September 7th, 2012 by Dr. Val Jones in Health Tips, Opinion
No Comments »
 I recently found my way to an interesting NPR podcast via a link from Dr. Ranit Mishori (@ranitmd) on Twitter. The host of the show interviewed a physician (Dr. Mishori), an obesity researcher (Sara Bleich), and a family nurse practitioner (Eileen O’Grady) about how healthcare providers are trying (or not trying) to help patients manage their weight. Several patients and practitioners called in to participate.
I recently found my way to an interesting NPR podcast via a link from Dr. Ranit Mishori (@ranitmd) on Twitter. The host of the show interviewed a physician (Dr. Mishori), an obesity researcher (Sara Bleich), and a family nurse practitioner (Eileen O’Grady) about how healthcare providers are trying (or not trying) to help patients manage their weight. Several patients and practitioners called in to participate.
First of all, I found it intriguing that research has shown that the BMI of the treating physician has a significant impact on whether he or she is willing to counsel a patient about weight loss. Normal weight physicians (those with a BMI under 25) were more likely to bring up the subject (and follow through with weight loss and exercise planning with their patients) than were physicians who were overweight or obese. Sara Bleich believes that this is because overweight and obese physicians either don’t recognize the problem in others who have similar body types, or that their personal shame about their weight makes them feel that they don’t have the right to give advice since they don’t practice what they preach. While 60% of Americans are either overweight or obese, 50% of physicians are also in those categories.
Although it’s not entirely surprising that overweight/obese physicians feel as they do, it made me wonder what other personal conditions could be influencing evidence-based patient care. Is a physician with high blood pressure less apt to encourage salt restriction or medication adherence? What about depression, smoking cessation, or erectile dysfunction? Are there certain personal diseases or conditions that impair proper care and treatment in others?
Several callers recounted negative experiences with physicians where they were “read the Riot Act” about their weight. One overweight woman said she handled this by simply avoiding going to the doctor at all, and another obese man said his doctor made him cry. However, the man went on to lose 175 pounds through diet and exercise modifications and said that the “tough love” was just what he needed to galvanize him into action.
Dr. Mishori felt that the “Riot Act” approach was rarely helpful and usually alienated patients. She advocated a more nuanced and sensitive approach that takes into account a patient’s social and financial situation. She explained that there’s no use advocating personal training sessions to a person on food stamps. Physicians need to be more sensitive to patients’ living conditions and physical abilities.
In the end, I felt that nurse practitioner Eileen O’Grady contributed some helpful observations – she argued that the rate-limiting factor in reversing obesity is not information, but motivation. Most patients know what they “should do” but just don’t have the motivation to start, and keep at it till they achieve a healthy weight. Ms. O’Grady devoted her practice to weight loss coaching by phone, and she believes that telephones have one big advantage over in-person visits: patients are more likely to be honest when there is no direct eye contact with their provider. Her secret to success, beyond a non-judgmental therapeutic environment, is setting small, attainable goals. She says that if she doesn’t believe the patient has at least a 70% chance of success, they should not set that particular goal.
Starting goals may be as simple as “finding a workout outfit that fits.” As the patient grows in confidence with their successes, larger, broader goals may be set. Weight loss coaching and intensive group therapy may be the most motivating strategy that we have to help Americans shed unwanted pounds. Apparently, the USPS Task Force agrees, as they recommend “intensive, multicomponent behavioral interventions” for those who screen positive for obesity in their doctors’ offices.
I think it’s unfortunate that most doctors feel that they “simply don’t have time to counsel patients about obesity.” Diet and exercise are the two most powerful medical tools we have to combat many chronic diseases. What else is so important that it’s taking away our time focusing on the “elephant in the room?” Pills are not the way forward in obesity treatment – and we should have the courage to admit it and do better with confronting this problem head-on in our offices, and also in our own lives.
September 5th, 2012 by Dr. Val Jones in Book Reviews
2 Comments »
 I just finished reading True Medical Detective Stories, Dr. Clifton Meador’s personal collection of medical mysteries. Dr. Meador is a prolific writer and the former dean of the University of Alabama School of Medicine and professor at Vanderbilt School of Medicine. His 50+ years in the academic arena have exposed him to some delightfully rare and bizarre medical cases, and he shares his top 18 in this pithy little book.
I just finished reading True Medical Detective Stories, Dr. Clifton Meador’s personal collection of medical mysteries. Dr. Meador is a prolific writer and the former dean of the University of Alabama School of Medicine and professor at Vanderbilt School of Medicine. His 50+ years in the academic arena have exposed him to some delightfully rare and bizarre medical cases, and he shares his top 18 in this pithy little book.
Dr. Meador was inspired by Berton Roueché, a staff writer at The New Yorker, who helped to popularize the medical detective story genre in the 1940’s and beyond. Each vignette is between 3-5 pages in length, making for a very quick and entertaining read. In choosing to review this book I was very tempted to give away details of some of the cases in order to entice you to read it, but I have resisted the urge so as not to spoil the fun.
Broadly speaking, the stories include a rare case of intractable hiccups, a bizarre infection caused by sexually deviant behavior, and several examples of the power of the mind to inflict bodily harm on oneself and others. In each situation, the underlying cause of the symptoms or disease is uncovered through careful listening and analysis. Often, human shame and fear must be managed before the truth can bubble to the surface.
I highly recommend this book to healthcare professionals, skeptics, and anyone interested in a fascinating look at some of the most unusual medical cases described in one book. Perhaps we can all learn to become better listeners, or true “medical detectives,” from Dr. Meador’s stories. You can find his book here at Amazon.com. Enjoy!
September 3rd, 2012 by Dr. Val Jones in Health Tips, True Stories
No Comments »
 I’ve spent the last couple of weeks making house calls to “at risk” seniors in rural South Carolina. At the rate of about 7 house calls per day, I was able to make some observations based on a respectable sample size. I was both surprised and intrigued by the living conditions I encountered, and I’m pleased to report that I have now performed my first physical exam under the careful scrutiny of a cat, rooster, and hen team (photo at left). On another house call I was offered a pygmy goat as a thank-you for my efforts, and countless good-natured folk offered me home made iced-tea and such edible delectables as fish patties and peach honey.
I’ve spent the last couple of weeks making house calls to “at risk” seniors in rural South Carolina. At the rate of about 7 house calls per day, I was able to make some observations based on a respectable sample size. I was both surprised and intrigued by the living conditions I encountered, and I’m pleased to report that I have now performed my first physical exam under the careful scrutiny of a cat, rooster, and hen team (photo at left). On another house call I was offered a pygmy goat as a thank-you for my efforts, and countless good-natured folk offered me home made iced-tea and such edible delectables as fish patties and peach honey.
But what struck me the most was that certain seniors were in far better health than others their age, and that the healthier ones all had one thing in common: strict daily exercise regimens. I realize that this is not ground-breaking news (that exercise is good for us), but the stark contrast between those who exercised and those who didn’t could not have been clearer to me.
One particularly charming 85 year old man gave me a tour of his vegetable garden, and explained that he bicycled into town six days a week to give away okra (and other veggies) to church friends and town folk. Growing vegetables and giving them away was his current life’s work, and although he lived in extremely modest circumstances, what he owned was tidy and clean. He was joyful, bright, and had the physique of an athlete.
Contrast this man to another patient in his 80’s who didn’t exercise at all, and stayed inside smoking cigarettes most of the day. He was blind in one eye, nearly deaf, struggled to breathe, had sores on his skin. He was depressed, over-weight, and swollen from heart failure. I was so sad to see his condition, and the relative squalor in which he lived. Urine and smoke odor permeated the house, and I wondered how much longer he would survive.
When I arrived at another octogenarian’s home, I noted that the garage was filled with watermelons of various sizes. Upon further inquiry, the gentleman said that he had hand-picked the watermelons from a plot of land that he owns 2 miles from his house. He brought them back to the house with a wheel barrow… and had made many trips back and forth over the past week. He was taking no medications and had a completely normal physical exam.
And so my days went – back-to-back visits with seniors who either were engaged in an active lifestyle, or who were wasting away, cooped up indoors with advancing dementia and chronic disease. I realized that no medical treatment has the power to overcome the relentless damage that inactivity, smoking, and deconditioning cause. The secret to a healthy old age lies in lifestyle choices, not pill bottles.
As we enjoy the last holiday weekend of the summer, let’s consider how important labor actually is to our mental and physical well being. You’re never too old to haul watermelons down the road, grow okra for your neighbors, or simply commit to smoking cessation and daily walks. If you do this regularly, your health will surely improve – and your quality of life will be enhanced immeasurably. In the end, adding life to years is what medicine is all about.
August 20th, 2012 by Dr. Val Jones in Health Policy, Opinion
No Comments »
 Health Leaders Media recently published an article about “the latest idea in healthcare: the informed shared medical decision.” While this “latest idea” is actually as old as the Hippocratic Oath, the notion that we need to create an extra layer of bureaucracy to enforce it is even more ridiculous. The author argues that physicians and surgeons are recommending too many procedures for their patients, without offering them full disclosure about their non-procedural options. This trend can be easily solved, she says, by blocking patient access to surgical consultants:
Health Leaders Media recently published an article about “the latest idea in healthcare: the informed shared medical decision.” While this “latest idea” is actually as old as the Hippocratic Oath, the notion that we need to create an extra layer of bureaucracy to enforce it is even more ridiculous. The author argues that physicians and surgeons are recommending too many procedures for their patients, without offering them full disclosure about their non-procedural options. This trend can be easily solved, she says, by blocking patient access to surgical consultants:
“The surgeon isn’t part of the process. Instead, patients would learn from experts—perhaps hired by the health system or the payers—whether they meet indications for the procedure or whether there are feasible alternatives.”
So surgeons familiar with the nuances of an individual’s case, and who perform the procedure themselves, are not to be consulted during the risk/benefit analysis phase of a “shared” decision. Instead, the “real experts” – people hired by insurance companies or the government – should provide information to the patient.
I understand that surgeons and interventionalists have potential financial incentives to perform procedures, but in my experience the fear of complications, poor outcomes, or patient harm is enough to prevent most doctors from performing unnecessary invasive therapies. Not to mention that many of us actually want to do the right thing, and have more than enough patients who clearly qualify for procedures than to try to pressure those who don’t need them into having them done.
And if you think that “experts hired by a health insurance company or government agency” will be more objective in their recommendations, then you’re seriously out of touch. Incentives to block and deny treatments for enhanced profit margins – or to curtail government spending – are stronger than a surgeons’ need to line her pockets. When you take the human element out of shared decision-making, then you lose accountability – people become numbers, and procedures are a cost center. Patients should have the right to look their provider in the eye and receive an explanation as to what their options are, and the risks and benefits of each choice.
I believe in a ground up, not a top down, approach to reducing unnecessary testing and treatment. Physicians and their professional organizations should be actively involved in promoting evidence-based practices that benefit patients and engage them in informed decision making. Such organizations already exist, and I’d like to see their role expand.
The last thing we need is another bureaucratic layer inserted in the physician-patient relationship. Let’s hold each other accountable for doing the right thing, and let the insurance company and government “experts” take on more meaningful jobs in clinical care giving.
August 15th, 2012 by Dr. Val Jones in Health Policy, Opinion
1 Comment »
 Hospitals can be dangerous and inefficient; therefore it is easy to connect with Atul Gawande’s recent New Yorker essay “BigMed” suggesting that the streamlined, production processes found at the Cheesecake Factory can and likely will be applied to healthcare. Yet hospital care should not be confused with the full spectrum of healthcare. One must make the distinction between the cognitive process of medical diagnosis occurring in exam rooms, with the procedural basis of surgical care and hospital recovery. While Dr. Gawande has provided a wonderful revealing portrait of cost-effective, fast, food preparation and delivery at the Cheesecake Factory, he has focused on the process of creating the meal, not the process of deciding what meal to make. Successful surgery, for the wrong diagnosis, is a problem. If we are to solve some of healthcare’s largest failings we should focus on what happens as physicians try to address their patient’s problems, diagnose and make decisions, at the table of medicine called the exam room.
Hospitals can be dangerous and inefficient; therefore it is easy to connect with Atul Gawande’s recent New Yorker essay “BigMed” suggesting that the streamlined, production processes found at the Cheesecake Factory can and likely will be applied to healthcare. Yet hospital care should not be confused with the full spectrum of healthcare. One must make the distinction between the cognitive process of medical diagnosis occurring in exam rooms, with the procedural basis of surgical care and hospital recovery. While Dr. Gawande has provided a wonderful revealing portrait of cost-effective, fast, food preparation and delivery at the Cheesecake Factory, he has focused on the process of creating the meal, not the process of deciding what meal to make. Successful surgery, for the wrong diagnosis, is a problem. If we are to solve some of healthcare’s largest failings we should focus on what happens as physicians try to address their patient’s problems, diagnose and make decisions, at the table of medicine called the exam room.
Consider the continuum of the patient encounter, from first symptoms, through diagnosis and therapy at a restaurant called Med. At Med I spend all of my shifts with my patrons at my tables. This is an unusual restaurant since the patrons are never sure of what they want to eat and appear every 20 minutes with ever changing lists of unique groups of ingredients to share with me. There are varying ingredients and thousands of meals that can be created. The patrons know the ingredients, but not the meal that they would like to eat. From memory I respond to the customers list of ingredients and ask many questions, take the pulse and other vital signs of the customer, order blood samples, radiographic studies and then decide for the patron which meal their ingredients add up to. All from memory. At Med, restaurant patrons also ask for foods and “food tests” they have seen on television all purported to be risk free. Further complicating the process is my customer is not out for a fun and relaxing evening, they are in small booths in skimpy, open at the back gowns, often anxious and uncertain if they will be harmed or poisoned by my foods, or simply receive a meal they do not want. Some are in pain and some are depressed, while other customers are totally unrealistic about the meal that is to be delivered. You see at Restaurant Med, where patrons only can speak to their wait staff about ingredients, and demand the modern but unhelpful ovens they heard about from friends and the media, it is really difficult to create meals that patrons thoroughly enjoy.
An appendectomy should be consistently performed and priced, but how do we consistently perform and price considering the ambiguity inherent in diagnosis itself? Unlike a restaurant, where customers choose a meal by ordering a meal, at restaurant Med some higher force gives an unfortunate person an undifferentiated and undiagnosed problem that needs and deserves an answer. As it turns out, none of the patrons really want to be eating at restaurant Med, as they always receive a meal they did not ask for.
Patients do not choose their diagnoses from menus; doctors must discover and diagnose them.
If your waiter tries to memorize all the orders at all the tables, you might get the wrong meal, and if your server is in a hurry, thai dipping sauce might be spilled on your new silk blouse. Likewise if physicians are in a rush, they might not take a thorough history, perform a complete physical exam, or have an accurate and thorough list of diagnostic possibilities, ultimately resulting in the wrong diagnosis. If your physician believes he or she can memorize all the questions, tied to all the possible diagnoses you also might receive the wrong diagnosis. With that wrong diagnosis you might end up in a hospital more efficient than the Cheesecake Factory with doctors efficiently ordering unnecessary tests, and performing wrong surgeries for the wrong diagnosis all with the ease and speed of the best assembly line on the planet.
Diagnostic and patient management error caused by cognitive mistakes in the exam room are all too often overlooked and unmentioned in the discussion of repairing our broken healthcare system. There are over a billion outpatient visits in the US each year, and numerous studies have shown 15-20% of these visits have an inaccurate diagnosis. Autopsy data proves this, malpractice insurers know this, and policy makers avoid it. Add diagnostic error in the emergency room and walk-in clinics to error in the out-patient offices of medicine and you have more than 200 million errors. If we are to resolve some of healthcare’s deepest woes we need to address diagnostic errors and the decision-making occurring at the restaurant table of medicine, the exam room. A bright light needs to be shined on the simple fact that there is too much to know, to ask and to apply during a 15 minute encounter unless the patient has the simplest of medical questions or problems. Medical informaticists, researchers and innovative companies are focusing on this essential limitation of medical decision-making by designing information systems to be used by physicians at the point of care, during the patient encounter. Problem oriented systems can also be designed for use by patients in advance of the visit, and the future holds home-based information coordinated with professional clinical decision support. These new information tools are beginning to take the guessing out of which ingredients (symptoms) relate to the meals that the patient ultimately receives (diagnosis and treatment). If medical care is truly to be driven back to primary care we need to arm the waiters of medicine with purposefully designed tools and training to resolve ambiguity, aid diagnosis and inform therapy in the exam room.
Art Papier MD
Art Papier MD is CEO of Logical Images the developer of www.visualdx.com a clinical decision support system, Associate Professor of Dermatology and Medical Informatics at the University of Rochester College of Medicine, and a Director of the Society To Improve Diagnosis In Medicine (SIDM) http://www.improvediagnosis.org/
 I recently found my way to an interesting NPR podcast via a link from Dr. Ranit Mishori (@ranitmd) on Twitter. The host of the show interviewed a physician (Dr. Mishori), an obesity researcher (Sara Bleich), and a family nurse practitioner (Eileen O’Grady) about how healthcare providers are trying (or not trying) to help patients manage their weight. Several patients and practitioners called in to participate.
I recently found my way to an interesting NPR podcast via a link from Dr. Ranit Mishori (@ranitmd) on Twitter. The host of the show interviewed a physician (Dr. Mishori), an obesity researcher (Sara Bleich), and a family nurse practitioner (Eileen O’Grady) about how healthcare providers are trying (or not trying) to help patients manage their weight. Several patients and practitioners called in to participate.

 I just finished reading
I just finished reading  I’ve spent the last couple of weeks making house calls to “at risk” seniors in rural South Carolina. At the rate of about 7 house calls per day, I was able to make some observations based on a respectable sample size. I was both surprised and intrigued by the living conditions I encountered, and I’m pleased to report that I have now performed my first physical exam under the careful scrutiny of a cat, rooster, and hen team (photo at left). On another house call I was offered a pygmy goat as a thank-you for my efforts, and countless good-natured folk offered me home made iced-tea and such edible delectables as fish patties and peach honey.
I’ve spent the last couple of weeks making house calls to “at risk” seniors in rural South Carolina. At the rate of about 7 house calls per day, I was able to make some observations based on a respectable sample size. I was both surprised and intrigued by the living conditions I encountered, and I’m pleased to report that I have now performed my first physical exam under the careful scrutiny of a cat, rooster, and hen team (photo at left). On another house call I was offered a pygmy goat as a thank-you for my efforts, and countless good-natured folk offered me home made iced-tea and such edible delectables as fish patties and peach honey.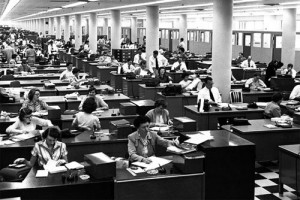 Health Leaders Media recently
Health Leaders Media recently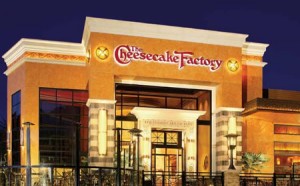 Hospitals can be dangerous and inefficient; therefore it is easy to connect with Atul Gawande’s recent New Yorker essay “
Hospitals can be dangerous and inefficient; therefore it is easy to connect with Atul Gawande’s recent New Yorker essay “







