January 30th, 2011 by GarySchwitzer in Health Tips, Opinion
Tags: Atlanta Hawks, Gary Schwitzer, Georgia Prostate Cancer Coalition, HealthNewsReview.org, Men's Health, Morehouse School of Medicine, Prizes For Prostates, Prostate Cancer Screening, PSA Screening, Radiotherapy
1 Comment »

We’ve seen it before. A couple of years ago, I wrote about Roswell Park’s Prostate Club for Men offering “Prizes For Prostates” — Buffalo Sabres hockey tickets or Buffalo Bills football tickets among other awards for men who showed proof that they talked to their doctor about prostate cancer.
Now a bunch of Georgia radiotherapy centers and the Morehouse School of Medicine are among those promoting the “Georgia Prostate Cancer Coalition” and luring men in for PSA blood tests by offering them Atlanta Hawks basketball tickets.
They also promote this misleading statistic: “One in 6 men will be diagnosed with prostate cancer in their lifetime.” No explanation is given of what lifetime risk means. And no explanation is given of how many of these “cancers” are indolent and would never have harmed a man. Read more »
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
January 29th, 2011 by KerriSparling in Health Tips, True Stories
Tags: Blood Sugar Control, Diabetes Bingo, Diabetes Burnout, Diabetes Management, Diabetes Tools, Diabetes-Related Health Goals, Glucose Control, Kerri Morrone Sparling, Living With Diabetes, Patient Empowerment, Person With Diabetes, PWD, Six Until Me
No Comments »

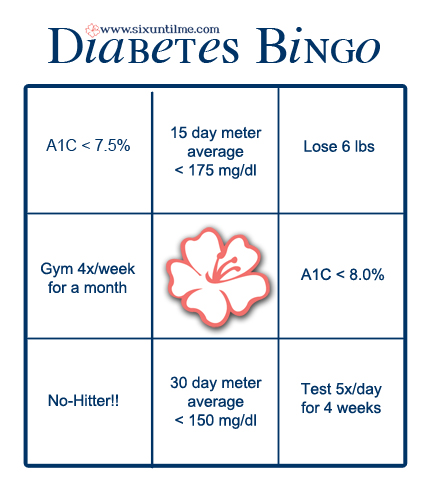
Recently, I reconnected with a long-lost local PWD (person with diabetes) named Ryan. Last time Ryan and I saw one another we were talking about diabetes goal-setting and dealing with wicked bouts of burnout. And this week I received an email from him with a brilliant idea about how to stay motivated towards setting — and reaching — diabetes-related goals.
“I’ve had this ‘pyramid’ for about three months now. Just something that I keep near my desk to keep me focused on my diabetes. After completion of the pyramid, I have no clue what I will do but some kind of celebration will be in order,” he wrote, and attached a slide to his image. And when I opened it, I was like “whoa.”
He had created a pyramid of his diabetes goals. Tangible goals — real-life goals — that are both achievable and ambitious, all at once. I thought this was so clever because it is a constant but non-threatening reminder of what diabetes goals are most top-of-mind for him. (Also, having a celebration at the end of that pyramid completion sounds like a quality idea. Perhaps a Fudgy the Whale?)
I’ve been working towards gaining better control of my diabetes (and overall health) lately, and I love the idea of something I can print out, stick to my fridge, and remain inspired by. I liked the idea of a pyramid, but I kept picturing a huge bingo hall in my mind, with a whole bunch of PWDs sitting at the tables with glucose tabs and bingo markers at the ready. But the trick wasn’t getting four in a row, it was filing the whole card.
I thought about my own personal goals and created this:
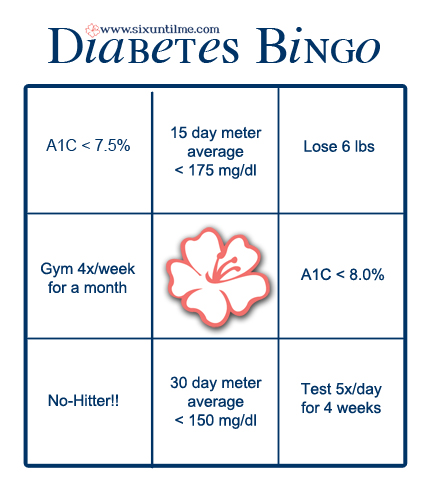
There are a few not-necessarily-diabetes-related goals on there (like “lose 6 pounds,” which is because I’m still trying to de-flump), but there are a lot of diabetes goals that aren’t unique to my particular circumstances. Since I’m trying to emerge from some diabetes burnout, my goals aren’t as tight as they were a few months ago (i.e. the slow progression from an A1C over 8 to one under 7.5). But these are real, and I’m hoping to fill the card within six months. Thanks for the fun idea, Ryan!
What would be on your bingo card?
*This blog post was originally published at Six Until Me.*
January 28th, 2011 by Paul Auerbach, M.D. in Health Tips, Research
Tags: Acetazolamide, Acute Mountain Sickness, AMS, Athlete's Health, Climbing, Decadron, Dexamethasone, Diamox, Dr. Jeremy Windsor, Drug Complications, Drug Safety, Drug Side Effects, Drug-Induced Health Problems, Gastroenterology, healthline, High Altitude, Himalayan Rescue Association, Medicine for the Outdoors, Mountaineering, Mt. Everest, Outdoor Safety, Outdoors and Health, Steroids, Wilderness & Environmental Medicine
No Comments »

 This is a guest post by Dr. Jeremy Windsor.
This is a guest post by Dr. Jeremy Windsor.
**********
Steroids and Acute Mountain Sickness
In recent years, many attempts have been made to identify safe and effective medications to prevent acute mountain sickness (AMS). Acetazolamide (Diamox), currently the “drug of choice” for this purpose, is not perfect and occasionally causes objectionable side effects. Dexamethasone (Decadron), a powerful steroid medication, has become increasingly popular for prevention and treatment in certain circles. While there is ample evidence to suggest that dexamethasone is effective, a recent case report highlights that this drug is not without risk.
In the latest issue of the journal Wilderness & Environmental Medicine [WEM 21(4):345-348, 2010] in an article entitled “Complications of steroid use on Mt. Everest,” Bishnu Subedi and colleagues working for the Himalayan Rescue Association (HRA) described the case of a 27 year-old man who was prescribed a course of three drugs, including dexamethasone, intended to support him during his attempt to climb Mt. Everest. After more than three weeks of taking the medications, the mountaineer noticed the appearance of a rash and decided to stop taking them. Rather than wait for the rash to subside, he chose to continue his acclimatization program and ascend to Camp 3 at 7010m altitude. The patient arrived exhausted and confused; onlookers quickly recognized that something was seriously wrong and so a rescue party was organized to help him back to safety. Read more »
This post, Drug Safety In Preventing Acute Mountain Sickness, was originally published on
Healthine.com by Paul Auerbach, M.D..
January 28th, 2011 by DrCharles in Health Tips, Research
Tags: Anger, Anxiety, Archives of Internal Medicine, Cardiology, Cardiovascular Disease Risk, Cardiovascular Health, CBT, Cognitive Behavioral Therapy, Depression, Emotional Health, Emotional Well-Being, Family Medicine, General Medicine, Heart Attack Deaths, Heart Attack Risk, Heart Disease, Heart Health, High-Stress Life, Hostility, How Stress Affects Health, Live Longer, Longevity, Managing Stress, Mental Health, Primary Care, Psychiatry and Psychology, Psychosocial Stressors, Stress, Stress Control, Stress Reduction, The Examining Room of Dr. Charles
1 Comment »

 “This job is killing me” is not a statement of jest. It is a desperate plea of outright sincerity.
“This job is killing me” is not a statement of jest. It is a desperate plea of outright sincerity.
Stress, anxiety, depression — all have been associated with an increased risk of cardiovascular disease and mortality. But can interventions to help people cope with stress positively affect longevity and decrease risk of dying? The results of a new study in the Archives of Internal Medicine would imply the answer is an encouraging “yes.”
Constructively dealing with stress is easier said than done, but it would seem logical that if we can reduce our psychological and social stressors we might live longer and delay the inevitable wear and tear on our vessels. This study proved that one such intervention, cognitive behavioral therapy (CBT) for patients who suffered a first heart attack, lowered the risk of fatal and nonfatal recurrent cardiovascular disease events by 41 percent over eight years. Nonfatal heart attacks were almost cut in half. Excitement may be dampened by the fact that all-cause mortality did not statistically differ between the intervention and control groups, but did trend towards an improvement in the eight years of follow up.
Definitely less suffering. Maybe less deaths.
The authors state that psychosocial stressors have been shown to account for an astounding 30 percent of the attributable risk of having a heart attack. Chronic stressors include low socioeconomic status, low social support, marital problems, and work distress. Emotional factors also correlated with cardiovascular disease include major depression, hostility, anger, and anxiety. Read more »
*This blog post was originally published at The Examining Room of Dr. Charles*
January 27th, 2011 by AnnMacDonald in Better Health Network, Health Tips
Tags: Ann MacDonald, Body Clock, Bright White Light Therapy, Center for Environmental Therapeutics, Circadian Rhythm, Depression, Emotional Health, Emotional Well-Being, Exposure To Natural Light, FDA, Feeling Mentally Foggy, Food and Drug Administration, Harvard Health Blog, Harvard Health Publications, Harvard Medical School, Harvard Mental Health Letter, Harvard University, Hypothalamus, Light Box, Light Therapy, Mental Fog, Mental Health, SAD, Seasonal Affective Disorder, Sleep-Wake Cycle, Society for Light Treatment and Biological Rhythms, Winter
No Comments »

 This picture shows the view from my office window in Boston: Dull, dreary, and depressing — at least on overcast days like today. Lack of light is one of the reasons that people feel mentally foggy.
This picture shows the view from my office window in Boston: Dull, dreary, and depressing — at least on overcast days like today. Lack of light is one of the reasons that people feel mentally foggy.
One of the bloggers I follow, Rachel Zimmerman of WBUR’s CommonHealth blog, recently wrote that she’s been drinking three times as much coffee as usual. In addition to imbibing more caffeine, I’ve been trying to boost my spirits and alertness with mid-day runs to the snack machine (not the best strategy, in case you’re wondering).
At this time of year, many people aren’t just foggy and sad — they’ve got SAD, or seasonal affective disorder. About half a million Americans — women more often than men — are diagnosed with seasonal affective disorder each year. Many others experience at least some of the symptoms, which include loss of pleasure and energy, inability to concentrate, feelings of worthlessness, and an uncontrollable urge to eat sugar and high-carbohydrate foods (in my case, chocolate chip cookies).
Bright white light therapy remains a mainstay of treatment for seasonal affective disorder. That’s because the light acts on cells in the retina, the tissue located at the back of the eye that sends visual information to the brain. The hypothalamus, which helps control the sleep-wake cycle, is one part of the brain that receives this information. During the winter months, when people tend to stay indoors more, days are shorter, and the weather becomes overcast, our exposure to natural light diminishes. That disrupts the sleep-wake cycle, as well as other circadian rhythms. The result can be symptoms of seasonal affective disorder. Read more »
*This blog post was originally published at Harvard Health Blog*






 This is a guest post by Dr. Jeremy Windsor.
This is a guest post by Dr. Jeremy Windsor.











