January 29th, 2011 by KerriSparling in Health Tips, True Stories
No Comments »

Recently, I reconnected with a long-lost local PWD (person with diabetes) named Ryan. Last time Ryan and I saw one another we were talking about diabetes goal-setting and dealing with wicked bouts of burnout. And this week I received an email from him with a brilliant idea about how to stay motivated towards setting — and reaching — diabetes-related goals.
“I’ve had this ‘pyramid’ for about three months now. Just something that I keep near my desk to keep me focused on my diabetes. After completion of the pyramid, I have no clue what I will do but some kind of celebration will be in order,” he wrote, and attached a slide to his image. And when I opened it, I was like “whoa.”
He had created a pyramid of his diabetes goals. Tangible goals — real-life goals — that are both achievable and ambitious, all at once. I thought this was so clever because it is a constant but non-threatening reminder of what diabetes goals are most top-of-mind for him. (Also, having a celebration at the end of that pyramid completion sounds like a quality idea. Perhaps a Fudgy the Whale?)
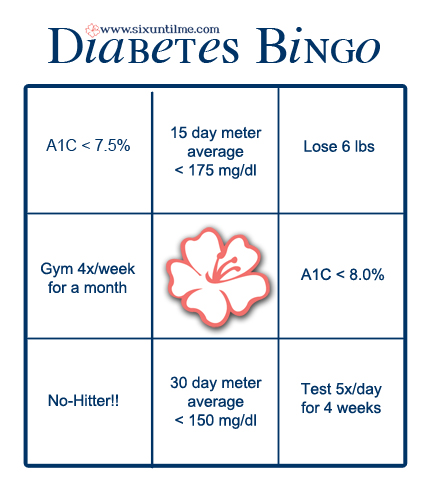
I’ve been working towards gaining better control of my diabetes (and overall health) lately, and I love the idea of something I can print out, stick to my fridge, and remain inspired by. I liked the idea of a pyramid, but I kept picturing a huge bingo hall in my mind, with a whole bunch of PWDs sitting at the tables with glucose tabs and bingo markers at the ready. But the trick wasn’t getting four in a row, it was filing the whole card.
I thought about my own personal goals and created this:
There are a few not-necessarily-diabetes-related goals on there (like “lose 6 pounds,” which is because I’m still trying to de-flump), but there are a lot of diabetes goals that aren’t unique to my particular circumstances. Since I’m trying to emerge from some diabetes burnout, my goals aren’t as tight as they were a few months ago (i.e. the slow progression from an A1C over 8 to one under 7.5). But these are real, and I’m hoping to fill the card within six months. Thanks for the fun idea, Ryan!
What would be on your bingo card?
*This blog post was originally published at Six Until Me.*
January 27th, 2011 by Linda Burke-Galloway, M.D. in Health Tips, Opinion
No Comments »

 The journey to a healthy pregnancy and delivery begins with the selection of a healthcare provider, and the challenge is to find the right one. This is the person who will be in charge of your pregnancy up until the time of the delivery, so it certainly is not a casual date. For the next 280 days your life and the life of your unborn child will be in this person’s hands. A background check is therefore in order.
The journey to a healthy pregnancy and delivery begins with the selection of a healthcare provider, and the challenge is to find the right one. This is the person who will be in charge of your pregnancy up until the time of the delivery, so it certainly is not a casual date. For the next 280 days your life and the life of your unborn child will be in this person’s hands. A background check is therefore in order.
One of the best ways to find the right healthcare provider is by word-of-mouth referral from neighbors, friends, or family members however please don’t stop there. Labor and delivery nurses are also a great source of referral because they have seen physicians and midwives under their most vulnerable and challenging moments.
Don’t feel intimidated about checking a provider’s credentials — this is public information. You can find out whether the provider’s medical license is current or expired. You’ll also be able to obtain information on whether the provider has ever been disciplined by the board for medical malpractice or unprofessional behavior or misconduct. Healthcare providers are not exempt from problems with alcoholism, drug addiction, professional incompetence, and unprofessional or unethical behaviors. Although less than five percent of healthcare providers have egregious problems, you want to make certain that your provider is not one of them. Read more »
*This blog post was originally published at Dr. Linda Burke-Galloway*
January 26th, 2011 by Elaine Schattner, M.D. in Health Tips, Opinion
No Comments »

A few years ago I started writing a book on what it was like to be a cancer patient and an oncologist. This morning I came upon this section on second opinions:
Is It OK To Get A Second Opinion?
Definitely. And there’s no need to be secretive about it, or to worry about hurting the doctor’s feelings. Second opinions are routine in fields like oncology, and are often covered by insurance. Be up-front: Any decent oncologist can understand a cancer patient’s need to find a doctor who’s right for them, with whom they’re comfortable making important decisions. And in difficult cases, some specialists appreciate the chance to discuss the situation with another expert. So a second opinion can be beneficial to patients and physicians alike.
When things can get out of hand, though, is when patients start “doctor shopping.” For example, I’ve cared for some patients with leukemia who’ve been to see over 10 oncologists. If you’re acutely sick, this sort of approach to illness can be counterproductive — it can delay needed therapy. From the physician’s perspective, it’s alienating: Who wants to invest her time, intellectual effort, and feelings for a patient who’s unlikely to follow up? Besides, oncology is the sort of field where each consulting doctor may have a distinct opinion. (If you see 10 oncologists, you may get 10 opinions.) Beyond a certain point, it may not help to get more input, but instead will cloud the issue. Read more »
*This blog post was originally published at Medical Lessons*
January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
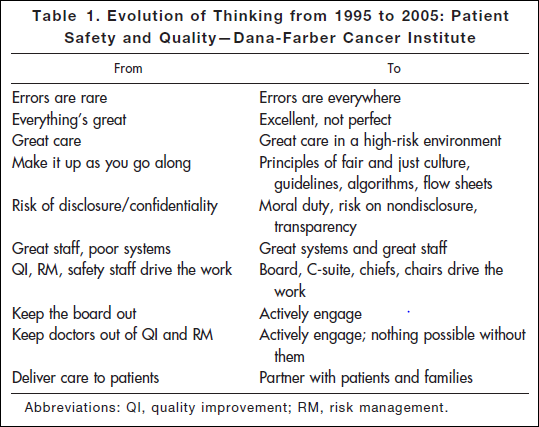
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*