January 28th, 2011 by Elaine Schattner, M.D. in News, Opinion
1 Comment »

The FDA [has] issued an alert about a possible link between breast implants — saline or silicone — and a rare form of lymphoma called anaplastic large cell lymphoma (ALCL). These lymphoma cases are exceedingly rare, but the association appears to be significant.
The FDA identified a total of approximately 60 ALCL cases in association with implants, worldwide. Of these, 34 were identified by review of published medical literature from 1997 to May, 2010; the others were reported by implant manufacturers and other sources. The agency estimates the number of women worldwide with breast implants is between five and 10 million. These numbers translate to between six and 12 ALCL cases in the breast, per million women with breast implants, assessed over 13 years or so.
In women who don’t have implants, ALCL is an infrequent tumor, affecting approximately one in 500,000 women is the U.S. per year. This form of lymphoma — a malignancy of lymphocytes, a kind of white blood cell — can arise almost anywhere in the body. But ALCL cases arising in the breast are unusual. The FDA reports that roughly three in 100,000,000 women are diagnosed with ALCL in the breast per year in the U.S.
These are very small numbers. Still, the finding of ALCL tumors by the implant capsules is highly suggestive. Almost all of the implant-associated ALCL cases were T-cell type, whereas most breast lymphomas are of B-cell type. The lymphomas arose in women with both silicone and saline-type implants, and in women with implants placed for purposes or augmentation and for reconstruction after mastectomy. Read more »
*This blog post was originally published at Medical Lessons*
January 26th, 2011 by Elaine Schattner, M.D. in Health Tips, Opinion
No Comments »

A few years ago I started writing a book on what it was like to be a cancer patient and an oncologist. This morning I came upon this section on second opinions:
Is It OK To Get A Second Opinion?
Definitely. And there’s no need to be secretive about it, or to worry about hurting the doctor’s feelings. Second opinions are routine in fields like oncology, and are often covered by insurance. Be up-front: Any decent oncologist can understand a cancer patient’s need to find a doctor who’s right for them, with whom they’re comfortable making important decisions. And in difficult cases, some specialists appreciate the chance to discuss the situation with another expert. So a second opinion can be beneficial to patients and physicians alike.
When things can get out of hand, though, is when patients start “doctor shopping.” For example, I’ve cared for some patients with leukemia who’ve been to see over 10 oncologists. If you’re acutely sick, this sort of approach to illness can be counterproductive — it can delay needed therapy. From the physician’s perspective, it’s alienating: Who wants to invest her time, intellectual effort, and feelings for a patient who’s unlikely to follow up? Besides, oncology is the sort of field where each consulting doctor may have a distinct opinion. (If you see 10 oncologists, you may get 10 opinions.) Beyond a certain point, it may not help to get more input, but instead will cloud the issue. Read more »
*This blog post was originally published at Medical Lessons*
January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
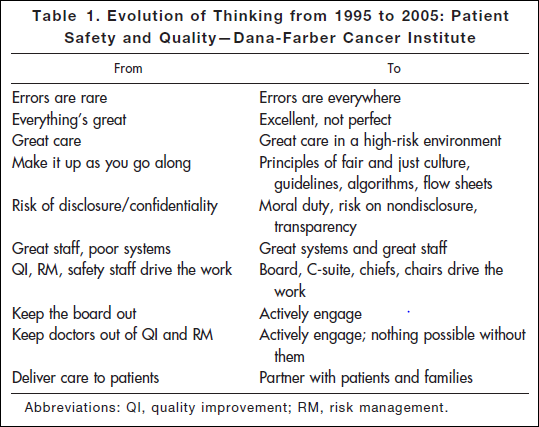
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
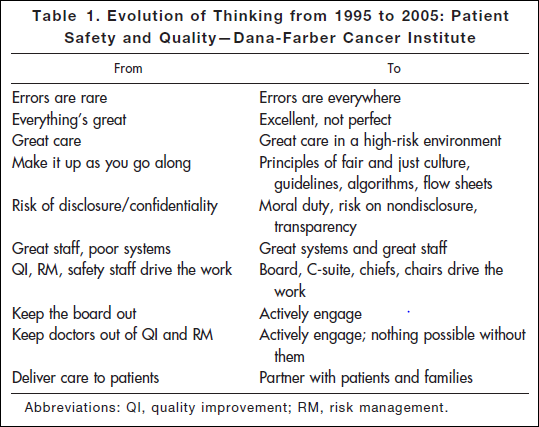
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*
January 19th, 2011 by GarySchwitzer in Better Health Network, Opinion
No Comments »

That’s the question Dartmouth’s Dr. Gil Welch asks in a column on the CNN website. He reflects on [recent] news about a test in development that might find a single cancer cell among a billion healthy ones — as so many news stories framed it. Welch analyzes:
“But it’s not that simple. The test could just as easily start a cancer epidemic.
…
Most assume there are no downsides to looking for things to be wrong. But the truth is that early diagnosis is a double-edged sword. While it has the potential to help some, it always has a hidden side-effect: overdiagnosis, the detection of abnormalities that are not destined to ever bother people in their lifetime.
Becoming a patient unnecessarily has real human costs. There’s the anxiety of being told you are somehow not healthy. There’s the problem that getting a diagnosis may affect your ability to get health insurance. There are the headaches of renewing prescriptions, scheduling appointments and keeping them. Finally, there are the physical harms of treatments that cannot help (because there is nothing to fix): drug side-effects, surgical complications and even death. Not to mention it can bankrupt you.
Americans don’t need more diagnoses, they need the right diagnoses.
I don’t know whether this test will help some patients. It might, but it will take years to figure that out. Read more »
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*