Credibility & Prestige In Medicine: How Are They Measured?
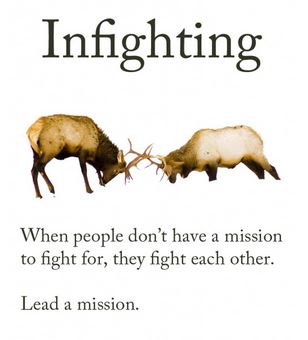 In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
Interestingly, the credibility question was raised in a different light when I was recently contacted by a prestigious medical organization that was seeking expansion of its board membership. I presumed that this was a personal invitation to join the cause, but soon realized that the caller wanted to use my influence to locate “more credible” candidates with academic gravitas.
When I asked what sort of candidate they wanted my help to find, the response was:
“A physician with an academic appointment at a name brand medical school. Someone who isn’t crazy – you know, they have to be respected by their peers. Someone at Harvard or Columbia would be great. You must know someone from your training program at least.”
While I appreciated the honesty, I began thinking about the age-old “town versus gown” hostilities inspired by academic elitism. In medicine, as with many other professions, it is more prestigious to hold an academic position than to serve in a rural community. But why do we insist on equating credibility with academics?
Another facet of credibility lies in physicians’ tendencies to admire only those at the top of their specific specialty. Dr. Lucy Hornstein described this phenomenon in her powerful essay on “How To Drive Doctors To Suicide:”
“Practice that condescending look and use it at hospital staff events. Make it a point to ignore newcomers. Concentrate on talking just with your friends and laughing at inside jokes, especially when others are around. Don’t return their calls, and don’t take their calls if you can possibly help it. If you accidentally wind up on the phone with the patient’s primary physician, just tell them you’ve got it all under control, and that he (and the patient) are so lucky you got involved when you did.”
A reader notes:
“And perhaps those of us who do see patients should get some self esteem and stop fawning all over [physician thought leaders] at conferences like needy interns.”
And finally, there seems to be an unspoken pecking order among physicians regarding the relative prestige of various specialties. How this order came about must be fairly complicated, as dermatology and neurosurgery seem to by vying for top spots these days. I find the juxtaposition almost amusing. Nevertheless, it’s common to find physicians in the more popular specialties looking down upon the worker bees (e.g. hospitalists and family physicians) and oddballs (e.g. physiatrists and pathologists).
While I try very hard not to take offense at my peers’ dismissiveness of my career’s value, it becomes much more concerning when funding follows prejudicial lines in the medical hierarchy. As a sympathetic family physician writes:
“I have observed the inequitable distribution of resources from the less glamorous to the sexy sub specialties despite obvious patient needs. Unfortunately, the administridiots who usually lack any medical training, opt to place resources where they are most likely to attract headlines.”
Yes, caring for the disabled (PM&R) is “less glamorous” than wielding a colonoscope (GI) (again, not sure who made that decision?) but it should not be less credible, or become a target for budget cuts simply because people aren’t informed about how rehab works.
It is time to stop specialty prejudice and honor those who demonstrate passion for patients, regardless of which patient population, body part, or organ system they serve. Excellent patient care may be provided by academics, generalists, or specialists, by those who practice in rural areas or in urban centers. The best “thought leaders” are those who bring unity and an attitude of peer respect to the medical profession. With more of them, we may yet save ourselves from mutually assured destruction.
















