvious stroke. This 48-year-old woman had collapsed the day before and was now accompanied by her three grown daughters, who were most attentive and worried. I examined her in the bed with other patients and families gathered around. (There is no sense of privacy and even an exam seems to be everyone’s business in Haiti). One daughter spoke broken English, but I had a good translator that helped me get the information I needed. It was a sad story. Read more »
*This blog post was originally published at EverythingHealth*
March 8th, 2010 by DaveMunger in Better Health Network, Research
No Comments »
When I began work on this month’s project, I contacted a clinician, a case manager, and a scientist to get their perspectives on how we’re making progress fighting HIV and AIDS. I’ve introduced you to the clinician and the case manager, but not the scientist.
Dave Wessner doesn’t actually study AIDS, but he’s written a textbook supplement on HIV and AIDS and teaches a course at Davidson College on the subject. His students have even set up a blog discussing the history and science of HIV and AIDS. He also regularly lectures on the topic. I’ll be attending one of his talks tonight. Read more »
*This blog post was originally published at The Daily Monthly*
February 24th, 2010 by DaveMunger in Better Health Network, Expert Interviews, True Stories
No Comments »
“I like your watch,” pharmacist Jin Jun tells me as I’m sitting down to interview him.
I have a plastic runner’s watch, nothing special, but I see Jun is wearing something similar. “Do you run?” I ask him.
Jun is a tall, personable man who runs marathons, it turns out, and he enthusiastically invites me to run in a 5K race this weekend. I’m not sure I’ll be able to make it but I ask him for the details anyway.
Jun is equally passionate about his job, which one day a week involves helping the patients at the Carolinas Medical Center Infectious Disease Clinic with HIV drug adherence. I ask him how he handles cases like LaShana Walker’s, where some days she just doesn’t feel like taking her medications because they make her so nauseous. Read more »
*This blog post was originally published at The Daily Monthly*
December 2nd, 2009 by Dr. Val Jones in News, Opinion
No Comments »
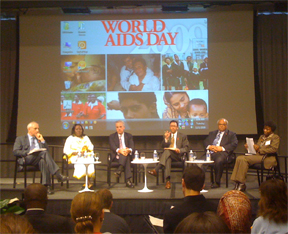
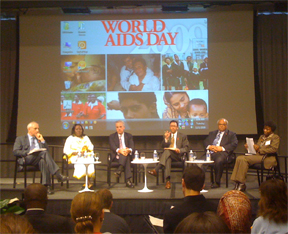 What does America’s economic recession have to do with a school teacher in Kenya? A lot more than you realize. If there’s one thing I learned at the World Bank’s World AIDS Day event yesterday, it’s that our lives, economies, and health are all inextricably intertwined on a global scale.
What does America’s economic recession have to do with a school teacher in Kenya? A lot more than you realize. If there’s one thing I learned at the World Bank’s World AIDS Day event yesterday, it’s that our lives, economies, and health are all inextricably intertwined on a global scale.
Beldina Atieno (second from the left in the photo) traveled all the way from Nairobi to offer her first hand account of life as an HIV+ school teacher in Africa. Ms. Atieno’s story was both heart-wrenching and eye-opening. She was first diagnosed after her youngest daughter became very ill from an opportunistic infection, which prompted HIV testing in both daughter and mother. After discovering that they were both positive, she was abandoned by her husband and was plunged into poverty and despair. Read more »
September 15th, 2009 by Bongi in Better Health Network, True Stories
No Comments »

 M and M was never fun. Sometimes I would walk out feeling I’d just escaped by the skin of my teeth. Sometimes I would feel like my teeth had had too close a shave. But once…just once, it could have been worse.
M and M was never fun. Sometimes I would walk out feeling I’d just escaped by the skin of my teeth. Sometimes I would feel like my teeth had had too close a shave. But once…just once, it could have been worse.
It was a pretty standard call. It was very busy. In the early evening I was called to casualties for a patient with severe abdominal pain. When I examined him it was clear there was something seriously wrong inside. He had a classical acute abdomen with board like rigidity. He clearly had a perforated peptic ulcer and needed surgery. I set my house doctor to work to get him admitted and on the list. Meanwhile I went back to theater to work through the number of equally critical patients already on the list.
Things then settled down into a rhythm. I was in theater with a student operating the cases one after the other while the house doctor separated the corn from the chaff in casualties. Finally it was time to do the laparotomy for the guy with the acute abdomen. I needed to shoot through casualties before we started so I decided to swing past the ward and make sure the guy was still ok.
The ward was dark. Pretty much everyone was asleep. Without wanting to wake the other patients I turned on the small bedside light of my patient. Even in that dim light I could see a bit of oral thrush. I was surprised. I was thinking to myself how the hell did I miss that in casualties. I felt his abdomen. It was no longer quite so tender. I turned to the student.
“See why it is important to make your decision before giving opioids?” I said with an air of authority. “Now he is actually not so tender but he definitely had an acute abdomen. We must go ahead with the operation.”
I quickly felt for lymph nodes. He had them everywhere. Once again I was quietly thinking that my clinical skills must be slipping because that I also didn’t pick up in casualties. I kept this new information to myself. Imagine the shock to the student if he realised I was not all knowing. i just didn’t want to be responsible for that level of devastation in his life. But I started considering other causes for his condition. It was clear he had AIDS and TB abdomen started looking like a possibility.
While we were still with the patient, the theater personnel arrived to take him to theater. I told them to get things going so long while I quickly shot down to casualties to evaluate a patient the house doctor was unsure about. And off I went at a brisk walk.
I walked into casualties. The house doctor led me to the patient in question, but as we approached his bed my blood went cold. In the exact bed where my acute abdomen had been lying about four hours previously was my acute abdomen still lying there!! I turned and ran back to theater. Fortunately I was in time.
Later I found out what had happened. Once we had admitted the acute abdomen, the porter had come in to take him to the ward. One of the patients lying in casualties was a guy that had just come in. His HIV had wreaked havoc in his life causing a number of unpleasant things, including AIDS dementia syndrome. The exchange went something like this;
“Timothy Mokoena? Is there a Timothy Mokoena here?” the porter called out.
“Here I am, but it’s not Mokoena. It’s Magagula.”
“Ok, Timothy Magagula, I’m going to take you to the ward.”
“Ok, but it’s not Timothy. It’s Michael.”
“Ok, Michael Magagula. Let’s go.”
And thus Michael Magagula, the AIDS dementia patient (not to be confused with Timothy Mokoena, the acute abdomen patient), thinking he had just jumped the queue to see a doctor was carted off to the ward and prepared for theater. He even signed for a laparotomy without even having seen a doctor.
In the end it all turned out well. Timothy got his operation and the hole in his stomach was patched. Michael was referred appropriately to the physicians. But I couldn’t help wondering how this could have looked in the next M and M meeting.
“Well, prof, the patient died on the table basically because I operated him unnecessarily.”
“And how is the other patient? The one you should have operated?”
“Well, he died too because I didn’t operate him.”
200% mortality for one operation. Not easy to achieve.

*This blog post was originally published at other things amanzi*