October 1st, 2009 by RamonaBatesMD in Better Health Network, True Stories
No Comments »

This topic has become more real for my family. My first cousin’s son-in-law committed suicide this past weekend. He had had difficulty adjusting since his return from Iraq, but the family was still caught off-guard. If you can make it any worse, he chose his wife’s birthday to take his life. Fortunately, neither she nor their toddler son was home at the time.
The issue of soldier suicide concerns many. Maj. Gen. William D. Wofford, Arkansas’ National Guard Adjutant General, recently made a public plea for help asking family members, friends and employers of the state’s 10,000 Guardsmen to watch for personality changes or signs of stress overwhelming his soldiers and airmen. There has been four suicides in Arkansas Guardsmen since January.
Read more »
*This blog post was originally published at Suture for a Living*
September 4th, 2009 by Paul Auerbach, M.D. in Uncategorized
No Comments »

 Michael Kilbourne and colleagues recently published an article entitled “Hemostatic Efficacy of Modified Amylopectin Powder in a Lethal Porcine Model of Extremity Arterial Injury”( Annals of Emergency Medicine 2009;53:804-810). The purpose of the study described in this article was to investigate the blood-stopping ability of a modified amylopectin powder in an animal (pig) model of severe limb bleeding created by an injury to the femoral artery.
Michael Kilbourne and colleagues recently published an article entitled “Hemostatic Efficacy of Modified Amylopectin Powder in a Lethal Porcine Model of Extremity Arterial Injury”( Annals of Emergency Medicine 2009;53:804-810). The purpose of the study described in this article was to investigate the blood-stopping ability of a modified amylopectin powder in an animal (pig) model of severe limb bleeding created by an injury to the femoral artery.
Following creation of the injury, animals were treated either with regular gauze with manual compression or with specially modified amylopectin powder and manual compression. Some of the endpoints measured in the study were total blood loss, survival, and time to bleeding cessation.
Post-treatment blood loss in the amylopectin powder-treated group was much less (approximately 0.275 liter) than in the gauze group (approximately 1.3 liters). Bleeding was stopped in approximately 9 minutes in the amylopectin group, and never stopped in the gauze group. 100% of the amylopectin animals survived, and none of the gauze animals survived.
While this study was directed to improve care for victims of major trauma (including wartime situations), the applicability to situations in the outdoors is direct. Many blood-stopping bandages have come to the civilian market, and they are quite useful. I carry them with me whenever I’m going into the wilderness, and often when I cover athletic events as the team doctor. They’re useful for nosebleeds and cuts, not just for severe injuries. Some of the product names include HemCon Bandage, QuickClot, BleedArrest, QR, Celox, and BloodStop. There will undoubtedly be improvements in these products, in particular the delivery systems, be they bandages or powders.
image courtesy of www.instructables.com
This post, Amylopectin Powder’s Amazing Ability Top Stop Hemorrhaging Fast, was originally published on
Healthine.com by Paul Auerbach, M.D..
June 9th, 2009 by KevinMD in Better Health Network
No Comments »

The military is learning from the dead.
In the past five years, every soldier who was killed in Iraq and Afghanistan has been given a CT scan. Why? In the hopes of creating a database of war injuries, which can be used to better equip and treat future soldiers.
The effort has already paid dividends. While examining the data, it was noticed that chest tubes used to treat pneumothoraces in the field were too short. The standard tubing would have been appropriate for 50 percent of soldiers, versus longer tubing that would fit 99 percent.
Also, it was because of these “autopsy scans” where it was noticed that many of the troops died from wounds in the upper torso, which could have been prevented with the appropriate body armor. On the basis of these findings, the military rushed more armor plates to Iraq.
It’s an interesting piece, and goes on to discuss the sensitive implications of the findings to family members:
The possibility that a relative burned to death is a particular source of anguish for families, and one area in which CT can outperform an autopsy. In a body damaged by flames, CT can help pathologists figure out whether the burns occurred before or after death. The scans can also tell whether a person found in water died from drowning.
It’s truly remarkable to see how much that can be learned after death.
*This blog post was originally published at KevinMD.com*
December 22nd, 2008 by Dr. Val Jones in Medblogger Shout Outs
No Comments »
Here’s my weekly round up of quotable quotes from my peers:
NHS Blog Doctor: Antibiotics do not cure snot. [Please go to the site for a fabulous illustrative photo.]
KevinMD: Since work-hours were restricted in 2003, there are no studies that have shown any marked improvements in patient safety or outcomes. Worse, errors have arisen from the so-called “patient hand-off,” the period of communication where rested doctors replaces those who are fatigued. Does increasing the frequency of patient hand-offs outweigh the benefit of better rested doctors?
Richard Reece, MD: The moral for doctors: Don’t expect as much leverage as in the past when negotiating with hospitals, even though you represent their main revenue stream.
Paul Levy: The medical community in Boston likes to boast about the medical care here, but we don’t do a very good job holding ourselves accountable.
Dr. Wes: Thanks to exorbitant costs of implementing EMRs in physician practices, the Medicare requirements for billing and prescribing electronically, and the prohibitive documentation requirements mandated by CMS in the name of “quality,” independent physician practices of all types will have no choice but capitulate to larger entities that have a fully integrated electronic medical record paired with collection software.
Heart found in a car wash (h/t Dr. Wes)
Ramona Bates, MD: I don’t think I would ever want to be part of doing a posthumous face lift or blepharoplasty or other cosmetic procedure, but I would be willing to debulk tumors if it would help families or individuals say “goodbye” more easily.
WhiteCoat Rants: For $79 you can blow into your iPod and it will play you a song if your blood alcohol is more than 0.08. You know this device wasn’t made for parents.
Just what we need. A bunch of drunk teenagers farting around with their iPods and getting into a “who can get the highest blood alcohol” contest.
The Happy Hospitalist: It frightens me to hear people say they want to work in medicine and work in a similar capacity as physicians, evaluating, diagnosing and managing disease, but not want to put in the time and sacrifice to be residency trained in depth and scope…
Science-Based Medicine: Our soldiers, grievously wounded in combat, deserve only the best science-based therapy available… If I were to propose treating our injured soldiers with bloodletting and toxic metals (both common methods in the 1700s and early 1800s) based on the concept that it would put the “imbalance of the four humors” back into balance, the Pentagon and the military medical establishment would toss me out on my ear as a dangerous quack–and rightly so. But introduce a method that claims “ancient Chinese wisdom” based on somehow magically redirecting the flow of a mysterious “life energy” by sticking small needles into parts of the body that correspond to no known anatomic structures through which “qi” flows, and suddenly the Air Force is funding a program to train medics and physicians treating our wounded soldiers how to do this method based on the same amount of convincing scientific evidence that qi exists as for the four humors (none) and in the face of no strong clinical evidence that it’s any better than a placebo.
Rural Doctoring: Hospitalists, take note: this is an example of why people go ape-sh*t crazy in the hospital:
• Her right arm is completely immobilized to protect the graft site.
• Her left arm has a heplocked IV in it.
• Half her head is shaved because the surgeon took the donor skin from the scalp.
• She’s vegetarian and the cafeteria sent her chicken for lunch.
• Dinner was vegetarian but she can’t really cut up a baked potato with only one hand.
• The hospital has double rooms and is running at capacity, so the staff is harried.
• Her roommate is an elderly, demented woman who keeps trying to get out of bed by herself and objects to the TV being on. So far, all she’s said to us is “Mind your own business!”
November 10th, 2008 by Dr. Val Jones in News, Opinion
2 Comments »
“My daddy’s in Iraq, but he’s not dead yet.”
— 5-year-old son of a US Marine
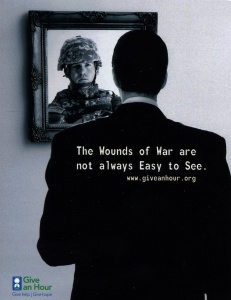
Roughly 1.7 million Americans have been deployed to Iraq so far. An estimated 320,000 US military have received a traumatic brain injury in the Iraq war. Another 300,000 suffer from major depression or post traumatic stress disorder. The VA is not equipped to handle the mental health needs of all returning veterans and their families. What can we do?
The Give An Hour organization has challenged mental health professionals to donate 1 hour of their time/week to serve the needs of the military. If only 1 in 10 providers joined the program, there would be enough hours to cover the unmet needs.
I met with Dr. Barbara Romberg today to discuss her plans for the program. She envisions an in-office, phone, and online platform for Give An Hour. I sure hope that I can help out with the online platform one day.
If you’re a mental health professional, please consider joining the Give An Hour initiative. Our troops risked their lives for us, and others have sustained life-long injuries – some visible, some invisible.
And there are little boys out there, wondering if this is the day their daddy will die.
Let’s consider how we can be of comfort to those who are suffering on this Veterans Day.