May 27th, 2009 by ValerieTinleyNP in Primary Care Wednesdays
No Comments »
A report just released on HealthReform.gov, the website for the Obama Administration’s healthcare reform effort, is entitled Roadblocks To Healthcare: Why The Current Health Care System Does Not Work For Women, and cites that more than half of American women (52%) delay or avoid care because of cost, compared to 39% of men.
A video synopsis of the report, hosted by Kathleen Sebelius, the Secretary of Health and Human Services, states that women are being left behind when it comes to healthcare and that there are over 21 million uninsured women in the U.S. Young women have much more difficulty finding affordable health insurance than do men and often pay higher premiums – sometimes one and a half times – those of a young man. These facts all add up to women not getting the care they need to stay healthy.
As a primary care provider (PCP) focusing on women’s health, the findings of the report don’t surprise me, not even a little. From my anecdotal studies of the number of women that I have seen over the years, the majority of women struggle to receive the care they need because they cannot afford it. What typically will happen is that these women delay, often for years, any type of check-up or preventive care because of costs. Instead, they wait until they are sick or are having issues, and then they are forced to find the money and the time to seek medical care.
I also have found another factor beyond price that is creating a barrier to healthcare for women, and the word is “convenience.” Many women cannot, or often will not, take the time to seek routine medical care when most doctor’s offices are open, which is nine to five. Frequently these women are working, albeit on jobs that offer them little or no healthcare coverage, and are loathe to take time off of work for a non-emergency medical issues. Women also have the lion’s share of childcare responsibility, and are more likely to put their children’s schedules and family needs well before theirs.
Primary care can be the first place to look for a solution in bringing affordable, convenient care to women so that there are no roadblocks to access. We strive to do just this at our practice. Our Well Women Clinics were spearheaded after much deliberation about cost and convenience. We started last year and have found them to be a great success. For these clinics, we designated specific days during the month for routine well women check-ups. Hours for these check-ups are early morning through lunch one day and mid-afternoon through evening on another days. We offer the clinics two days each month on different days of the week, ideally making times available for each patient’s schedule, whether she is a current patient with us or a new one.
Although the biggest hurdle for women to getting the care may be cost, as the Obama Administration’s report cites, let us not forget the role that convenience in getting this care plays. Healthcare and wellness does not have a nine-to-five schedule. Likewise, most women’s roles beyond possibly those in a regular “office” job are not on such a regimented schedule; their roles as caretakers and mothers have round-the-clock demands. We need to work with women determine and then remove all of the roadblocks to accessing of care, starting first and foremost with cost, moving to convenience and then considering others that may exist.
Until next week, I remain yours in primary care,
Valerie Tinley, MSN, RNFA, FNP-BC
May 13th, 2009 by AlanDappenMD in Primary Care Wednesdays
No Comments »
“OK,” I can hear you say, “Enough about telemedicine. So what if you can prevent two-thirds of office visits by using the phones, or that it’s convenient for the patient and can start them on the road to recovery faster, or that it costs much less money than conducting an office visit, or that malpractice companies have accepted this delivery model.
I can see that you still side with the other non-believers in telemedicine, citing, “Telemedicine is no way to build relationship with patients. Problems abound with telemedicine: It’s too impersonal, patients could easily not be telling you the truth because you lose the “body language and facial expressions,” and it certainly can’t be useful for chronic illness. Maybe it’s good for the simple problems, but this has no place with complex or chronic medical care.”
I do, of course, have some rebuttals for you …
Let’s start with impersonal. In today’s world, we let our friends and family communicate with us constantly through phones and email, and I’ve yet to see how this has destroyed the intimacy of our relationships. So why do Americans anxiously wait up to four days for a doctor’s appointment to get their problem or question resolved and waste at least four hours of a day to get to the office simply to wait for an unpredictable time for a predictable 10-15 minutes of the doctor’s time when so many issues can be resolved remotely by phone? Furthermore, try convincing someone with a urinary tract infection (UTI) or that needs a prescription refill that their long wait, suffering, and run through the primary care funnel were “good for the relationship.” In fact, nothing is more personal that a doctor saying to their patients, “Here is my direct phone number, please call me anytime you need help.” Viewing telemedicine from this perspective determines that the “impersonal” concern is a ruse to protect doctor’s privacy at the expense of their patients.
What about the patient who is not truthful? Does a face-to-face visit make this less likely? In 30 years of work, several patients I know have not always been honest. Many of these people were attractively dressed, well educated and for awhile, fooled me badly. I saw them all face to face too. To this day, I have no idea what to look for when someone is trying to pull the wool over my eyes.
If people are going to hide the truth, they can do it in person just as well as over the phone. When a doctor becomes suspicious about a patient’s truthfulness through a pattern of calls and behaviors, then a scheduled office visit may help. However, forcing office visits based on a blanket rule of thumb of not trusting your patients means there is something fundamentally wrong with the doctor-patient relationship.
Lastly is the idea that chronic disease management isn’t appropriate through phones and email. Really? Let’s say you had diabetes, or hypertension, or high cholesterol, or cancer, or depression, just to name a few. With one of these conditions, you will be in contact with your health professional a lot more than you are now. Not only is your life more complicated, but the doctor wants you to consume 10% of your life waiting to see him in person because it’s good for him. Instead, many of these visits can be conducted easily anytime through phone calls and email.
Here are some examples:
#1. A phone call: “Mr. Doe this is Dr Dappen. I see a calendar reminder that you’re due for labs to check your cholesterol and to make sure the statin drug we put you on is not causing problems. I’ve faxed the order to the lab that is located close to you home, so stop by anytime in the next week and they’ll draw the blood. I should have the results in 24 hours after your visit to the lab, and we can review the report over the phone at that time and decide if we need to make any change.”
#2. An email from a patient: “Dr. Dappen, I’ve been worrying about my blood pressure readings. Over the past 3 weeks, they’ve been running consistently higher. Not sure why and until recently the home readings were doing great. Attached is the spread sheet of readings. Look forward to your input.”
In fact, examples abound of how chronic disease management conducted via phones and email is more efficient, reduces costs, and improves outcomes; I’d invite any Doubting Thomas to visit the American Telemedicine Association for further inquiry. An entire telemedicine industry is gearing up to manage chronic illnesses and most of the time it has nothing to do with patients visiting doctors’ offices.
When all is said and analyzed, the conclusion is really simple as to why the use of telemedicine is not more prevalent: no one wants to pay a doctor the market value for the time it takes to answer a phone and expedite an acute problem or manage a chronic health care problem. No money means no mission. This means no phones, no email. Don’t think about it. See you in the office. Why ruin 2400 years of tradition?
April 29th, 2009 by AlanDappenMD in Primary Care Wednesdays, Uncategorized
3 Comments »
In early 2006, four years into running my current medical practice, doctokr Family Medicine, I got a call from my medical malpractice carrier. Just weeks before I’d received a notice that my malpractice rates could go up by more than 25%. The added news of a pending investigatory audit was chilling. In 25 years of practicing medicine I’d never been audited.
“Is there a complaint, or a law suit against me that I don’t know about?”
“No,” the auditor told me over the phone, “We’ve never seen a medical practice like yours and feel obligated to investigate your process from a medical-legal perspective.”
“Great,” I thought, with a weary sigh. “I’m already battling the insurance model, the status quo of the medical business model, and slow adoption by consumers who are addicted to their $20 co-pay. All I’m trying to do is to breathe life into primary care and get the consumer a much higher quality service for less money than currently subsidized through the insurance model. And now this.”
The time had arrived to add the concerns of the malpractice companies to the list of hurdles to clear if a new vision of a medical care model was ever to catch flight.
I frequently am asked the question “Aren’t you afraid of the malpractice risk?” when I explain my medical practice model, which is based on the doctor answering the phone 24/7, resulting in the patient’s medical problem being solved by the phone more 50% of the time. The simplest counter to this question is to analyze the risk patients incur when the doctor won’t answer the phone. What happens when the doctor is the LAST person to know what’s going on with patients? The answer is obvious. But malpractice companies could have concerns beyond patient safety. Buy-in from the malpractice companies would be critical to the future viability of all telemedicine.
I prepared a summary paper, which included 12 bullet points, explaining how a doctor- patient relationship based on trust , transparency, continuous communications and high quality information systems significantly reduce risk to the person you’re trying to help.
Bullet 1: The industry standard is that 70% of malpractice cases in primary care center on communication barriers. My medical team deploys continuous phone and email communications and 7 days a week- same day office visits when needed between doctor and patient thus significantly reducing these barriers.
.
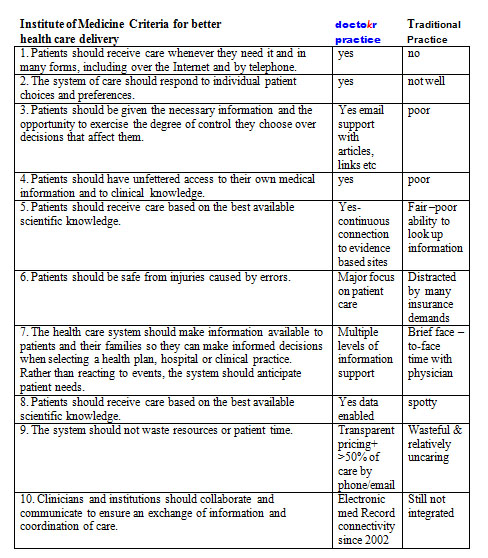
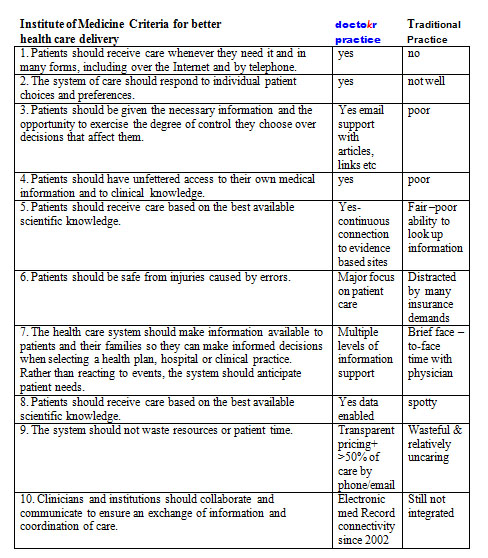
The remaining bullets could be summarized by the conclusions from the Institute of Medicine’s visionary book Crossing the Quality Chasm: A New Health System for the 21st Century using a table developed by The American Medical News when they reviewed the book. I carefully plotted our practice standards compared to the traditional business model as it stands today based on this table:
The auditor showed up, spent 4 hours reviewing our practice, electronic medical records, compliance to HIPPA, our intakes, on-line connectivity, procedures, and practice standards. While the auditor reviewed, I sat as unobtrusively as I could, feeling my brow grow damp with perspiration, as I carefully answered her questions. During the auditor’s time, I never moved to sway her to “my way.” I just let the data that I had accumulated from four years of practice do the talking.
Once the auditor left, I waited for two weeks for the results. By the time their letter arrived, I was scared to open it. The news arriving made me jubilant. The medical practice company announced a DECREASE in my premiums because we used telemedicine and EMR to treat patients so fast (often within 10 minutes of someone calling us we have their issue solved without the patient ever having to come in).
I will admit that I felt, and actually still do feel, vindicated by having my malpractice insurer understand fully the value that the type of telemedicine my practice offers to our patients: round-the-clock access to the doctor, speed of diagnosis, and convenience, which all led to healthier patients and lower risk.
Doctors answering the phone all day for their patients, it’s not just lower risk, it’s better health care at a better price. It’s a win-win-win strategy whose day is arriving.
Until next week, I remain yours in primary care,
Alan Dappen, MD
April 22nd, 2009 by AlanDappenMD in Primary Care Wednesdays
No Comments »
By: Valerie Tinley, MSN, RNFA, FNP-BC
House calls have long been associated with primary care providers (PCPs), the proverbial “black bag,” and days gone by. Unfortunately, house calls are often just a memory or something we watch in reruns on the television.
Those people that best remember the prevalence of house calls, the elderly, may be the same population whose needs will bring house calls back from the brink of extinction and return them to the mix of services offered by PCPs.
House calls should be a core offering of PCPs, since by nature we help patients from cradle to grave. Therefore, some of these patients may not be able to come to see us because they are too old or too sick or immobile.
Why then can’t PCPs go to these patients? We certainly can solve the majority of primary care problems where our patients want or need to be seen, including in their homes, whether these problems are run of the mill day-to-day issues; or those associated with chronic, continuous care diseases; or even many urgent care issues.
Unfortunately house calls are rarely offered because many PCPs view them as too time consuming and therefore too costly to conduct.
The need for house calls for these populations will not go away. The populations that house calls can help include:
• those that are bed bound, very old, who want to age at home rather than a nursing home;
• those suffering from dementia;
• those recently discharged from the hospital, and unable to be mobile short term or long term; and
• those that are receiving hospice care.
Many of these people cannot leave their home, or more importantly, should not leave the home, to go to the doctor’s office for an office visit. It is important to understand how very expensive this is for the caregiver, in terms of time, lost hours on the job, effort and transportation costs, all to actually get them to the medical provider’s office, because their loved ones have problems with mobility or other hindrances.
The result? There are many in need of medical care that cannot receive it. This increases medical problems and mortality. When healthcare is ignored or foregone for the most routine of problems, more expensive and much more serious healthcare issues arise in its place.
A recent article in the New York Times reported that keeping geriatric patients out of the hospital and getting them the care the need at home can result in a cost savings of between 30% and 60%. In addition, a house call program, piloted by Duke University, has reduced the number of hospital admissions for those patients unable to get to the doctors office by 68% and the number of emergency room admissions by 41%. These patients are thereby healthier, and even safer, working with a PCP that makes house calls.
Several organizations currently offer house calls as a core part of their services offerings, like Urban Medical in Boston, or the practice I am with, doctokr Family Medicine. Also there are beginnings of pilot programs for house calls, like the one at Duke’s Medical School which was mentioned earlier.
But these are only a few providers, and the movement needs to be widespread. Our aged population needs it and we as primary care providers should be listening to their needs and providing for these needs. Otherwise, we are falling short.
Until next week, I remain yours in primary care,
Valerie Tinley MSN, RNFA, FNP-BC
April 15th, 2009 by AlanDappenMD in Primary Care Wednesdays
No Comments »
The most revolutionary tool in primary health care, for almost all out patient care for that matter, is something so common, so mundane, so overlooked that it’s like the nose on your face, you never see it. This tool is not the computer, the internet or a killer software application.
It’s the phone. Why? The answer is equally as simple: The phone allows for 24/7 communication between a doctor and patient who know each other. Likewise, the patient can access the health system with an expert from anywhere and most of the time get what they need.
The American Telemedicine Association (ATA) estimates that 70% of medical problems can be resolved with phones. Almost everyone thinks phone medicine is reserved for an arctic explorer or a poor citizens living in Timbuktu. This assumption ignores how life transforming it would be for every American citizen to pick up a phone, and expect to speak to their doctor anytime from anywhere, at work, on the metro, even on travel, or vacation and expect to resolve their issue instantaneously! No wait, no hassle, no waiting room, no bureaucracy. At least 70% of the time it should be that easy!
Telephone medicine is not to be misconstrued for talking to a stranger. It is not impersonal, nor meant to avoid seeing patients. In reality, it is simply one way of many to get good health care. Sometimes you need a hospital, an emergency room, a specialist, an office visit. However, more than half the time you only need a phone visit, preferably with a doctor or medical practice you know and trust. Even emails are appropriate at times.
That telephones could so easily replace more than 50% of all office visits is so unexamined, so foreign, so shocking, that a predictable series of objections arise:
1. If it was so safe why isn’t it being done already? Of course this begs the reality that our health care system doesn’t pay — or underpays — a doctor to do this. It’s as simple as following the money. Right now the money is in seeing you, so an office visit it must be.
Doctors also answer phones on weekends and night. In fact more than half of the week they are practicing “free telemedicine care,” and that means phone medicine has more real time, more experience in any week than office visit time. It’s just been always deemed “free.” No money means no mission. The doctor, saying, “We’ll schedule you an office visit,” is code for, “Come on in so I can get paid.” That’s a business fact!
2. Isn’t the doctor afraid that he/she’ll miss something? First, office visits miss things all the time. For the sake of not missing something, shouldn’t it mean every problem needs doing a full body scan, complete blood work, and parading every medical problem in front of three separate specialists. If each problem was hospitalized too, maybe that would mean not missing something.
The answer of course, is that to every problem there is a season of reasoning; a triage of appropriateness. Many problems arise where physical exam is irrelevant. If you or the doctor thinks you should be seen, then a face-to-face visit should be arranged but when both people agree what’s going on and that an office visit is not needed, then a phone visit makes sense, which is true over 50% of the time.
3. Isn’t it dangerous for a doctor to answer the phone? To which no one asks the converse question: What’s the experience when the doctor doesn’t answer the phone? If this occurs, then the most knowledgeable person about healthcare, becomes the LAST person to know. This means exposure to the Hippocrates business model of care: long delays, hassled waits, rushed visits. Illness is not a static problem but evolves. The reality of how you feel this minute in front of the doctor often is rendered irrelevant tomorrow when something dramatically changes “Waiting and communicating change” is critical to medical decision making and treatment. Most doctors bring you back in to “see how you’re doing” and make sure they get paid again. It’s not the doctors’ fault, It’s the way the system pays them.
4. Telemedicine, doesn’t that mean higher chances for malpractice? You’ll love the answer to this, but that will need to wait ‘til next week.
Until next time, I remain yours in primary care,
Alan Dappen, MD