February 1st, 2011 by DavedeBronkart in Better Health Network, Opinion
No Comments »

I have a Google alert for “e-patient,” and sometimes I’m surprised what it catches. [Recently] it was this:
3 Reasons Steve Jobs Will Be The Ultimate e-Patient
Steve Jobs’ medical leave sets the stage for the upcoming revolution in the production and delivery of medical information at time of diagnosis. 3 things you need to know.
So I’m thinking: “Oh, wow: Is the term ‘e-patient’ going mainstream?” That would be a hoot, because indeed the Society for Participatory Medicine is engaged in spreading the word.
*This blog post was originally published at e-Patients.net*
January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
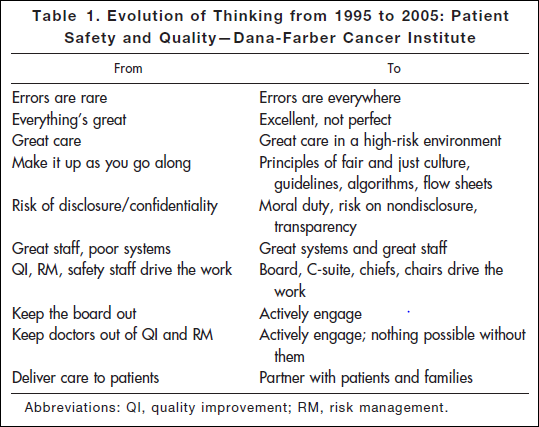
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
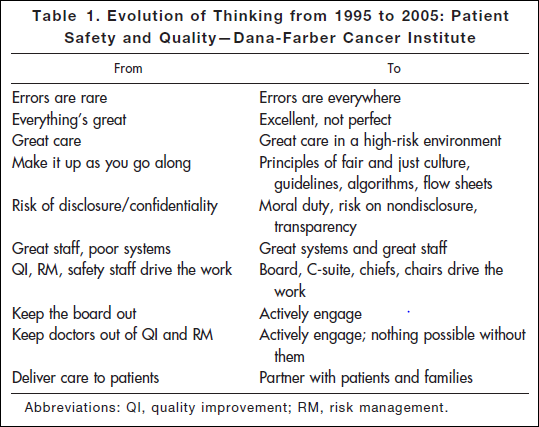
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*
January 16th, 2011 by DavedeBronkart in Health Policy, Opinion
No Comments »

From the Medscape Medical Ethics article entitled “‘Some Worms Are Best Left In The Can’: Should You Hide Medical Errors?“:
Consequences aside, from a strictly ethical perspective, if a patient doesn’t realize that his physician made a mistake, should the physician fess up?
Before you jump to conclusions (as I did), look at the article’s three parts. It’s about a survey. The title is on the inflammatory side; the article is a window into physicians’ views. The introduction continues:
Evidence of the complex prisms through which physicians view these issues was apparent in the replies to four questions asked in Medscape’s exclusive ethics survey. More than 10,000 physicians responded to the survey in 2010.
Subheads:
— Mistakes that don’t harm patients. “Are there times when it’s acceptable to cover up or avoid revealing a mistake if that mistake would not cause harm to the patient?” Sixty percent said “no;” the others split between “yes” and “it depends.”
- I personally can understand this note from a survey respondent: “If there is a mistake that would have no medical effect but would cause extreme, uncalled-for anxiety, then yes,” especially since I know people (some elders, some young) who would indeed freak out, out of proportion. But, that’s a big judgment call.
- I have a harder time accepting this comment: “Why shake the patient’s trust in the doctor for something that is irrelevant?” Irrelevant is a big judgment call, and I’d be really concerned about the natural human tendency to minimize the probable impact of a mistake — especially if a provider thinks it’s all about maintaining a patient’s trust, even when the topic is their own error.
— Mistakes that might harm patients. Ninety five percent said “no;” some still said “yes!” One commented: “If the mistake has not progressed to harmfulness, then it’s essentially a non-issue. Treatment correction takes place and you move on.” Another says if there hasn’t been harm yet, “I think a ‘wait and see’ approach is okay.” Read more »
*This blog post was originally published at e-Patients.net*
January 10th, 2011 by DavedeBronkart in Better Health Network, Health Policy, News
No Comments »

In December, the Society for Participatory Medicine’s executive committee appointed health law attorney David Harlow to represent the Society in public policy matters. Regular readers of HealthBlawg::David Harlow’s Health Care Law Blog know what a patient-centered, participatory thinker David is. This is his first report.
 I am delighted to offer my first report as Public Policy Committee Chair for the Society of Participatory Medicine. I encourage all of you who are not yet Society members to join, and I encourage new and old members to consider volunteering to help with the wide range of public policy issues facing us today.
I am delighted to offer my first report as Public Policy Committee Chair for the Society of Participatory Medicine. I encourage all of you who are not yet Society members to join, and I encourage new and old members to consider volunteering to help with the wide range of public policy issues facing us today.
Over the past couple of months, the Public Policy Committee has gotten its sea legs. We are beginning to add the Society’s voice to the national discourse on patient engagement in a formal manner. As planning for health reform and related initiatives becomes more concrete, it is clear that patient engagement and patient-centeredness are key issues to be considered. For example, it was encouraging to hear Centers for Medicare and Medicaid Services (CMS) Administrator Don Berwick speak about the “Triple Aim” at the Accountable Care Organization (ACO) workshop this fall, and explicitly link the achievement of the triple aim — better care for individuals, better health for populations, and reduced per-capita costs — to patient engagement and empowerment.
There will be many opportunities for the Society to engage with policymakers, payors and provider organizations as this work continues. CMS and its many related organizations, as well as many provider and private sector payor organizations recognize that without maintaining a focus on the patient at the core, health reform and related health IT initiatives cannot be successful. We’ve kicked things off on two fronts — ACOs and Stage 2 Meaningful Use rules. Read more »
*This blog post was originally published at e-Patients.net*
December 31st, 2010 by DavedeBronkart in Better Health Network, Health Tips, Research
2 Comments »

This is the first of the follow-up posts I hope to write from participating in the Salzburg Global Seminar titled “The Greatest Untapped Resource in Healthcare? Informing and Involving Patients in Decisions about Their Medical Care.”
One of our purposes on this site is to help people develop e-patient skills, so they can be more effectively engaged in their care. One aspect is shared decision making, which we wrote about in September. A related topic, from August, is understanding the challenges of pathology and diagnosis. Both posts teach about being better informed partners for our healthcare professionals.
I’ve recently learned of an another topic, which I’m sure many of you know: Practice variation. This is a big subject, and I’ll have several posts about it. It’s complex, the evidence about it is overwhelming, and its cost is truly enormous. Read more »
*This blog post was originally published at e-Patients.net*