December 3rd, 2010 by StevenWilkinsMPH in Better Health Network, Health Tips, Opinion, Research
1 Comment »

“I recommend.” These are two word which, when spoken by a physician to a patient have tremendous power to change behavior. That assumes of course a trusting relationship between patient and physician (but that’s a topic for another day.)
Take the colonoscopy. The U.S. Preventive Services Task Force (USPSTF) recommends that adults aged ≥50 years get a colonoscopy every 10 years. In 2005, 50 percent of adults aged ≥50 years in the U.S. had been screened according to these recommendations. Not surprisingly, the rate of colonoscopy screening is much lower than that of other recommended adult preventive services. I was curious: Why?
Here are two interesting facts:
1. Studies show that patients cite “physician recommendation” as the most important motivator of colorectal screening. In one study, 75 to 90 percent of patients who had not had a colonoscopy, said that their doctor’s recommendation would motivate them to undergo screening.
2. In that same study, in 50 percent of patients where a colonoscopy was appropriate but not done, the reason given was that the physician simply did not “bring up” the subject during the visit. Reasons included lack of time, visit was for acute problem, patient had previously declined or forget. Read more »
*This blog post was originally published at Mind The Gap*
November 18th, 2010 by StevenWilkinsMPH in Better Health Network, News, Opinion, Research
No Comments »

What do cell phones and health-information seeking have in common? Very little, at least among the chronically ill (e.g., the folks who are driving healthcare use and cost). An American Medical News article about the latest Pew Research Center’s Internet & American Life Project study on mobile phone use caught my eye. The introduction to the article reads:
Despite the proliferation of cell phones in the United States, the number of people using them to access health information is low. But experts believe the sheer number of people using mobile phones and wireless devices means that health information eventually will get more mobile as well.
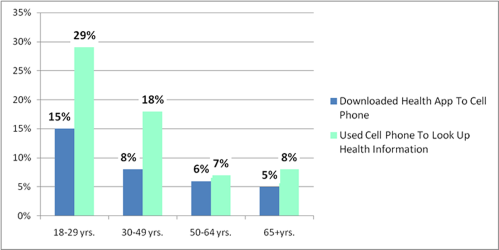
According to the study, 85 percent of Americans use mobile phones, but only 17 percent of cell phone owners have used them to look up health information. Nine percent of Americans have downloaded a health-related app on their cell phone.
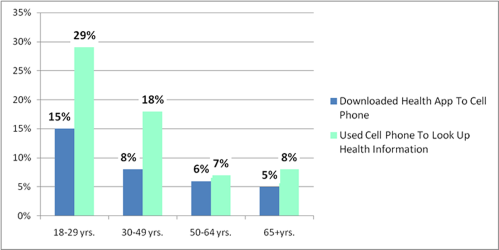
Get this: The highest use of cell phone health-information seeking and downloading cell phone health apps was among 18- to 29-year olds at 29 percent and 15 percent respectively. With the exception of accidents, 18- to 29-year-old adults are generally among the most healthy demographic. Read more »
*This blog post was originally published at Mind The Gap*
November 2nd, 2010 by StevenWilkinsMPH in Better Health Network, News, Opinion, Research
No Comments »

Over the last year or two, lots of people have been jumping on the social media bandwagon, i.e., Twitter, Facebook, and so on. There has been a lot of talk about how social media and social networking will revolutionize healthcare, but little evidence to back this talk up. Until now, that is.
Before I get to the evidence that I referred to, I need to clarify something. The goal of social media as I understand it is to get people talking, sharing information and creating new ideas. As applied to healthcare, one of the goals of social media is to get people/patients with like medical conditions taking, sharing and supporting one another. Healthcare researchers refer to this phenomenon as peer support. Peer support is not new to healthcare. Disease-specific support groups (breast cancer, diabetes, etc.) have been around for years. “Group” physician office visits comprised of patients with the same diagnosis have been around for years as well.
The Study
Now to the evidence. As anyone with a chronic condition or who treats patient with chronic conditions knows, patient self-care is critical. Knowledge, skills and confidence are prerequisites for effective self-care management. Read more »
*This blog post was originally published at Mind The Gap*
October 6th, 2010 by StevenWilkinsMPH in Better Health Network, Health Tips, Research, True Stories
No Comments »

A 69-year-old woman who swims in my master program came back to the pool after a total knee replacement. I asked her how she was doing. She said she is still in a lot of pain because of her physical therapy. She said that her physical therapist was disappointed that she still was still unable to achieve full flexion of 120 degrees. Why 120 degrees? Did you set that goal I asked her? “No,” she said, “the therapist did.”
She went on to tell how she already had more range of motion in her knee than she did before the surgery. My friend was quite satisfied with her progress and wanted to stop physical therapy. The pain from the PT was worse than anything she had experienced before the knee replacement. I knew she and her 80-year-old boy friend were going on a cruise and she didn’t want to still be hobbling around.
It turns out that patients and physicians disagree on quite a few things. We hear a lot about patient-centered care. You know, that’s where the provider is supposed to consider the patient’s needs, preferences, and perspective when diagnosing and treating health problems. But medicine is still very provider-centered. Read more »
*This blog post was originally published at Mind The Gap*