December 18th, 2011 by Toni Brayer, M.D. in Health Tips, News
2 Comments »

 Women have been told they should have screening for cervical cancer with a pap test every year. The visit to the gynecologist or internal medicine physician has been a right of passage for most young women and most are very compliant with that annual visit throughout their lives.
Women have been told they should have screening for cervical cancer with a pap test every year. The visit to the gynecologist or internal medicine physician has been a right of passage for most young women and most are very compliant with that annual visit throughout their lives.
Well, the times they are a-changin’ because new guidelines issued by the US Preventative Services Task Force and the American Cancer Society say women should undergo screening NO MORE OFTEN than every 3 years starting at age 21. To further strengthen this recommendation, even the American Society for Clinical Pathology (those folks that read the pap smears) agrees with the recommendation. They also recommend stopping routine pap smears after age 65 for women who have had 3 negative Pap test results in the past 10 years. These women are just not at high risk.
So why the change? Read more »
*This blog post was originally published at EverythingHealth*
December 3rd, 2011 by Elaine Schattner, M.D. in Opinion, Research
No Comments »

The latest issue of the Annals of Internal Medicine contains 2 noteworthy papers on cervical cancer screening. The first, a systematic review of studies commissioned by the USPSTF, looked at 3 methods for evaluating abnormalities in women over 30 years:
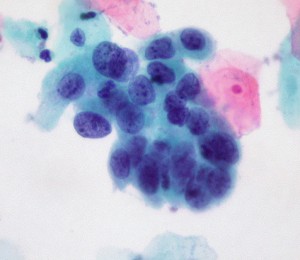
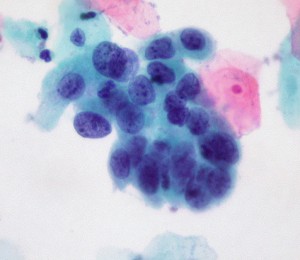
high-grade cervical cell dysplasia (Dr. E. Uthman, Wikimedia Commons)
1. Conventional cytology (as in a Pap smear; the cervix is scraped and cells splayed onto a microscope slide for examination);
2. Liquid-based cytology (for LBC, the NHS explains: the sample is taken as for a Pap test, but the tip of the collection spatula is inserted into fluid rather than applied to slides. The fluid is sent to the path lab for analysis);
3. Testing for high-risk HPV (human papillomavirus). Currently 3 tests have been approved by the FDA in women with atypical cervical cells or for cervical cancer risk assessment in women over the age of 30: Digene Hybrid Capture 2 (manufactured by Quiagen), Cobas 4800 HPV (Roche) and Cervista HR HPV (Hologic); another Roche Diagnostics assay, Amplicor HPV, awaits approval.
These HPV assays use distinct methods to assess DNA of various HPV strains.
There’s a lot of jargon here, and I have to admit some of this was new to me despite my nearly-due diligence as a patient at the gynecologist’s office and my familiarity as an oncologist with the staging, clinical manifestations and treatment of cervical cancer. Who knew so many decisions were made during a routine pelvic exam about which manner of screening? Read more »
*This blog post was originally published at Medical Lessons*
November 23rd, 2011 by Harriet Hall, M.D. in Opinion
2 Comments »

A recent announcement is likely to generate a lot of controversy. The Advisory Committee on Immunization Practices of the CDC has recommended that boys and young men be vaccinated against human papillomavirus (HPV). Previously the guidelines said boys “could” be given the HPV vaccine. Now they have recommended that boys age 11 to 12 “should” be vaccinated, as well as boys age 13 to 21 who have not already had the full series of 3 shots. The vaccine can also be given to boys as young as 9 and to young men age 22 to 26.
The vaccine was originally promoted as a way to prevent cervical cancer. Boys don’t have a cervix, so why should they be subjected to a “girl’s” vaccine? There are some good science-based reasons:
- Boys can transmit the virus to female sex partners later in life, leading to cervical cancer in women.
- More importantly, boys themselves can also be directly harmed by the virus. It can cause genital warts, cancer of the head and neck (tongue, tonsils and throat), anal and penile cancer, respiratory papillomatosis, and giant condyloma of Buschke and Lowenstein. In rare cases, immunocompromised patients can develop epidermodysplasia verruciformis.
- HPV has even been Read more »
*This blog post was originally published at Science-Based Medicine*
October 18th, 2011 by RyanDuBosar in Research
No Comments »

Oropharyngeal cancers caused by the human papillomavirus (HPV) are on the rise in the United States since 1984, as changes in sexual habits further the virus’ spread. But the focus of the HPV vaccine will remain on preventing genital warts and cervical cancer.
Reuters reported one clinician’s opinion that throat cancer linked to HPV will become the dominant cause of the disease, ahead of tobacco use.
To study the issue, researchers determined HPV-positive status among 271 of all 5,755 oropharyngeal cancers collected by the three population-based cancer registries in Hawaii, Iowa and Los Angeles from the Surveillance, Epidemiology, and End Results (SEER) program from 1984 to 2004. Prevalence trends across four calendar periods were estimated by using logistic regression. The study appeared online Oct. 3 in the Journal of Clinical Oncology.
HPV prevalence Read more »
*This blog post was originally published at ACP Internist*
March 2nd, 2011 by Jon LaPook, M.D. in News, Research, Video
2 Comments »
A new study finds that half of men in America are infected with the HPV virus. Dr. Jon LaPook reports on the growing concern that the virus in men could be responsible for an increase in head and neck cancers.
HPV Affects Half Of U.S. Men
A study out [yesterday] in The Lancet by Moffitt Cancer Center researcher Anna Giuliano, Ph.D., and her colleagues finds that 50 percent of men ages 18 to 70 in Brazil, Mexico, and the U.S. have genital infection with human papillomavirus (HPV). HPV is the virus that causes cervical cancer in women. It also causes warts and cancer of the genitals and anus in both men and women. Over the past several years, researchers have realized that the virus can also cause cancer of the head and neck.
Aimee R. Kreimer, Ph.D., of the National Cancer Institute, estimates that about 65 percent of the approximately 8,000 cancers of the tonsils and base of the tongue (oropharynx) seen in the U.S. in 2010 were from HPV infection; eighty percent of these are in men. The rates for HPV-associated cancers like these are increasing; for sites like the mouth and larynx that are associated with tobacco and alcohol use, the rates are decreasing (though still too high since too many people still smoke and abuse alcohol).
An infection rate of 50 percent for a virus that can cause cancer sounds scary. But knowing a few more facts about HPV helps put the risk in perspective. About 90 percent of men and women infected with HPV virus get rid of it on their own within about two years. There are many different strains of HPV — some that cause cancer and some that don’t. Only about 6 percent of men have genital infection with HPV 16 — the strain linked to more than 90 percent of cancers of the head and neck. And only about 0.6 percent of men have HPV 16 in specimens taken from their mouths; what percentage of those men go on to develop head and neck cancer is unknown. Read more »
 Women have been told they should have screening for cervical cancer with a pap test every year. The visit to the gynecologist or internal medicine physician has been a right of passage for most young women and most are very compliant with that annual visit throughout their lives.
Women have been told they should have screening for cervical cancer with a pap test every year. The visit to the gynecologist or internal medicine physician has been a right of passage for most young women and most are very compliant with that annual visit throughout their lives.