June 8th, 2009 by Dr. Val Jones in Health Policy, Opinion
9 Comments »
The abortion “issue” is such a hot topic that I have never written about it on this blog until today. I hope I won’t regret that decision but I felt it was appropriate to respond to this medical student’s essay – and the ~560+ comments that follow it – as a physician who has witnessed (but never performed) about 100 abortions. Let me explain.
During my Emergency Medicine training I was required to perform a certain number of intubations and abdominal ultrasound scans. My residency training program offered rotations in Ob/Gyn and at a local Planned Parenthood center. The senior residents told me that the best way to fulfill my intubation requirements was to assist with the Ob/Gyn OR procedures because the patients were young, healthy, and generally uncomplicated. At the time I was really excited by the opportunity to get the experience I needed – in as short a time as possible. I used to hang out in an Ob/Gyn operating room asking if I could assist the anesthesiologist with the intubations. Once they got to know and trust me, I could intubate about 6 patients in a day – an opportunity otherwise hard to come by as all the new anesthesiology residents were vying to practice intubation themselves.
One of the Ob/Gyns who used the OR (where I got my intubation experience) scheduled some abortions of fetuses that were at the border of viable – as old as 23 weeks. That made me quite uncomfortable, and I know that there were other staff (and several nurses) who refused to work with that physician. However, as squirmy as I felt, I thought it was important for me to see first hand what the procedure entailed… because otherwise I’d have to rely on anecdotes and second-hand opinions to draw my own conclusions. I wanted to see this for myself.
I’ll never forget the day I witnessed the first late-ish term abortion. I was preparing my intubation equipment – fidgeting with the Mac size 4 blade, making sure the light worked, when the physician brought the patient into the room on a gurney. The woman’s abdomen was very pregnant, and the Ob/Gyn was stroking her hair and whispering reassuring things to her. The anesthesiologist made small talk with the patient, explaining the nuts and bolts of the anesthesia – the oxygen mask – the propofol – the intubation. I stayed out of the patient’s line of sight and allowed the Ob/Gyn and her resident to spend some final moments with her. The scene was both tense, and yet supportive of the patient.
I initiated rapid sequence intubation with the assistance of the anesthesiologist, and then moved to get the ultrasound machine to visualize the uterus and its contents. Much to my discomfort the fetus was fairly large – and was moving around normally, even sucking its thumb at one point. I asked the Ob/Gyn resident why the fetus was being aborted since it didn’t appear to have any structural abnormalities. She responded that the mother simply didn’t want to have the baby, and had wrestled with the idea of abortion for a long time before she made her final decision.
The rest of the procedure is a bit of a blur – with details too graphic to describe here. But suffice it to say that the resident performing the dilatation and curettage had a fairly difficult time removing the fetus through the cervix, and had to resort to eliminating it in smaller parts, rather than a whole. It was very sad and it took a long time to make sure that the uterus was fully evacuated. I decided that I couldn’t watch another one of these procedures.
The rest of my female abdominal ultrasound experience was obtained at a Planned Parenthood center where very early abortions were performed. Generally, this consisted of suctioning out a tiny yolk sac (and “products of conception”) – without much of a recognizable fetus in the midst. Although these procedures were certainly emotional, they were somewhat less troubling than the later term dilatation and curettage.
What I didn’t expect, however, was that of the approximately 100 abortions I witnessed – none (to my knowledge) of the women requesting them were rape victims, nor was there a life-threatening birth defect in the fetus. Usually the reason they gave was psychological, emotional, or financial – “I just can’t afford to raise a child” or “This is not a good time for me to be pregnant” or “I don’t want this baby” or “I don’t want another baby” or “This was an accident, and I don’t want it to ruin my life.”
I did my very best to adopt an attitude much like the one that the author of the Washington Post article did – “It’s not for me to judge the validity of someone else’s reasons for wanting an abortion… They’re going to do it anyway so physicians need to make sure they’re safe… Women have the right to choose…”
But the reality was that those attitudes didn’t prepare me for the emotional turmoil inherent in the process of abortion. It’s sadder than I thought, more difficult than I thought… and the impact is farther reaching than I imagined. Studies estimate that about 1/3 of US women have an abortion at some point in their lives – that’s a heavy emotional burden that many women carry in silence.
In my opinion women should have the right to choose to have an abortion, but I’d hope that they also consider their right to choose to give their baby up for adoption as well. Some believe that an abortion is “easier” than giving up a baby for adoption – but I’m not so sure that’s the case from an emotional perspective. As far as rape victims or women who are carrying a moribund fetus – the decision to abort may well be emotionally less damaging. But for the majority of women who have abortions for less clear reasons (reasons like the ones I witnessed), I’d really encourage them to consider adoption as an option. Obviously, these decisions are intensely personal and have to be made on a case-by-case basis – and women should be supported either way.
As scientific and rational as I wanted to be about the procedure, I am still troubled by what I experienced as a witness to various abortions. Though I might have “entered the abortion conversation” as the third-year medical student did – after witnessing quite a few, I have a deeper appreciation for the emotional complexity of abortion, and a desire to help women avoid them if at all possible. I wonder if the author of the Washington Post article will change her perspective after she’s witnessed a few of the procedures?
June 8th, 2009 by Emergiblog in Better Health Network
2 Comments »

You walk into the unit, put down your backpack, fill your pocket with pen, scissors, and tape, sling the stethoscope over your neck, swipe your namebadge into the infernal timeclock and enter stage right.
It’s showtime!
Get the triage, hook up the monitor, grab the EKG, slam in the saline lock – grab the bloods in the process, hang a liter of normal saline, put up the side rails, hook the call bell to the side rail, throw on a warm blanket, medicate for fever and slam the chart in the “to-be-seen” rack.
Repeat x 30 over the next eight hours.
Feel like burnt toast, look like burnt toast, act like burnt toast.
*****
Where’s the patient?
You know, the person you just triaged, hooked, slammed, hydrated, side-railed, blanketed, medicated and lined up for evaluation?
Oh.
Did it ever occur to you that the reason you feel like burnt toast is because you are so focused on what you are doing you have lost sight of the “who” you are doing it to?
*****
Well, it occurred to me.
Because that is exactly what had happened.
Oh, my physical care was fine.
But I had stopped looking patients in the eye. I was spitting out standard responses instead of listening to what my patients were saying. I was expending the bare minimum of energy required to complete tasks.
I was doing; I wasn’t caring.
And I was burnt.
*****
But I discovered something.
And this is huge.
I was not focusing on tasks because I had burned out, I burned out because I had started focusing on tasks.
Let’s face it. The ER, while seemingly exciting to those outside the ambulance doors, can actually feel redundant to those of us who deal with the same issues every day. The same complaints. The same symptoms. Over and over and over.
So, what makes each case interesting? What makes each case unique?
The patient behind the story. The person under the symptoms.
Lose sight of the person and you lose sight of the profession. Lose sight of their humanity and you lose sight of your own. Lose sight of your own and you become a burnt shell.
*****
You would think that after three decades of this, I’d have figured this out by now.
I guess you never stop learning.
This time, my teachers were an elderly man with a DVT who talked to me about his time on the LAPD, back in the day.
And the young woman who described, quite vividly, how it felt to go from the pinnacle of health to the devastation of a cancer diagnosis, overnight.
Or the 18-month old who tucked their head under my chin and fell asleep as Mom described the terror of witnessing a first-time febrile seizure.
*****
Who would have guessed that sometimes patients are the cure for burn out and not the cause of burn out.
The patients didn’t change, they were always willing to talk.
All I had to do was stop and listen.
That simple.
Go figure.
*This blog post was originally published at Emergiblog*
June 8th, 2009 by KerriSparling in Better Health Network, Patient Interviews
No Comments »

Even though I do not like the disease, there are some diabetes-related simple pleasures that make me smile:
- I like when I change the battery and the insulin reservoir at the same time. Having my Medtronic 522 “full” on both sides makes me happy.
- I like when the carb count on something is exactly 10 grams of carbs because it matches my insulin to carb ration precisely. One snack, one unit, one oddly happy Kerri.
- I like the sound of the pump counting up a bolus. Boop boop beep!
- I like when the sound of the bolus is caught by Chris and he ends up whistling it back to me, almost without thinking. It’s a little soundtrack snippet of our life.
- I like when the cats wait patiently for me to remove the pump tubing from my body before they lunge for it.
- I like when new boxes of diabetes supplies show up and I can organize them in my little OCD supply closet.
- I like when the number on my meter is two digits, but higher than 89 mg/dl. It’s a tight range, I’m not usually in it, but it brings me weird joy.
- I like when the Dexcom beeps and my coworker (who works a wall away from me) IMs me quietly to check, “Low?” because she’s ready to get juice if necessary.
- I like not having to wear a watch.

- I like when I get to dump all the used test strips that have piled up throughout the day. Knowing I’ve tested a bunch makes me feel like I really stayed tuned in.
- I like the smell of white glucose tabs.
- I like when the new infusion set doesn’t sting at all.
- I like having someone in my life who is willing to get their hands covered in SkinTac in an attempt to stick a Dexcom sensor to random places on my body.
- I like that the hope of the parents of kids with diabetes rubs off on me, and makes me feel good for even just a few minutes.
- I like that diabetes gives two people, who wouldn’t otherwise have a thing to say to one another, a whole dinner’s worth of conversation.
- I like having coworkers who understand but don’t push.
- I like when my best friend clinks her beer to mine and says, “Bolus, baby.”
- I like when the cat licks my hand after I test.
- I like “free shower:” a shower without a pump site or a CGM sensor attached.
- I like having a whole network of people who understand – and do not judge – my diabetes life.
I like when I can focus on the silly, simple things when I feel a little overwhelmed by the tough stuff.
*This blog post was originally published at Six Until Me.*
June 8th, 2009 by Shadowfax in Better Health Network, Opinion
No Comments »

Bob Wachter, who I generally like and admire, takes on the topic of hospital peer review, stimulated by a
report issued by Public Citizen’s Health, that hospitals rarely report physicians to the National Practitioner Data Bank:
Wachter’s World : Is Hospital Peer Review a Sham? Well, Mostly Yes
Although the public cannot access NPDB reports on individual physicians, healthcare organizations (mostly hospitals) ping the database about 4 million times per year. When it was inaugurated, the best estimates (including those of the AMA) were that the NPDB would receive 5,000-10,000 physician reports each year.
Not so much. Since its launch two decades ago, NPDB reports have averaged 650/year, and nearly half of US hospitals (2845 of 5823) have never reported a single physician! The most extreme case is that of South Dakota, where three-quarters of the hospitals have never reported a single case to the NPDB. I’m sure South Dakota has some wonderful doctors, but the idea that the state’s 56 hospitals have not had a single physician who needed to be suspended for incompetence, substance abuse, sexual harassment, or disruptive behavior since the Reagan presidency is a bit of a stretch, don’t you think?
And on the merits of the matter, it’s hard to dispute that the NPDB has been an abject failure as far as its original goal went: it is not an effective data bank collecting data on suspect and problematic physicians. I think that Public Citizen and Dr Wachter transpose cause and effect, though, when they attribute the blame to the peer review process. The fault, I think lies in the NPBD itself.
The goal may have been laudable and simple — get in trouble, get a file, and keep bad doctors from hurting patients. Wow. Who could oppose something like that? But that’s not how it worked out in the real world. Perhaps it’s a consequence of the fact that it is so infrequently used, but the reality is that being in the NPDB is incredibly stigmatizing, which is not a matter limited to the ego of the reported physician, but also is an essential death sentence to his or her career. This is not a “Oh dear, now I’ll never be Chief of Staff,” sort of career disruption — being in the data bank makes a physician essentially unemployable.
And that’s why it’s shunned: it often seems unjust. There’s no proportionality, no way to indicate the gravity of the transgression, because the full details behind a report are screened from view. Molesting a patient and telling dirty jokes in the OR both show up as “sexual impropriety.” An isolated mistake or an episode of poor judgment is impossible to distinguish from incompetence, as both are filed as “quality of care deficiencies.” When the only punishment is the ultimate one, it’s no suprise that medical staffs are loathe to invoke it.
And it’s expensive. Since a physician at risk of a medical staff action usually knows how high the stakes are, they will commonly lawyer up and fight tooth and nail to prevent any blot on their record. The legal bills for these cases can run into the hundreds of thousands of dollars, and even if the hospital “wins,” all they’ve done is spend a ton of money to get rid of a problem. If they can get rid of him or her for free with a negotiated sham resolution, why would they go through all the expense to persecute the poor bastard as well?
Much of the same can be said for the state licensing boards, to which medical staff committees are also responsible for reporting of suspensions and revocations of privileges.
So, I think it should be noted that this is not a simple “docs are too softhearted to police themselves” issue. It’s that the legal and regulatory tools we have been given are too blunt and indiscriminate for those of us wielding them to feel that they are useful and fair in the vast majority of cases.
Because the true case of the dangerous/incompetent/morally unfit physician is relatively uncommon. Dr Wachter falls right into the false “Good doc/bad doc” dichotomy and buys into the assumption that there is a large cohort of “Bad Doctors” out there that we need to drum out of the profession. There are some, I am sure, but I’ve rarely seen one at our hospitals, and they’re actually quite easy to deal with when you come across them. It’s the gray cases, which comprise the majority of the head-scratchers that we have to deal with in the hospital. It’s the surgeon whose patients love him but just seem to have a lot of complications. It’s the doc who manages to pick a fight with every other member of the medical staff but never quite crosses any bright lines. It’s the creepy male doc who makes all the nurses uncomfortable but never really touches where he shouldn’t. The “incompetent” doc who you wouldn’t let care for your family member but seems to muddle by just well enough to keep from killing anyone.
You all know the one I’m talking about, right? But it can be tough to identify an incompetent doc. I’ve never yet met one whose ID badge or diploma listed them as “incompetent.” In many cases, there’s a legitimate defense to the care provided, even if it’s a weak defense. In many cases an error or errors may have been genuine and severe, but not characteristic of the doc’s general level of quality. The cut and dried “you suck” level of incompetence is rare and far overshadowed by the many cases of borderline physician skills.
The “Bad Doc” approach to this matter also makes the error of assuming that a problem doc is irredeemable and must be expelled from the order. I’ve seen docs who rose and fell and rose again over the long arcs of a career. Some of them needed to go through a formal, sanctioned process involving chemical dependency treatment, most often. Others, however, simply needed attention and managerial support: focused redirection, re-education, sensitivity training or the like, and with appropriate supervision they are able to continue practice. Reporting them to the NPDB is not a solution, at least not a defensible one in the “typical” borderline case. Sometimes you can counsel them or devise a practice plan that works to keep patients safe and the hospital harmonious. But the adversarial relationship makes this hard enough, and the need to carefully work around this death threat of the NPDB is a burden and an impediment to working collaboratively with the “challenged” physicians.
None of this is intended to be a defense for the truly impaired, incompetent, or sociopathic docs out there, or the medical staffs who have enabled them. I’m sure that the problem exists to some degree. But the idea that the NPDB is a valuable or even a positive tool in the vast majority of cases is itself laughable. It was a great idea but as implemented it has been an abject failure. The high-handed folks over at Public Citizen will never admit to it, will never modify it in ways that might make it more functional. They will, rather, rail against the scofflaw docs and hospitals who do not deign to use this blunt and ineffective instrument which has been thrust upon us. And we, working away on Medical Exec and Credentials Committees will be left with ad hoc and jury-rigged approaches to the borderline physicians who represent the more common and more challenging dilemmas in the industry.
*This blog post was originally published at Movin' Meat*
June 7th, 2009 by David H. Gorski, M.D., Ph.D. in Better Health Network, Quackery Exposed
5 Comments »

 Unfortunately, a frequent topic on SBM has been the anti-vaccine movement, personified these days by celebrity spokesmodel for Generation Rescue Jenny McCarthy and her boyfriend comedian and actor Jim Carrey. Unfortunately, it is a topic that is unlikely to go away. We’ve all speculated why the anti-scientific emotion-based notion that vaccines somehow must cause autism persists in spite of mountains of evidence to the contrary, but I think the question goes much deeper than that because it’s not just about vaccines. The anti-vaccine movement is but one of the most visible components of a much deeper problem in our public discourse, a problem that values feelings and personal experience over evidence, compelling stories and anecdotes over science.
Unfortunately, a frequent topic on SBM has been the anti-vaccine movement, personified these days by celebrity spokesmodel for Generation Rescue Jenny McCarthy and her boyfriend comedian and actor Jim Carrey. Unfortunately, it is a topic that is unlikely to go away. We’ve all speculated why the anti-scientific emotion-based notion that vaccines somehow must cause autism persists in spite of mountains of evidence to the contrary, but I think the question goes much deeper than that because it’s not just about vaccines. The anti-vaccine movement is but one of the most visible components of a much deeper problem in our public discourse, a problem that values feelings and personal experience over evidence, compelling stories and anecdotes over science.
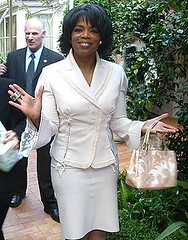
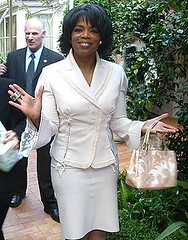
I’m referring to the Oprah-fication of medicine in America.
Why Oprah? you may ask. I’m happy to tell you. Oprah Winfrey has been the host of the highest rated syndicated talk show in television history, her self-named The Oprah Winfrey Show. The show has been running for nearly 23 years, with over 3,000 episodes. Winfrey is so famous that she is one of those rare celebrities who is known instantly by just her first name. Say “Oprah,” and virtually everyone will know to whom you’re referring, and her show is often colloquially known as simply Oprah. Given this unprecedented level of success, which has made Oprah a billionaire and a ubiquitous presence on TV, her own magazine, her own satellite radio station, and, soon, her own cable channel, Oprah has developed a media empire that few single individuals can match or beat. Indeed Rupert Murdoch is the only person that I can think of who likely has a wider reach than Oprah. Personally, I have no problem with Oprah’s level of success. Clearly, she is a very talented and savvy TV host and businesswoman.
Unfortunately, in marked contrast, Oprah has about as close to no critical thinking skills when it comes to science and medicine as I’ve ever seen, and she uses the vast power and influence her TV show and media empire give her in order to subject the world to her special brand of mystical New Age thinking and belief in various forms of what can only be characterized as dubious medical therapies at best and quackery at worst. Arguably there is no single person in the world with more influence pushing woo than Oprah. Indeed, she puts Prince Charles to shame, and Kevin Trudeau is a mere ant compared to the juggernaught that is Oprah Winfrey’s media empire. No one even comes close. No one, and I mean no one, brings pseudoscience, quackery, and antivaccine madness to more people than Oprah Winfrey does every week. (She doesn’t discuss such topics every day, but it seems that at least once a week she does.) Naturally, Oprah doesn’t see it that way and likely no one could ever convince her of the malign effect she has on the national zeitgeist with respect to science and medicine, but that’s exactly what she does. Consequently, whether fair or unfair, she represents the perfect face to put on the problem that we supporters of science-based medicine face when trying to get the message out to the average reader about unscientific medical practices, and that’s why I am referring to the pervasiveness of pseudoscience infiltrating medicine as the “Oprah-fication” of medicine.
Read more »
*This blog post was originally published at Science-Based Medicine*