April 29th, 2009 by AlanDappenMD in Primary Care Wednesdays, Uncategorized
3 Comments »
In early 2006, four years into running my current medical practice, doctokr Family Medicine, I got a call from my medical malpractice carrier. Just weeks before I’d received a notice that my malpractice rates could go up by more than 25%. The added news of a pending investigatory audit was chilling. In 25 years of practicing medicine I’d never been audited.
“Is there a complaint, or a law suit against me that I don’t know about?”
“No,” the auditor told me over the phone, “We’ve never seen a medical practice like yours and feel obligated to investigate your process from a medical-legal perspective.”
“Great,” I thought, with a weary sigh. “I’m already battling the insurance model, the status quo of the medical business model, and slow adoption by consumers who are addicted to their $20 co-pay. All I’m trying to do is to breathe life into primary care and get the consumer a much higher quality service for less money than currently subsidized through the insurance model. And now this.”
The time had arrived to add the concerns of the malpractice companies to the list of hurdles to clear if a new vision of a medical care model was ever to catch flight.
I frequently am asked the question “Aren’t you afraid of the malpractice risk?” when I explain my medical practice model, which is based on the doctor answering the phone 24/7, resulting in the patient’s medical problem being solved by the phone more 50% of the time. The simplest counter to this question is to analyze the risk patients incur when the doctor won’t answer the phone. What happens when the doctor is the LAST person to know what’s going on with patients? The answer is obvious. But malpractice companies could have concerns beyond patient safety. Buy-in from the malpractice companies would be critical to the future viability of all telemedicine.
I prepared a summary paper, which included 12 bullet points, explaining how a doctor- patient relationship based on trust , transparency, continuous communications and high quality information systems significantly reduce risk to the person you’re trying to help.
Bullet 1: The industry standard is that 70% of malpractice cases in primary care center on communication barriers. My medical team deploys continuous phone and email communications and 7 days a week- same day office visits when needed between doctor and patient thus significantly reducing these barriers.
.
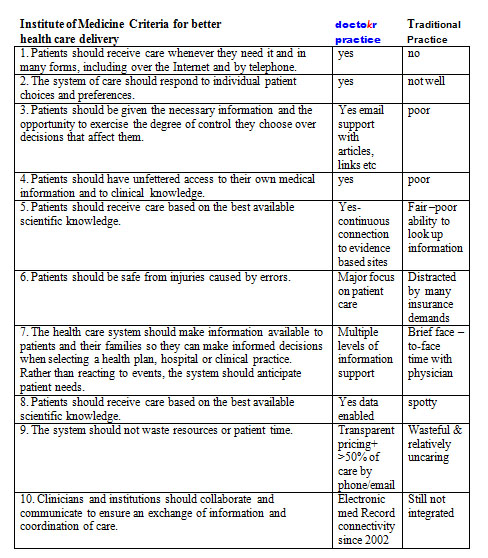
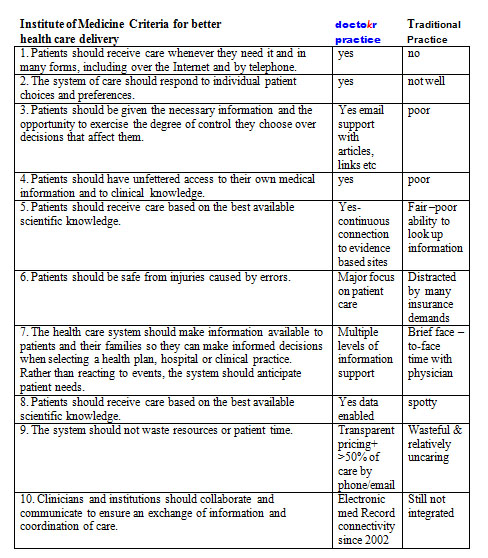
The remaining bullets could be summarized by the conclusions from the Institute of Medicine’s visionary book Crossing the Quality Chasm: A New Health System for the 21st Century using a table developed by The American Medical News when they reviewed the book. I carefully plotted our practice standards compared to the traditional business model as it stands today based on this table:
The auditor showed up, spent 4 hours reviewing our practice, electronic medical records, compliance to HIPPA, our intakes, on-line connectivity, procedures, and practice standards. While the auditor reviewed, I sat as unobtrusively as I could, feeling my brow grow damp with perspiration, as I carefully answered her questions. During the auditor’s time, I never moved to sway her to “my way.” I just let the data that I had accumulated from four years of practice do the talking.
Once the auditor left, I waited for two weeks for the results. By the time their letter arrived, I was scared to open it. The news arriving made me jubilant. The medical practice company announced a DECREASE in my premiums because we used telemedicine and EMR to treat patients so fast (often within 10 minutes of someone calling us we have their issue solved without the patient ever having to come in).
I will admit that I felt, and actually still do feel, vindicated by having my malpractice insurer understand fully the value that the type of telemedicine my practice offers to our patients: round-the-clock access to the doctor, speed of diagnosis, and convenience, which all led to healthier patients and lower risk.
Doctors answering the phone all day for their patients, it’s not just lower risk, it’s better health care at a better price. It’s a win-win-win strategy whose day is arriving.
Until next week, I remain yours in primary care,
Alan Dappen, MD
April 15th, 2009 by AlanDappenMD in Primary Care Wednesdays
No Comments »
The most revolutionary tool in primary health care, for almost all out patient care for that matter, is something so common, so mundane, so overlooked that it’s like the nose on your face, you never see it. This tool is not the computer, the internet or a killer software application.
It’s the phone. Why? The answer is equally as simple: The phone allows for 24/7 communication between a doctor and patient who know each other. Likewise, the patient can access the health system with an expert from anywhere and most of the time get what they need.
The American Telemedicine Association (ATA) estimates that 70% of medical problems can be resolved with phones. Almost everyone thinks phone medicine is reserved for an arctic explorer or a poor citizens living in Timbuktu. This assumption ignores how life transforming it would be for every American citizen to pick up a phone, and expect to speak to their doctor anytime from anywhere, at work, on the metro, even on travel, or vacation and expect to resolve their issue instantaneously! No wait, no hassle, no waiting room, no bureaucracy. At least 70% of the time it should be that easy!
Telephone medicine is not to be misconstrued for talking to a stranger. It is not impersonal, nor meant to avoid seeing patients. In reality, it is simply one way of many to get good health care. Sometimes you need a hospital, an emergency room, a specialist, an office visit. However, more than half the time you only need a phone visit, preferably with a doctor or medical practice you know and trust. Even emails are appropriate at times.
That telephones could so easily replace more than 50% of all office visits is so unexamined, so foreign, so shocking, that a predictable series of objections arise:
1. If it was so safe why isn’t it being done already? Of course this begs the reality that our health care system doesn’t pay — or underpays — a doctor to do this. It’s as simple as following the money. Right now the money is in seeing you, so an office visit it must be.
Doctors also answer phones on weekends and night. In fact more than half of the week they are practicing “free telemedicine care,” and that means phone medicine has more real time, more experience in any week than office visit time. It’s just been always deemed “free.” No money means no mission. The doctor, saying, “We’ll schedule you an office visit,” is code for, “Come on in so I can get paid.” That’s a business fact!
2. Isn’t the doctor afraid that he/she’ll miss something? First, office visits miss things all the time. For the sake of not missing something, shouldn’t it mean every problem needs doing a full body scan, complete blood work, and parading every medical problem in front of three separate specialists. If each problem was hospitalized too, maybe that would mean not missing something.
The answer of course, is that to every problem there is a season of reasoning; a triage of appropriateness. Many problems arise where physical exam is irrelevant. If you or the doctor thinks you should be seen, then a face-to-face visit should be arranged but when both people agree what’s going on and that an office visit is not needed, then a phone visit makes sense, which is true over 50% of the time.
3. Isn’t it dangerous for a doctor to answer the phone? To which no one asks the converse question: What’s the experience when the doctor doesn’t answer the phone? If this occurs, then the most knowledgeable person about healthcare, becomes the LAST person to know. This means exposure to the Hippocrates business model of care: long delays, hassled waits, rushed visits. Illness is not a static problem but evolves. The reality of how you feel this minute in front of the doctor often is rendered irrelevant tomorrow when something dramatically changes “Waiting and communicating change” is critical to medical decision making and treatment. Most doctors bring you back in to “see how you’re doing” and make sure they get paid again. It’s not the doctors’ fault, It’s the way the system pays them.
4. Telemedicine, doesn’t that mean higher chances for malpractice? You’ll love the answer to this, but that will need to wait ‘til next week.
Until next time, I remain yours in primary care,
Alan Dappen, MD
April 8th, 2009 by AlanDappenMD in Primary Care Wednesdays
No Comments »
Back in 1983, as a third year medical student, I read a study stating that 80% of medical visits were not needed. After finishing the text, I remember thinking, “Hmm, there aren’t that many hypochondriacs in our office!”
It wasn’t until I had practiced medicine for 20 years that I finally understood this statement for what it really meant: doctors were not helping patients through remote means, instead insisting on seeing patients in the office for all medical issues, even the most routine of issues out of habit, out of fear, out of how to get paid.
In 1996, I set out to prove that allowing established patients to remotely access doctors for care would improve their medical outcomes. I convinced my medical partners to let me conduct an experiment: I would work a few half days on the phones, fielding medical-related calls from our HMO patients. Since HMO plans paid us a flat rate to take care of them, bringing these patients to the office cost us money and offering these patients medical consults by phone instead, for routine issues, would be more cost-effective for us and a lot more convenient for them.
At that time, the front desk fielded over 500 patient calls a day. I sat next to the four receptionists, and the HMO screened patients with straightforward medical problems would be triaged to me. I then would speak to the patient, review their medical history and address their medical issue and get them what they needed. I was able treat 90% of the screened patients I spoke over the phone, while determining that the other 10% needed face-to-face appointments. During a typical 3.5 hour shift, I routinely spoke to 25 patients, and immediately helped 23 of those patients with their medical issues thereby avoiding an office visit.
Unfortunately, the experiment didn’t last long. To the business managers of the practice, we lost $500 in co-pays while I logged half days on the phone, not billing a single dollar for the practice. Where I saw opportunity and a new paradigm, they saw lost income.
Thus, I returned to my routine day, seeing 25 patients a day in person, day after day. But drudgery of this led to deepening despair. So many unnecessary office visits, patients upset with their delays, apologies for running late, and meetings about how to see more patients, see them faster, charge the insurance companies more. In some cases all the delays had led to a complication that could have been avoided with more timely care.
Not undeterred, I discretely planned a study in 1999. For two weeks I collected data on each patient I saw. Recording data on a laptop during each visit, I analyzed three questions: How long did we talk, how long did the exam take, how often did I already know what to do through history alone and not due to findings from the face-to-face exam.
Here are the results: I saw an average of 23 patients a day. The longest office visit was 45 minutes, and the longest physical examination of a complicated patient took 10 minutes. Sixty-six percent of my patient visits had no reason to be in the office, with my diagnosis relying on patient history and not being influenced by my physical exam.
On reflection of the data, the implication of the data awoke me to a new realization. I must step outside the “Matrix” that I had been a part of: a healthcare system that often delayed and even held hostage 2 of 3 patients I saw each day.
But making the decision to step outside this system was not easy: why should I risk my medical career as I knew it, and my financial security to do what is best for my patients and deliver them the quality they care they needed?
It was my wife, who, in 2001, finally convinced me to move on. She wrote a resignation letter to my medical practice, a practice filled with respected friends and colleagues. As I sat pondering the risk I’d confront by handing in the letter, my wife reminded me of a familiar refrain, “Ships are safe at harbor, but that’s not what ships are for.”
And so, in 2002, I founded doctokr Family Medicine, a practice that does step outside the typical paradigm of healthcare. My patients control how and when they are seen by our medical team. At doctokr, all of the patients establish their care through a face-to- face visit at the office. We gather their history, review their records and do an exam. After that, all established patients are free to email or call the doctor directly, 24/7. Over half of patients’ issues are resolved remotely, via phone or email. Our medical team also sees patients if they want to be seen, or if we feel we need to see them 7 days a week.
As a medical practice with 3000 pioneering patients, we sail on empty oceans but with full faith that we will not have done so in vain. Our experience has shown happier and healthier patients, providers with a mission and passion again and pricing that is 50% less than the current system price of healthcare.
For doctors and patients, staying “safe” behind the many unexamined assumptions in health care makes such harbor risky indeed.
Until next week, I remain yours in primary care,
Alan Dappen, MD
April 1st, 2009 by AlanDappenMD in Primary Care Wednesdays
2 Comments »
Imagine yourself a patient 2400 years ago. By chance, Dr. Hippocrates is your “preferred provider.” You and Dr. Hippocrates have a long standing relationship, and you’ve seen him in person many times, including for a comprehensive check-up and medical history. Since his office is located 20 miles away, getting there requires a Herculean effort. With the help of friends, donkeys, walking and several days of delay you luckily arrive before closing time at 4 pm on Wednesday. You remember well the weekends, the evenings and the holidays that you got to the office sicker than a dog, only to be left in the street until the clinic re-opened.
When you arrive, many sick patients greet you, their expressions fatalistic. All have made similar journeys, and some are very sick. A line strings out the waiting room door that is two hours long. Dr. Hippocrates is rushing to finish the day’s work, see the last person and go home to supper and his family. With so many people to see and not much time, Hippocrates flies through the patient histories, relying only on his memory, knowledge and expertise to prescribe treatments and cures, moving quickly from one patient to the next.
For you, an herb is prescribed and you make the arduous journey home. Two days later you’re feeling worse. Maybe it’s the herb, maybe it’s the wrong diagnosis, maybe it’s the exhaustion from the ordeal. Yet one thing is for sure, taking the trip back to Hippocrates is too daunting to consider.
Fast forward to present day, and consider yourself as patient. Fortunately, the science of medicine has changed exponentially. Sadly the business model and the experience of getting that care is egregiously similar. Every time you need to use health care in today’s world, a gauntlet of obstacles stands between you and the service. First, there’s the receptionist answering the phone, then the scheduler fitting you into a limited number of times to come to the office, with all available slots being at least two days in the future. Upon arriving at the office, a waiting room stuffed full of sick patients greets you. Next, the person at the in-window verifies your insurance eligibility. On to the nurse who greets and reviews your history, then a wait again for the hurried doctor to rush in, and in 10 minutes or less, reduce your problem to a prescription. You’re ushered out and to the window where the co-pay is made and next a follow-up visit scheduled. The bill proceeds to the billing specialist and somewhere along the way (often months later) you might get an insurance adjustment charge. The next day you wake up with a rash. Maybe it’s the drug, maybe it’s the wrong diagnosis, but taking that trip back through that system is going to give you pause and it’s not just the pause of your time or life interrupted. For most day-to-day health care this story has repeated itself ad infinitum from antiquity until today.
A huge unexamined question in primary health care revolves around the requirement of “forced” office visits. Why do you think you are going to the obligatory ritual of the office visit for every medical problem be it a prescription refill, poison ivy rash, allergic runny nose, tick bite, urinary tract infection among thousands of other problems. Do medical experts really need to “see” you to protect you, themselves, or build a relationship?
The answer to this conundrum once analyzed is simple: No. As a matter of fact, the majority (over 50%) of routine primary care health problems can be taken care remotely, by phone, email, IM, or even online chat, if the doctor and patient have a pre-existing relationship. And why don’t more primary care practitioners use the convenience of remote access to get their patients the fastest initial and follow-up treatments possible? It’s about the money. Insurance companies pay a doctor to help you by seeing you face-to-face. Since doctors are beholden to insurance companies payments to cover the cost of your visit and since your copay doesn’t even get close to covering the cost of running the business. So the primary docs elect to put you through The Funnel.
When the idea is first suggested, most people disbelieve that phone consultation alone between a doctor and patient could handle more than 50% of the medical issues sent through the funnel of the mandatory office visit gauntlet. Don’t misread this, talking with your doctor doesn’t mean that you don’t need to be seen in person sometimes too. Likewise, all patient-doctor relationships should begin first with a face-to-face visit, complete with check-up and the discussion of the patient’s prior medical history. However, just open your eyes to the possibility of a new idea. I’ll let this uncomfortable thought settle in for while and will check back on your progress in my next post.
Until next week I remain yours in primary care,
Alan Dappen, MD