November 26th, 2012 by Dr. Val Jones in Health Tips, Opinion, Research
5 Comments »
 A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
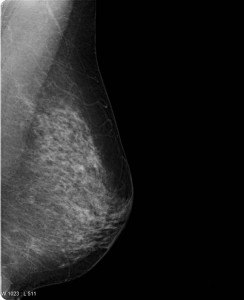
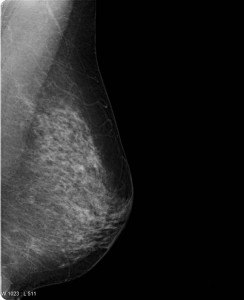
A question on most women’s minds (as they turn 40 and beyond) is whether or not they should get a screening mammogram (x-ray of the breasts). If you have found a lump in your breast or you have a family history of breast cancer the answer is yes. No need to read any further. However, for the majority of us lumpless, family-history-free women, a screening mammogram is far more likely to expose us to unnecessary follow up testing than it is to catch a tumor early. Dr. Welch explains that screening mammograms aren’t very good at identifying aggressive breast cancer early enough to make a difference in whether one lives or dies anyway. That’s very disappointing news.
Dr. Welch goes on to explain that most of the gains we’ve made in breast cancer survival have been because of improved breast cancer treatments, not because of early detection with mammograms. He estimates that every year in the U.S. 1.3 million women are “over-diagnosed” with breast cancer because of screening mammograms, subjecting women to unnecessary biopsies, surgical procedures, and further follow up studies. In the video, Dr. Welch doesn’t explain exactly what these “over diagnosed” cancers end up being exactly (Cysts? Benign calcifications? Early non-aggressive cancers that the immune system kills on its own?) But suffice it to say that they don’t contribute to the cancer death rates.
So, given the fact that you are more likely to suffer through a false alarm than to discover a cancer early (and even if you do find it early, if it’s the “bad” kind you may not survive) are you willing to undergo a screening mammogram? That’s a personal question that we each have to answer for ourselves. As time goes on, however, I suspect that the answer will be made for us since health insurance companies (whether public or private) will begin to balk at paying for tests that do more harm than good overall. I think this issue is really at the heart of the controversy (the perception of rolling back a health benefit that women currently “enjoy”). Eventually screening mammograms may become an out-of-pocket expense for women who simply prefer the peace of mind that a normal test can give – even at the risk of going through a false alarm.
That being said, it sure would be great if we could find a screening test that identifies breast cancer early – especially the aggressive kind. Perhaps a blood test will do the trick one day? At least it is comforting to know that we have made great strides on the treatment side, so that fewer women than ever before die of breast cancer. More research is needed on both the screening and treatment sides of course.
As for me, I do regular breast self exams – though because I have no family history of breast cancer I’ve opted out of screening mammograms because I feel the cost/benefit ratio is not in my favor. I certainly hope that a better screening test is developed before I face a potential diagnosis. I respect that other women will disagree with me – and I think they have the right to be screened with the only option we currently have: the mammogram. I’m not sure how long it will continue to be covered by insurance, but at a price point of about $100, most of us could still afford to pay for it out-of-pocket if desired.
The bottom line of this controversial research study is that screening mammograms don’t actually catch death-causing breast cancers early enough to alter their course. Even though it makes intuitive sense to be screened, long term observations confirm that overall, mammograms do more harm than good. So now we wait for a better test – while some of us continue with the old one (as the National Cancer Institute recommends), and others (like me) don’t bother.
***
Thanks to ePatient Dave and Susannah Fox who brought the issue to my attention on Facebook. Isn’t social media grand?
June 10th, 2011 by Peggy Polaneczky, M.D. in Health Tips
No Comments »

 In a large multicenter study enrolling over 70,000 women, annual screening with transvaginal pelvic ultrasound and ca125 blood testing did not reduce deaths from ovarian cancer, and in fact led to an increase in complications due to screening.
In a large multicenter study enrolling over 70,000 women, annual screening with transvaginal pelvic ultrasound and ca125 blood testing did not reduce deaths from ovarian cancer, and in fact led to an increase in complications due to screening.
Investigators in the NCI-sponsored Prostate, Lung and Ovarian Cancer (PLCO) Screening trial randomly assigned over 78,000 women age 55-64 years of age to either annual screening with transvaginal pelvic sonograms for 4 years plus CA125 testing for 6 years or usual care at 10 study sites across the US., and followed the groups for up to 13 years. Over that time period, ovarian cancer rates in the screened group were 5.7 per 10,000 person-years vs 4.7 per 10,000 persons-years in the usual care group, with 3.1 deaths vs 2.6 deaths per 10,000 person years, respectively. Over 3000 women had false positive screening results, a third of whom had surgery and 15% of those operated on had a complications from their surgery. Deaths from other causes did not differ between the groups.
The investigators concluded that annual screening for ovarian cancer does not reduce mortality, and in fact caused harms among women with fals positive abnormal results.
This is not the first study that failed to find efficacy for ultrasound and ca125 in reducing mortality from ovarian cancer, but Read more »
*This blog post was originally published at The Blog That Ate Manhattan*
March 14th, 2011 by RyanDuBosar in Better Health Network, Research
No Comments »

The number of cancer survivors in the United States increased to 11.7 million in 2007, according to a report released by the Centers for Disease Control and Prevention (CDC) and the National Cancer Institute (NCI), part of the National Institutes of Health (NIH). Women survive more often, and survive longer, according to the report.
There were 3 million cancer survivors in 1971 and 9.8 million in 2001. Researchers attributed longer survival to a growing aging population, early detection, improved diagnostic methods, more effective treatment and improved clinical follow-up after treatment.
The study, “Cancer Survivors in the United States, 2007,” is published today in the CDC’s Morbidity and Mortality Weekly Report.
 To determine the number of survivors, the authors analyzed the number of new cases and follow-up data from NCI’s Surveillance, Epidemiology and End Results Program between 1971 and 2007. Population data from the 2006 and 2007 Census were also included. The researchers estimated the number of persons ever diagnosed with cancer (other than non-melanoma skin cancer) who were alive on Jan. 1, 2007. Read more »
To determine the number of survivors, the authors analyzed the number of new cases and follow-up data from NCI’s Surveillance, Epidemiology and End Results Program between 1971 and 2007. Population data from the 2006 and 2007 Census were also included. The researchers estimated the number of persons ever diagnosed with cancer (other than non-melanoma skin cancer) who were alive on Jan. 1, 2007. Read more »
*This blog post was originally published at ACP Internist*
March 2nd, 2011 by Jon LaPook, M.D. in News, Research, Video
2 Comments »
A new study finds that half of men in America are infected with the HPV virus. Dr. Jon LaPook reports on the growing concern that the virus in men could be responsible for an increase in head and neck cancers.
HPV Affects Half Of U.S. Men
A study out [yesterday] in The Lancet by Moffitt Cancer Center researcher Anna Giuliano, Ph.D., and her colleagues finds that 50 percent of men ages 18 to 70 in Brazil, Mexico, and the U.S. have genital infection with human papillomavirus (HPV). HPV is the virus that causes cervical cancer in women. It also causes warts and cancer of the genitals and anus in both men and women. Over the past several years, researchers have realized that the virus can also cause cancer of the head and neck.
Aimee R. Kreimer, Ph.D., of the National Cancer Institute, estimates that about 65 percent of the approximately 8,000 cancers of the tonsils and base of the tongue (oropharynx) seen in the U.S. in 2010 were from HPV infection; eighty percent of these are in men. The rates for HPV-associated cancers like these are increasing; for sites like the mouth and larynx that are associated with tobacco and alcohol use, the rates are decreasing (though still too high since too many people still smoke and abuse alcohol).
An infection rate of 50 percent for a virus that can cause cancer sounds scary. But knowing a few more facts about HPV helps put the risk in perspective. About 90 percent of men and women infected with HPV virus get rid of it on their own within about two years. There are many different strains of HPV — some that cause cancer and some that don’t. Only about 6 percent of men have genital infection with HPV 16 — the strain linked to more than 90 percent of cancers of the head and neck. And only about 0.6 percent of men have HPV 16 in specimens taken from their mouths; what percentage of those men go on to develop head and neck cancer is unknown. Read more »
February 28th, 2011 by Elaine Schattner, M.D. in Opinion, Research
No Comments »

There’s a new study out on mammography with important implications for breast cancer screening. The main result is that when radiologists review more mammograms per year, the rate of false positives declines.
The stated purpose of the research*, published in the journal Radiology, was to see how radiologists’ interpretive volume — essentially the number of mammograms read per year — affects their performance in breast cancer screening. The investigators collected data from six registries participating in the NCI’s Breast Cancer Surveillance Consortium, involving 120 radiologists who interpreted 783,965 screening mammograms from 2002 to 2006. So it was a big study, at least in terms of the number of images and outcomes assessed.
First — and before reaching any conclusions — the variance among seasoned radiologists’ everyday experience reading mammograms is striking. From the paper:
…We studied 120 radiologists with a median age of 54 years (range, 37–74 years); most worked full time (75%), had 20 or more years of experience (53%), and had no fellowship training in breast imaging (92%). Time spent in breast imaging varied, with 26% of radiologists working less than 20% and 33% working 80%–100% of their time in breast imaging. Most (61%) interpreted 1000–2999 mammograms annually, with 9% interpreting 5000 or more mammograms.
So they’re looking at a diverse bunch of radiologists reading mammograms, as young as 37 and as old as 74, most with no extra training in the subspecialty. The fraction of work effort spent on breast imaging –presumably mammography, sonos and MRIs — ranged from a quarter of the group (26 percent) who spend less than a fifth of their time on it and a third (33 percent) who spend almost all of their time on breast imaging studies. Read more »
*This blog post was originally published at Medical Lessons*
 A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.
A recent mammogram study in the New England Journal of Medicine was so controversial that the authors (Drs. Welch and Bleyer) decided to make a YouTube video to defend and explain their conclusions. Now that’s a first, isn’t it? Well kudos to the study authors for their creative approach to getting ahead of a controversy. However, their video (created for the “general public”) is still a bit too technical in my opinion. I’d like to take a crack at distilling it further.














