May 16th, 2016 by Dr. Val Jones in Opinion
No Comments »
 *This blog post was initially published on the Barton Blog.
*This blog post was initially published on the Barton Blog.
When doctors complete their residency training, they are under a lot of pressure to land their first “real job” quickly. Student loan deferments end shortly after training, and whopping debt faces many of them. But choosing a job that is a good long-term fit can be difficult, and gaining a broader exposure to the wide variety of options is key to success. That’s why “try before you buy” can be an excellent strategy for young physicians.
Locum tenens agencies such as Barton Associates work with healthcare organizations and practice locations across the country to offer a variety of temporary assignments for physicians.
These agencies negotiate your salary and call schedule. They also arrange the logistics, covering the costs of travel and accommodations. Once the doctor and the facility agree to terms, the physician simply arrives on the required date(s) and takes on the responsibilities requested. It’s a hassle-free, minimal-commitment arrangement that pays an hourly or daily rate for work.
Locum providers are given the convenient option to receive direct deposits to their bank accounts at regular intervals. Physicians can travel as broadly as they like for assignments, and the agency credentialing team works to efficiently complete any needed paperwork for new licenses and hospital privileging.
I enjoyed “living la vida locum” for six years before I landed my dream job. That’s a long time to be living out of a suitcase, and I doubt that most of my peers would want to do it for that long of a stretch. But an amazing thing happened during those years: With each new hospital experience, I gained insight and knowledge about my specialty. By rubbing elbows and networking with a wide swath of patients and experts across the country, I became a sought-after consultant in my own right.
I experienced different ways of delivering healthcare — from critical access hospitals to bustling academic centers. I learned about best practices and creative solutions that administrators and clinical staff had discovered to improve care quality, given the limitations of Medicare rules and private insurance restrictions.
When I was hired as the Medical Director of Admissions at St. Luke’s Rehabilitation Institute in Spokane, Washington, I came armed with creative ideas and a wealth of experience to draw from. I was a highly seasoned physician who had been exposed to the widest variety of patient populations and practice styles. I knew all about the unique struggles, successes, and solutions of various rehab centers across America. I now leverage that experience to drive change at my institution, and I am virtually unfazed by new problems and challenges.
The career value of locum tenens work is extraordinary. Take the time to look around you at each assignment. Learn what works and what doesn’t work, and file it away for future reference.
Like a bumblebee cross-pollinating hospital or medical practice “flowers,” locum tenens providers have the potential to drive change like no one else. When you’ve seen it all, your insights become invaluable, and you gain the maturity to know when a full-time job is the right cultural fit. Choosing the right job, on your terms and in your time, is the key to finding happiness in healthcare.
August 25th, 2015 by Dr. Val Jones in Health Tips
1 Comment »
 This post originally appeared on The Barton Blog.
This post originally appeared on The Barton Blog.
It’s both expensive and time-consuming to obtain temporary coverage for a hospital or medical practice. Locum tenens clients have every right to expect high-quality care from the locum tenens providers they hire; but even the very best locums may not perform to their full potential if their onboarding isn’t carefully planned.
As a locum tenens physician with licenses in 14 states, I have much experience with the onboarding process. Here are 12 tips for facilities eager to encourage smooth transitions, foster good provider relationships, and provide excellent patient care.
1. Arrange for provider sign-outs.
Since lapses in provider communication is a leading cause of medical errors, you can protect your patients by organizing a face-to-face (or phone call) report between the current provider and the locum who is going to be assigned to their census. Studies have shown a 30% decrease in error rate when physicians hand off their patient panel in person.
2. Allow for at least one day of training overlap, if possible.
The incoming provider will adapt best to your unique environment and care process if he or she has the chance to “shadow” the current provider for a day. Various questions will naturally arise and be answered during real-time patient care. In emergency fill situations, this will obviously not be possible; but it will help ease transitions in cases where it can be done.
3. Get your IT ducks in a row before the locum tenens provider arrives.
Electronic medical records (EMR) systems are difficult to master, and attempting to learn how to navigate in a new one (or newer version of one) in the middle of a full patient caseload is a recipe for disaster. Logins and passwords should be set up long before the locum tenens provider arrives. EMR training needs should be discussed and planned for in advance. If an IT professional is available to sit with the locum during his or her first round of documentation attempts, so much the better.
4. Plan for a day or half-day of orientation.
A facility tour, combined with an in-person meeting of key hospital players, is extremely important. The following people should be included:
- Unit medical director
- Nursing and therapy supervisors
- Risk management staff
- Human resources
- Medical records staff
- Coding and billing staff
- Pharmacy staff
- Laboratory staff
5. Prepare a welcome packet in advance.
This packet should include important information about the organization, the assignment, and the facility, including:
- Site maps
- Parking instructions
- Orientation day schedule
- Door key codes (if applicable)
- ID badge instructions
- EMR login and password
- Dictation codes
- Cafeteria location and hours
- A hospital directory with key phone numbers highlighted
Make sure the locum knows who signs their time sheets and where their office is located. A coding “cheat sheet” may also be appreciated.
6. Invite the locum tenens provider to lunch or dinner at some point during their assignment.
This is a friendly way to show that you appreciate them, and you want to get to know them. Being on the road can be lonely, and most locums appreciate opportunities to socialize.
7. …
– See more at: http://www.bartonassociates.com/2015/08/18/12-ways-to-help-your-locum-tenens-provider-succeed/#sthash.6KV0S3vE.dpuf
March 24th, 2015 by Dr. Val Jones in Opinion
No Comments »
 It’s no secret that physicians are experiencing burnout at an exponentially increasing rate in our progressively bureaucratic healthcare system. Many are looking for “alternative careers” as their salvation. I receive emails from physicians all the time, asking for advice about getting out of clinical medicine, since I have spent a few years outside it myself. As my own career pendulum has swung from full time clinical work to full time editorial and/or consulting work, I’ve found that the best mix is somewhere in between.
It’s no secret that physicians are experiencing burnout at an exponentially increasing rate in our progressively bureaucratic healthcare system. Many are looking for “alternative careers” as their salvation. I receive emails from physicians all the time, asking for advice about getting out of clinical medicine, since I have spent a few years outside it myself. As my own career pendulum has swung from full time clinical work to full time editorial and/or consulting work, I’ve found that the best mix is somewhere in between.
If you’re like me, you’re happiest using both halves of your brain. You have a creative side (I’m a cartoonist and blogger) and an analytic side (hospital-based physician). It’s not easy to make a living as a cartoonist or writer, and it’s soul-sucking to work 80 hour weeks in the hospital without rest. So how do you make a living, but participate in all the things you love? You work as a traveling physician (aka locum tenens) one third of your time, and spend the other two-thirds doing the creative things you also enjoy.
“But I couldn’t survive on 1/3 of my salary,” you say. Actually, I make the equivalent of a full-time academic physiatrist salary while working ~14 weeks a year as a traveling physician. Really? Yes, really. Because when I’m filling in at a hospital with an acute need, the work hours are long, and I’m paid by the hour. It can be grueling, but it is short, and the pay is fair so morale remains high. Drawing a flat employee salary (and then often discovering that the work load requires double the time estimated by the employer) can cause a lot of unconscious resentment. But when you are paid for your time, long hours aren’t as dread-worthy. This is what attorneys have been doing from day one, so why not physicians?
“But if all physicians suddenly dropped to half or 1/3 time, wouldn’t that do irreparable damage to patient access?” you cry. Yes, it could be catastrophic. However, if physicians stay the course and do nothing about our burnout, then the powers that be will continue tightening the vice – targeting physician reimbursement, increasing the burden of bureaucratic monitoring, pay for performance measures, and meeting “meaningless abuse” requirements for our electronic medical records systems. If there are no consequences to their actions, why would they ever stop?
I don’t think that most physicians will read this blog post and quit their jobs. I’m not worried about a sudden reduction in the physician work force. What I am offering is a suggestion for those of you who have a secret passion outside of clinical practice – a pathway that allows you to continue practicing medicine, and also enjoy cultivating your other talents. I’m hoping my advice will actually reduce the full drop out rate (if you believe the polls, up to 60% of PCPs would retire today if they had the means) to partial drop out rate (keeping those wanting to quit completely working part time).
So if there’s something you’ve always wanted to do (A non-profit endeavor? A low-paying, but rewarding job? Running a small business that can’t pay all the bills but is fun to do?) I say do it! Life is too short to get caught on the clinical treadmill, driving your spirits into the ground. You love your patients but can’t tolerate the work pace? Don’t quit altogether… you can still be a fantastic, caring, clinician in fewer hours/week and make the salary you need to maintain a reasonable lifestyle.
Please see my previous blog post to gain more insight into whether or not locum tenens might work for you.
And here’s a video of my recent thoughts about locum tenens work:
The Benefits Of Locum Tenens Work
September 15th, 2014 by Dr. Val Jones in Opinion
2 Comments »
 Judging from recent articles, surveys, and blog posts, the medical profession is remarkably demoralized. Typical complaints range from “feeling like a beaten dog” to “living in humiliating servitude,” to being forced to practice “treadmill medicine.” Interestingly, the public response to these complaints is largely indifferent. The prevailing attitude (if the “comments sections” of online articles and blog posts are representative) seems to be unsympathetic: “Poor doctors, making a little less income and not being treated like gods anymore? You have to do extra paperwork? You have to work long hours? Welcome to the real world, you whiners!”
Judging from recent articles, surveys, and blog posts, the medical profession is remarkably demoralized. Typical complaints range from “feeling like a beaten dog” to “living in humiliating servitude,” to being forced to practice “treadmill medicine.” Interestingly, the public response to these complaints is largely indifferent. The prevailing attitude (if the “comments sections” of online articles and blog posts are representative) seems to be unsympathetic: “Poor doctors, making a little less income and not being treated like gods anymore? You have to do extra paperwork? You have to work long hours? Welcome to the real world, you whiners!”
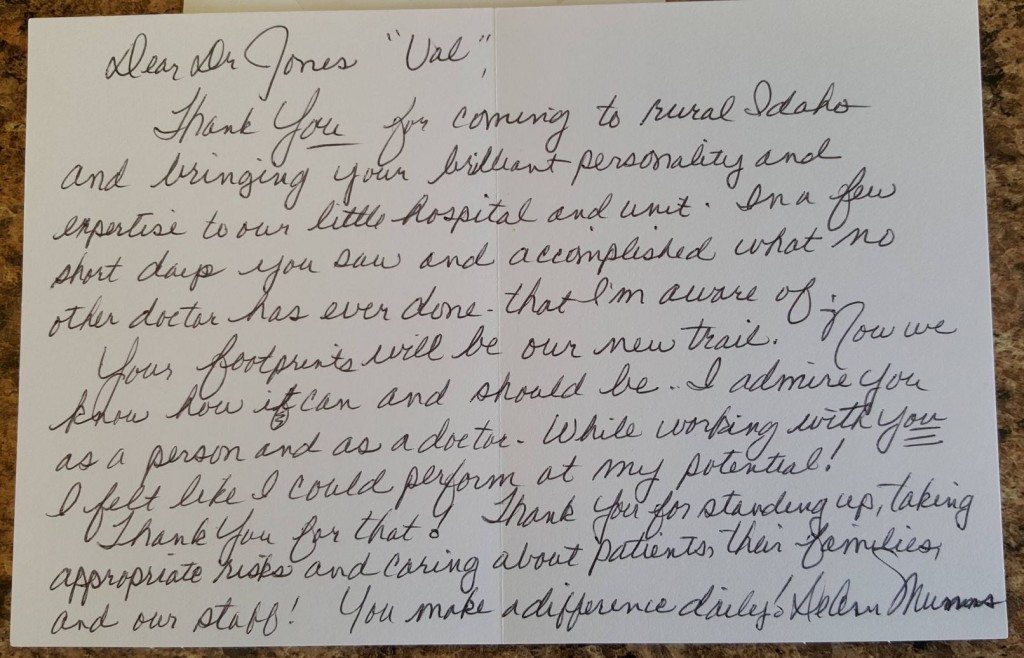
But thank goodness that practicing medicine is more nuanced than the Facebook stream of hostility that we are subjected to on a daily basis. If patients spoke to me the way online comments read, I’d surely have quit medicine years ago. But my reality is that patients are generally grateful, attentive, and respectful. This could be because I work in inpatient rehabilitation medicine, a place where patients are screened for motivation to participate in their care, but I don’t think that’s the whole story. I have experience working in other settings across the country (including Emergency Departments), and I have found a significant number of good-natured, engaged patients there too.
I think that to some degree our attitudes shape our work environments. Patient and peer dispositions are in part a reflection of our own. Try approaching a frightened, sick patient with an arrogant, dismissive tone and see how your professional relationship with them (and their families) develops. There is a negative cascade that physicians can trigger (perhaps unwittingly) when they are rushed, curt, or inattentive. Beginning every new patient relationship with a caring, respectful, detailed history and physical exam lays a foundation of trust for future interactions. Once you have established that positive rapport, the daily grind (along with what my friend, Dr. Steve Simmons, has nicknamed ‘C.R.A.P.P.’ – Continuous Restrictive And Punitive Paperwork) is much more bearable.
As physicians we have the power to make our careers as meaningful or soul-sucking as we choose. Reducing the C.R.A.P.P. in our work lives can help (I’ve tried outpatient, “concierge style” practices and inpatient locum tenens assignments with good success), but that’s not the most important factor in enhancing work satisfaction. The relationships built by allying ourselves with patients, and shepherding them through this broken system, are where the rewards lie. They hold the keys to our professional fulfillment because nothing can beat the joy of helping those in need.
How do I know that patient appreciation is enough to make medicine worthwhile?
Because I still don’t hate being a doctor.
 *This blog post was initially published on the Barton Blog.
*This blog post was initially published on the Barton Blog.


 It’s no secret that physicians are
It’s no secret that physicians are Judging from recent
Judging from recent 







