April 21st, 2014 by Dr. Val Jones in Opinion, True Stories
2 Comments »
 For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
This week I’ve been considering how in-patient doctoring has changed since I was in medical school. Unfortunately, my experience is that most of the changes have been for the worse. While we may have a larger variety of treatment options and better diagnostic capabilities, it seems that we have pursued them at the expense of the fundamentals of good patient care. What use is a radio-isotope-tagged red blood cell nuclear scan if we forget to stop giving aspirin to someone with a gastrointestinal bleed?
At the risk of infecting my readers with a feeling of helplessness and depressed mood, I’d like to discuss my findings in a series of blog posts. Today’s post is about why electronic medical charts have become ground zero for deteriorating patient care.
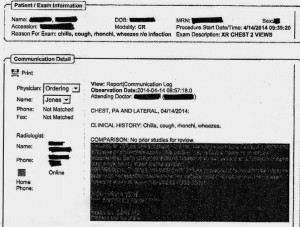
EMR Alert - Featuring radiologist note in illegible font color
1. Medical notes are no longer used for effective communication, but for billing purposes. When I look back at the months of training I received at my alma mater regarding the proper structure of intelligent medical notes, I recall with nostalgia how beautiful they were. Each note was designed to present all the observed and collected data in a cohesive and logical format, justifying the physician’s assessment and treatment plan. Our impressions of the patient’s physical and mental condition, reasons for further testing, and our current thought processes regarding optimal treatments and follow up (including citation of scientific literature to justify the chosen course) were all crisply presented.
Nowadays, medical notes consist of randomly pre-populated check box data lifted from multiple author sources and vomited into a nonsensical monstrosity of a run-on sentence. It’s almost impossible to figure out what the physician makes of the patient or what she is planning to do. Occasional “free text” boxes can provide clues, when the provider has bothered to clarify. One needs to be a medical detective to piece together an assessment and plan these days. It’s both embarrassing and tragic… if you believe that the purpose of medical notes is effective communication. If their purpose is justifying third-party payer requirements, then maybe they are working just fine?
My own notes have been co-opted by the EMRs, so that when I get the chance to free-text some sensible content, it still forces gobbledygook in between. I can see why many of my peers have eventually “given up” on charting properly. No one (except coders and payers interested in denying billing claims) reads the notes anymore. The vicious cycle of unintelligible presentation drives people away from reading notes, and then those who write notes don’t bother to make them intelligent anymore. There is a “learned helplessness” that takes over medical charting. All of this could (I suppose) be forgiven if physicians reverted back to verbal handoffs and updates to other staff/peers caring for patients to solve this grave communication gap. Unfortunately, creating gobbledygook takes so much time that there is less old fashioned verbal communication than ever.
2. No one talks to each other anymore. I’m not sure if this is because of a general cultural shift away from oral communication to text-based, digital intermediaries (think zombie-like teens texting one another incessantly) or if it’s related to sheer time constraints. However, I am continually astonished by the lack of face-to-face or verbal communication going on in hospitals these days. When I first observed this phenomenon, I attributed it to the facility where I was working. However, experience has shown that this is an endemic problem in the entire healthcare system.
When you are overworked, it’s natural to take the path of least resistance – checking boxes and ordering consults in the EMR is easier than picking up a phone and constructing a coherent patient presentation to provide context for the specialist who is about to weigh in on disease management. Nursing orders are easier to enter into a computer system than actually walking over and explaining to him/her what you intend for the patient and why.
But these shortcuts do not save time in the long run. When a consultant is unfamiliar with the partial workup you’ve already completed, he will start from the beginning, with duplicate testing and all its associated expenses, risks, and rabbit trails. When a nurse doesn’t know that you’ve just changed the patient to “NPO” status (or for what reason) she may give him/her scheduled medications before noticing the change. When you haven’t explained to the physical therapists why it could be dangerous to get a patient out of bed due to a suspected DVT, the patient could die of a sudden pulmonary embolism. Depending upon computer screen updates for rapid changes in patient care plans is risky business. EMRs are poor substitutes for face-to-face communication.
In one case I remember a radiology tech expressing amazement that I had bothered to type the reason for the x-ray in the order field. How can a radiologist be expected to rule out something effectively if he isn’t given the faintest hint about what he’s looking for? On another occasion I called to speak with the radiologist on a complicated case where the patient’s medical history provided him with a clue to look for something he hadn’t thought of – and his re-read of the CT scan led to the discovery and treatment of a life-threatening disease. Imagine that? An actual conversation saved a life.
3. It’s easy to be mindless with electronic orders. There’s something about the brain that can easily slip into “idle” mode when presented with pages of check boxes rather than a blank field requiring original input. I cannot count the number of times that I’ve received patients (from outside hospitals) with orders to continue medications that should have been stopped (or forgotten medications that were not on the list to be continued). In one case, for example, a patient with a very recent gastrointestinal bleed had aspirin listed in his current medication list. In another, the discharging physician forgot to list the antibiotic orders, and the patient had a partially-treated, life-threatening infection.
As I was copying the orders on these patients, I almost made the same mistakes. I was clicking through boxes in the pharmacy’s medication reconciliation records and accidentally approved continuation of aspirin (which I fortunately caught in time to cancel). It’s extremely unlikely that I would have hand-written an order for aspirin if I were handling the admission in the “old fashioned” paper-based manner. My brain had slipped into idle… my vigilance was compromised by the process.
In my view, the only communication problem that EMRs have solved is illegible handwriting. But trading poor handwriting for nonsensical digital vomit isn’t much of an advance. As far as streamlining orders and documentation is concerned, yes – ordering medications, tests, and procedures is much faster. But this speed doesn’t improve patient care any more than increasing the driving speed limit from 60 mph to 90 mph would reduce car accidents. Rapid ordering leads to more errors as physicians no longer need to think carefully about everything. EMRs have sped up processes that need to be slow, and slowed down processes that need to be fast. From a clinical utility perspective, they are doing more harm than good.
As far as coding and billing are concerned, I suppose they are revolutionary. If hospital care is about getting paid quickly and efficiently then perhaps we’re making great strides? But if we are expecting EMRs to facilitate care quality and communication, we’re in for a big disappointment. EMRs should have remained a back end billing tool, rather than the hub of all hospital activity. It’s like using Quicken as your life’s default browser. Over-reach of this particular technology is harming our patients, undermining communication, and eroding critical thinking skills. Call me Don Quixote – but I’m going to continue tilting at the hospital EMR* windmill (until they are right-sized) and engage in daily face-to-face meetings with my peers and hospital care team.
*Note: there is at least one excellent, private practice EMR (called MD-HQ). It is for use in the outpatient setting, and is designed for communication (not billing). It is being adopted by direct primary care practices and was created by physicians for supporting actual thinking and relevant information capture. I highly recommend it!
March 31st, 2014 by Dr. Val Jones in Health Policy, Health Tips, Opinion, Research
2 Comments »
 A Canadian study published today in the Annals of Internal Medicine suggests that about one third of new prescriptions (written by primary care physicians) are never filled. Over 15,000 patients were followed from 2006 to 2009. Prescription and patient characteristics were analyzed, though patients were not directly interviewed about their rationale for not filling their prescriptions.
A Canadian study published today in the Annals of Internal Medicine suggests that about one third of new prescriptions (written by primary care physicians) are never filled. Over 15,000 patients were followed from 2006 to 2009. Prescription and patient characteristics were analyzed, though patients were not directly interviewed about their rationale for not filling their prescriptions.
In short, patients were less likely to fill a prescription if the treatment was expensive, but certain types of drug indications had consistently higher non-fill rates:
- Headache (51% not filled)
- Ischemic heart disease (51.3% not filled)
- Thyroid agents (49.4% not filled)
- Depression (36.8% not filled)
Overall, hormonal (especially Synthroid), ENT (especially Flonase), skin, and cardiovascular drugs (especially statins) had the highest non-fill rates.
As far as those prescriptions more likely to be filled, antibiotics (especially for urinary tract infections) ranked number one.
Trends towards prescription compliance were seen among older, healthier patients, and those who were switching medications within a class rather than starting an entirely new drug. Patients who received prescriptions from a doctor that they visited regularly (rather than a new provider) were also more likely to fill their prescriptions.
This study was not designed to elucidate the exact rationale behind prescription non-adherence, but I am willing to speculate about it. In my experience, patients are less likely to fill a prescription if a reasonable over-the-counter alternative is available (think headache or allergy relief). I also suspect that they are less likely to fill a prescription if they believe it won’t help them (skin cream) or isn’t treating a palpable symptom (statin therapy for dyslipidemia). Finally, patients are probably nervous about starting a medicine that could effect their metabolism or cognition (thyroid medication or anti-depressant) without a full explanation of the possible benefits and side effects.
I was surprised to see how compliant patients seem to be with antibiotic agents (at least, filling the initial prescriptions). Given the increasing rates of antibiotic resistance, this reinforces the need to limit prescriptions to those agents truly indicated, and to analyze bacterial sensitivities during the treatment process to optimize medical management.
My take home message from this study is that providers need to do a better job of explaining the reasoning behind new prescriptions (their necessity, consequences of non-compliance, and risk/benefit profiles) and reviewing the overall cost to the patient. If a cheaper, effective alternative is available (whether OTC or generic), we should consider prescribing it. Providers can likely improve medication compliance rates with a little patient education and price consciousness. Extra time should be spent with patients at higher risk for non-compliance due to their personal situation (age, degree of illness, income level) or if a specific drug with lower compliance rates is being introduced (Synthroid, statins, etc.) Regular follow up (especially with the same prescriber) to ensure that prescriptions are filled and taken as directed is also important.
March 24th, 2014 by Dr. Val Jones in Health Policy, Health Tips, Opinion
3 Comments »
 One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a locum tenens physician, traveling across the country to “cover” for my peers on vacation or when hospitals are having a hard time recruiting a full-time MD. This type of work is particularly vulnerable to gaps in continuity of care, and has heightened my awareness of the prevalence of poor sign-outs.
One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a locum tenens physician, traveling across the country to “cover” for my peers on vacation or when hospitals are having a hard time recruiting a full-time MD. This type of work is particularly vulnerable to gaps in continuity of care, and has heightened my awareness of the prevalence of poor sign-outs.
Recent research suggests that communications lapses are the number one cause of medical errors and adverse events in the healthcare system. An analysis published in the Archives of Internal Medicine suggests various kinds of consequences stemming from inadequate transfer of information, including missed diagnoses, incomplete work ups, ICU admissions, and near-miss errors. I have personally witnessed all manner of problems, including medication errors (the patient’s full list of medical conditions was not known by the new physician), lack of follow up for incidental (though life-threatening) findings discovered during a hospital stay, progression of infection due to treatment delay, inappropriate antibiotic therapy (follow up review of bacterial drug resistance results did not occur), accidental repeat fluid boluses in patients who no longer required rehydration (and had kidney or heart failure), etc.
It has long been suspected, though not unequivocally proven, that sleep deprivation (due to extended work hours and long shifts) is a common cause of medical errors. New regulations limiting resident physician work hours to 80 hours a week have substantially improved the quality of life for MDs in training, but have not made a remarkable difference in medical error rates. In my opinion, this is because sleep deprivation is a smaller contributor to the error problem than incomplete information transfer. If we want to keep our patients safe, we need to do a better job of transferring clinical information to peers assuming responsibility for patient care. This requires more than checklists (made popular by Atul Gawande et al.), it’s about creating a culture of carefulness.
Over the past few decades, continuity of care has been undermined by a new “shift worker” or “team” approach. Very few primary care physicians admit patients to local hospitals and continue to manage their care as inpatients. Instead, hospitalists are responsible for the medical management of the patient – often sharing responsibility as a group. This results in reduced personal knowledge of the patient, leading to accidental oversights and errors. The modern shift-worker model is unlikely to change, and with the rise of locum tenens physicians added to the mix – it’s as if hospitalized patients are chronically cared for by “float staff,” seeing the patient for the very first time each day.
As a physician frustrated with the dangers of chronically poor sign-outs, these are the steps that I take to reduce the risk of harm to my patients:
1. Attend nursing change of shift as much as possible. Some of the most accurate and best clinical information about patients may be obtained from those closest to them. Nurses spend more face-to-face time with patients than any other staff members and their reports to one another can help to nip problems in the bud. I often hear things like, “I noticed that Mr. Smith’s urine was cloudy and smelled bad this morning.” Or “Mrs. Jones complained of some chest pain overnight but it seems to be better now after the Percocet.” These bits of information might not be relayed to the physician until they escalate into fevers, myocardial infarctions, or worse. In an effort to not “bother the physician with too much detail” nurses often unwittingly neglect to share subtle findings that can prevent disease progression. If you are new to a unit or don’t already know the nursing staff well, join their morning or evening sign out meeting(s). They (and you) will be glad you did.
2. Pretend that every new patient needs an H&P (complete history and physical exam). When I pick up a new patient, I comb through their medical chart very thoroughly and carefully. I only need to do this once, and although it takes time, it saves a lot of hassle in the long run. I make note of every problem they’ve had (over the years and currently) and list them in a systems-based review that I refer to in every note I write thereafter.
3. Apply the “trust but verify” principle. I read other physicians’ notes with a careful eye. Electronic medical records systems are notorious for “copy and paste” errors and accidentally carrying over “old news” as if it were an active problem. If a physician notes that the patient has a test or study pending, I’ll search for its result. If they are being treated empirically for some kind of infection, I will look for microbiologic evidence that the bug is sensitive to the antibiotics they are receiving. I’ll ask the patient if they’ve had their radiology study yet, and then search for the result. I’ll review the active medication list and see if one of my peers discontinued or started a new medicine without letting me know. I never assume that anything in the medical record is correct. I try my best to double check the notes and data.
4. Create a systems-based plan of care, reconcile it each day with the active medication list. I like to organize patient diseases and conditions by body systems (e.g. cardiovascular, endocrine, gastrointestinal, neurologic, dermatologic, etc.) and list all the diseases/conditions and medications currently being offered to treat them. This only has to be done thoroughly one time, and then updated and edited with additional progress notes. This helps all consultants and specialists focus in on their particular area of interest and know immediately what is currently being done for the patient (both in their system of interest and as a whole) with a glance at your note. Since medications often have multiple purposes, it is also very helpful to see the condition being treated by each medication. For example, if the patient is on coumadin, is it because they have a history of atrial fibrillation, a prosthetic heart valve, a recent orthopedic procedure, or something else? That can easily be gleaned from a note with a systems-based plan of care.
5. Confirm your assessment and plan with your patient. I often review my patients’ medication and problem list with them (at least once) to ensure that they are aware of all of their diagnoses, and to make sure I haven’t missed anything. Sometimes a patient will have a condition (otherwise unmentioned in their record) that they treat with certain medications at home that they are not getting in the hospital. Errors of omission are not uncommon.
6. Sign out face-to-face or via phone whenever possible. These days people seem to be less and less eager to engage with each other face-to-face. Texting, emailing, and written sign-outs often substitute for face-to-face encounters. I try to remain “old school” about sign-outs because inevitably, something important comes up during the conversation that isn’t noted in the paper record. Things like, “Oh, and Mr. Smith tried to hit the nursing staff last night but he seems calmer now.” That’s something I want to know about so I can preempt new episodes, right nursing staff?
7. Create a culture of carefulness. As uncomfortable as it is to confront peers who may not be as enthusiastic about detailed sign-outs as I am, I still take the initiative to get information from them when I come on service and make sure that I call them to provide them with a verbal sign-out when I’m leaving my patients in their hands. By modeling good sign offs, and demonstrating their utility by heading off problems at the pass, I find that other doctors generally appreciate the head’s up, and slowly adopt some of my strategies (at least when working with me). I have found that nurses are particularly good at learning to tell me everything (no matter how small it may seem at the time) and have heard time and again that things “just run so much more smoothly” when we communicate and even “over-communicate” when in doubt.
“The Devil is in the details.” This is more true at your local hospital than almost anywhere else. Reducing hospital error rates is possible with some good, old-fashioned verbal handoffs and a small dose of charting OCD. Let’s create a culture of carefulness, physicians, so we don’t get crushed with more top-down bureaucratic rules to solve this problem. We can fix this ourselves, I promise.
March 18th, 2014 by Dr. Val Jones in Announcements, Health Tips
No Comments »
 I’m excited to announce that US News and World Report has invited me and some other social-media savvy physicians to participate in a live Twitter chat about how to find a good doctor. The chat will be held on Thursday, March 20th at 2pm EST. You can join the conversation by following the #DoctorFinder hashtag or take the pre-chat poll here.
I’m excited to announce that US News and World Report has invited me and some other social-media savvy physicians to participate in a live Twitter chat about how to find a good doctor. The chat will be held on Thursday, March 20th at 2pm EST. You can join the conversation by following the #DoctorFinder hashtag or take the pre-chat poll here.
Most people, including physicians, rely on personal references to find a good doctor. But what do you do when you’re far from home, or you don’t know anyone with firsthand knowledge of local doctors? My parents recently asked me to recommend a physician for them in a state where I knew none of my colleagues personally. This is the 10-step process that I used to help them navigate their way to an excellent specialist – I hope it helps others you find the right doctor as well!
1. Determine what kind of doctor you need. You’d be surprised how many different specialists treat the same symptom – depending on its underlying cause. Take “back pain” for example – should you see a primary care physician, an orthopedist, a neurosurgeon, an anesthesiologist, a rheumatologist, or a rehab specialist to evaluate your symptoms? That depends on the cause of the pain, which might not yet be evident to you. The first step to finding a good physician is to figure out which type is best suited to your potential diagnosis. Bouncing from specialist to specialist can be costly, so if you’re not sure which kind of physician specializes in treating your disease or condition (or if you haven’t been diagnosed yet), start with a primary care physician first.
If you’d like to ask an online physician about your symptoms (or find out which specialist would be the most appropriate for you or your loved one), eDocAmerica.com is my favorite online physician consultant service (note that I answer questions for them.)
2. Compile a list of all the doctors (of the specialty you need) in your area. This list can be generated by your insurance carrier or by an online search of doctor-finder databases such as Healthgrades.com, Vitals.com, or US News & World Report’s Doctor Finder directory.
3. Narrow online choices by your preferences (available via Healthgrades.com or Vitals.com databases.) Check out the doctors’:
Hospital affiliation(s)
Office location(s)
Educational background
Specialty interests
Languages spoken
Years in practice
Gender
Types of insurance accepted
Review CV if available (often on affiliated hospital website)
Check out patient reviews (take them with a grain of salt in case they are skewed by an unfairly disgruntled patient)
Make sure they’re accepting new patients
4. Do an online “background check” of your top choices.
5. Make an appointment – consider the following qualities in a good physician experience:
- The team: courteousness of scheduling staff, professionalism of nurses, PA’s, techs, etc.
- Facilities – cleanliness, comfort
- Medical records/communication – how will they provide you your data? EMR? Email?
- Timeliness/convenience
6. Come prepared
- Bring your list of medications
- Bring a list of your medical and surgical history/conditions
- Bring a list of your allergies
- Bring contact information for your other physicians/providers
- Bring your insurance information
7. Ask the right questions
- How many procedures (like the one I’ll need) have you performed previously?
- What are the risks/benefits of the procedure? Alternatives?
- What should I read to learn more about this?
- If unsure of diagnosis: What else could this be?
- Are there other medicines that are less expensive that we could substitute?
8. Go with your gut
- Did the doctor explain everything clearly?
- Did the doctor seem to care about you?
- Do you trust your doctor to be thorough with follow up?
- Do you like your doctor?
9. Get a second opinion
- If the doctor did not meet your expectations in any significant way, find another one
- If you want to be sure that you’re on the best path, get a second opinion from one of his/her peers or do it online: eDocAmerica (for generalist questions), Best Doctors (to be matched with top national specialists)
10. Reward good doctors with good online recommendations so others can benefit. Physician ratings are only as reliable as the reviewers. Help other patients locate good doctors by promoting those who deserve it.
February 13th, 2014 by Dr. Val Jones in Health Tips
3 Comments »
 Thanks to support from OTCSafety.org, I’ve created a series of health tips for common medical concerns. This week’s article is about how to diagnose and treat sleep difficulties in children and adolescents. There are many possible causes of insomnia, which include everything from emotional distress to bad dreams, breathing problems, stomach pains, medical conditions or behavioral problems.
Thanks to support from OTCSafety.org, I’ve created a series of health tips for common medical concerns. This week’s article is about how to diagnose and treat sleep difficulties in children and adolescents. There are many possible causes of insomnia, which include everything from emotional distress to bad dreams, breathing problems, stomach pains, medical conditions or behavioral problems.
In my article I discuss how you can work with a healthcare professional to determine the cause of your child’s sleep difficulties (this includes details on how to keep a sleep diary). I offer instructive do’s and don’ts to promote healthy sleep, and offer examples of symptoms that may require medical intervention.
For the full article, please click here. I promise it won’t put you to sleep! 😉
 For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.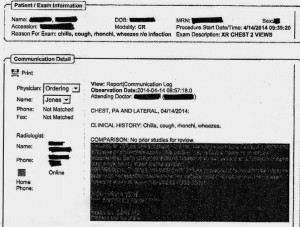



 One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a
One of my biggest pet peeves is taking over the care of a floor-full of complicated patients without any explanation of their current conditions or plan of care from the physician who most recently treated them. Absent or inadequate verbal and written “handoffs” of patient care are alarmingly common in my experience. I work primarily as a 









