Telemedicine Care: A malpractice risk? Au Contraire …
In early 2006, four years into running my current medical practice, doctokr Family Medicine, I got a call from my medical malpractice carrier. Just weeks before I’d received a notice that my malpractice rates could go up by more than 25%. The added news of a pending investigatory audit was chilling. In 25 years of practicing medicine I’d never been audited.
“Is there a complaint, or a law suit against me that I don’t know about?”
“No,” the auditor told me over the phone, “We’ve never seen a medical practice like yours and feel obligated to investigate your process from a medical-legal perspective.”
“Great,” I thought, with a weary sigh. “I’m already battling the insurance model, the status quo of the medical business model, and slow adoption by consumers who are addicted to their $20 co-pay. All I’m trying to do is to breathe life into primary care and get the consumer a much higher quality service for less money than currently subsidized through the insurance model. And now this.”
The time had arrived to add the concerns of the malpractice companies to the list of hurdles to clear if a new vision of a medical care model was ever to catch flight.
I frequently am asked the question “Aren’t you afraid of the malpractice risk?” when I explain my medical practice model, which is based on the doctor answering the phone 24/7, resulting in the patient’s medical problem being solved by the phone more 50% of the time. The simplest counter to this question is to analyze the risk patients incur when the doctor won’t answer the phone. What happens when the doctor is the LAST person to know what’s going on with patients? The answer is obvious. But malpractice companies could have concerns beyond patient safety. Buy-in from the malpractice companies would be critical to the future viability of all telemedicine.
I prepared a summary paper, which included 12 bullet points, explaining how a doctor- patient relationship based on trust , transparency, continuous communications and high quality information systems significantly reduce risk to the person you’re trying to help.
Bullet 1: The industry standard is that 70% of malpractice cases in primary care center on communication barriers. My medical team deploys continuous phone and email communications and 7 days a week- same day office visits when needed between doctor and patient thus significantly reducing these barriers.
.
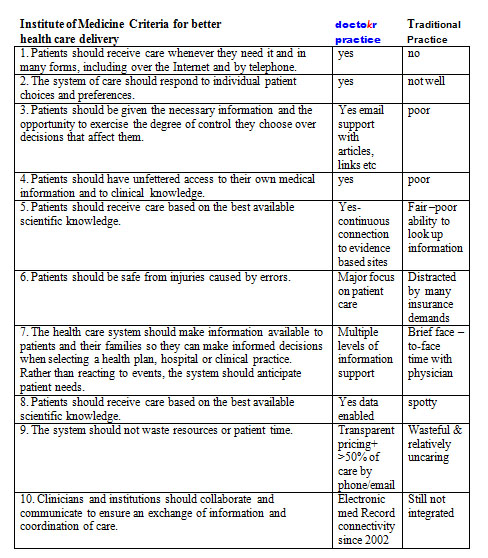
The remaining bullets could be summarized by the conclusions from the Institute of Medicine’s visionary book Crossing the Quality Chasm: A New Health System for the 21st Century using a table developed by The American Medical News when they reviewed the book. I carefully plotted our practice standards compared to the traditional business model as it stands today based on this table:
The auditor showed up, spent 4 hours reviewing our practice, electronic medical records, compliance to HIPPA, our intakes, on-line connectivity, procedures, and practice standards. While the auditor reviewed, I sat as unobtrusively as I could, feeling my brow grow damp with perspiration, as I carefully answered her questions. During the auditor’s time, I never moved to sway her to “my way.” I just let the data that I had accumulated from four years of practice do the talking.
Once the auditor left, I waited for two weeks for the results. By the time their letter arrived, I was scared to open it. The news arriving made me jubilant. The medical practice company announced a DECREASE in my premiums because we used telemedicine and EMR to treat patients so fast (often within 10 minutes of someone calling us we have their issue solved without the patient ever having to come in).
I will admit that I felt, and actually still do feel, vindicated by having my malpractice insurer understand fully the value that the type of telemedicine my practice offers to our patients: round-the-clock access to the doctor, speed of diagnosis, and convenience, which all led to healthier patients and lower risk.
Doctors answering the phone all day for their patients, it’s not just lower risk, it’s better health care at a better price. It’s a win-win-win strategy whose day is arriving.
Until next week, I remain yours in primary care,
Alan Dappen, MD










