September 9th, 2015 by Dr. Val Jones in Health Tips, True Stories
1 Comment »

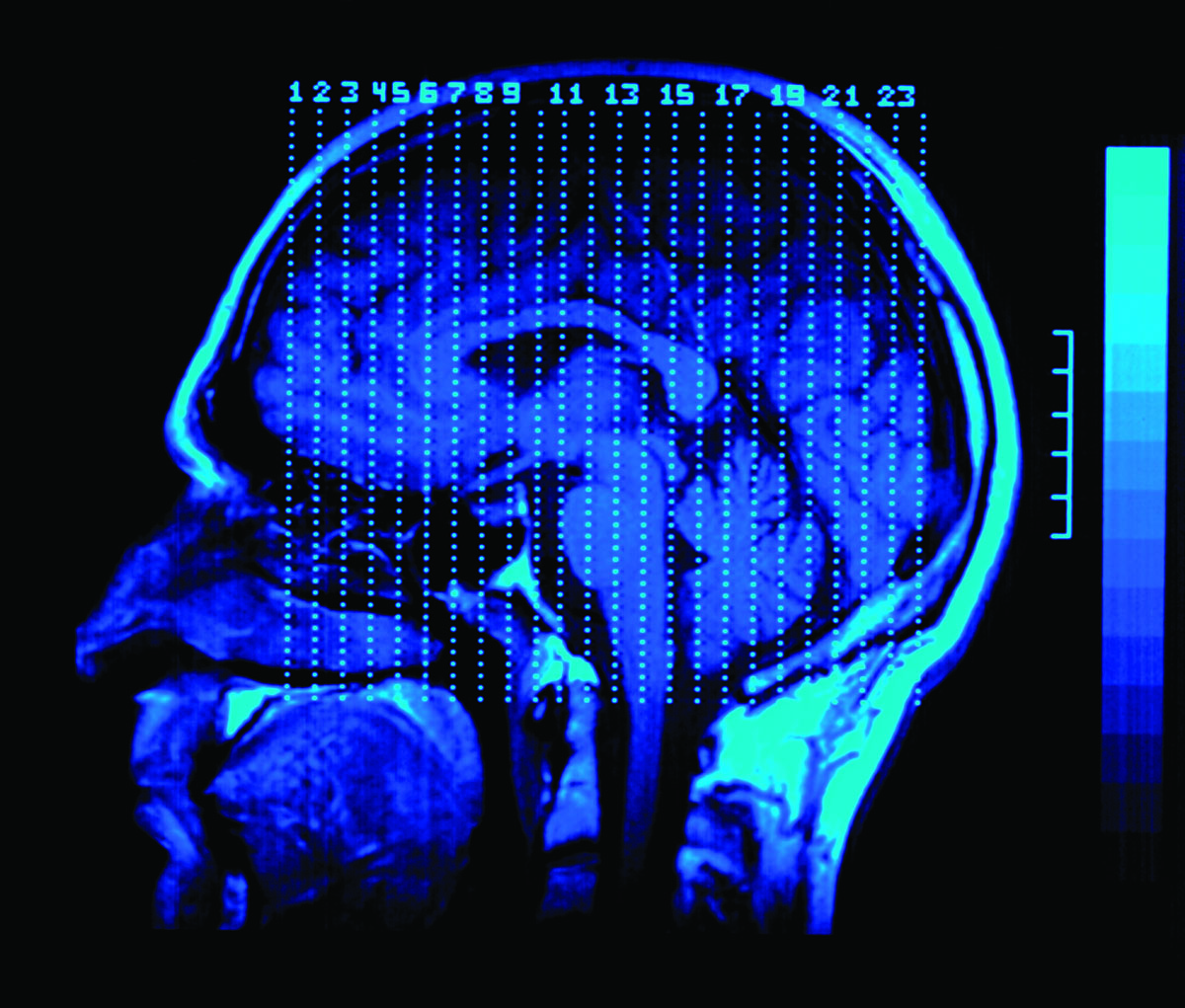
Photo Cred: Max S. Gerber
I learned a valuable lesson recently about how difficult it can be to make the correct diagnosis when you see a patient for a very short period of time. In the acute rehab setting I admit patients who are recovering from severe, life-altering brain events such as strokes, head injuries, and complex medical illnesses. It is challenging to know what these patients’ usual mental function was prior to their injuries, and so I rely on my knowledge of neuroanatomy, infectious disease, and pharmacology to guide my work up. However, I have learned that asking the patient’s family members about what they were like (in their healthier state) is extremely important as well. Personality quirks, likes and dislikes, and psychiatric history all offer clues to ongoing behavioral challenges and mental status changes.
This fact was never clearer than when I met an elderly gentleman with a new stroke. He was extremely drowsy, non-participatory, and was not oriented to anything but his name. The stroke had occurred in a part of the brain that does not affect cognition, so I began to wonder if he had an infection or was having a reaction to a medication. I carefully ruled out all possible sources of infection, and I combed through his medication list and removed any potentially sedating drugs. His mental status remained unchanged for several days. I then began to wonder if perhaps he was suffering from significant dementia at baseline, and that he was living at home with more help from his family than they had initially reported. The therapy team and I began to consider a transfer to a nursing home. The family was horrified by the idea.
As it turned out, his grandson shared with me that he believed that the patient was autistic. Because his grandpa was elderly, he grew up in a time where not much was known about autism, and diagnoses of the condition was rarely made. He was therefore never formally diagnosed, but had many of the textbook characteristics. His stroke, combined with a sudden transfer to an inpatient hospital setting, was very distressing for the patient, and he had shut down to protect himself from the mental anguish. The “dementia-like” behavior that we were witnessing was merely an acute psychological reaction.
Armed with this new information, the therapy team requested family members to be present during all sessions – to encourage participation and to provide comfort and normalization of the transition from home to hospital. The patient responded beautifully, and made remarkable gains in his ability to walk and participate in self care activities.
I apologized profusely to the family for our period of confusion about his diagnosis and care needs, and offered reassurance that we would do our very best to help him recover from his stroke so that he could go home directly from the hospital. He did in fact return home, and with a little extra help from his daughters, he is enjoying his usual projects and activities.
As for me, I will never presume dementia without careful family confirmation again.
March 31st, 2011 by admin in Health Policy, Health Tips, Research
No Comments »
By Richard C. Hunt, MD, FACEP
Centers for Disease Control and Prevention
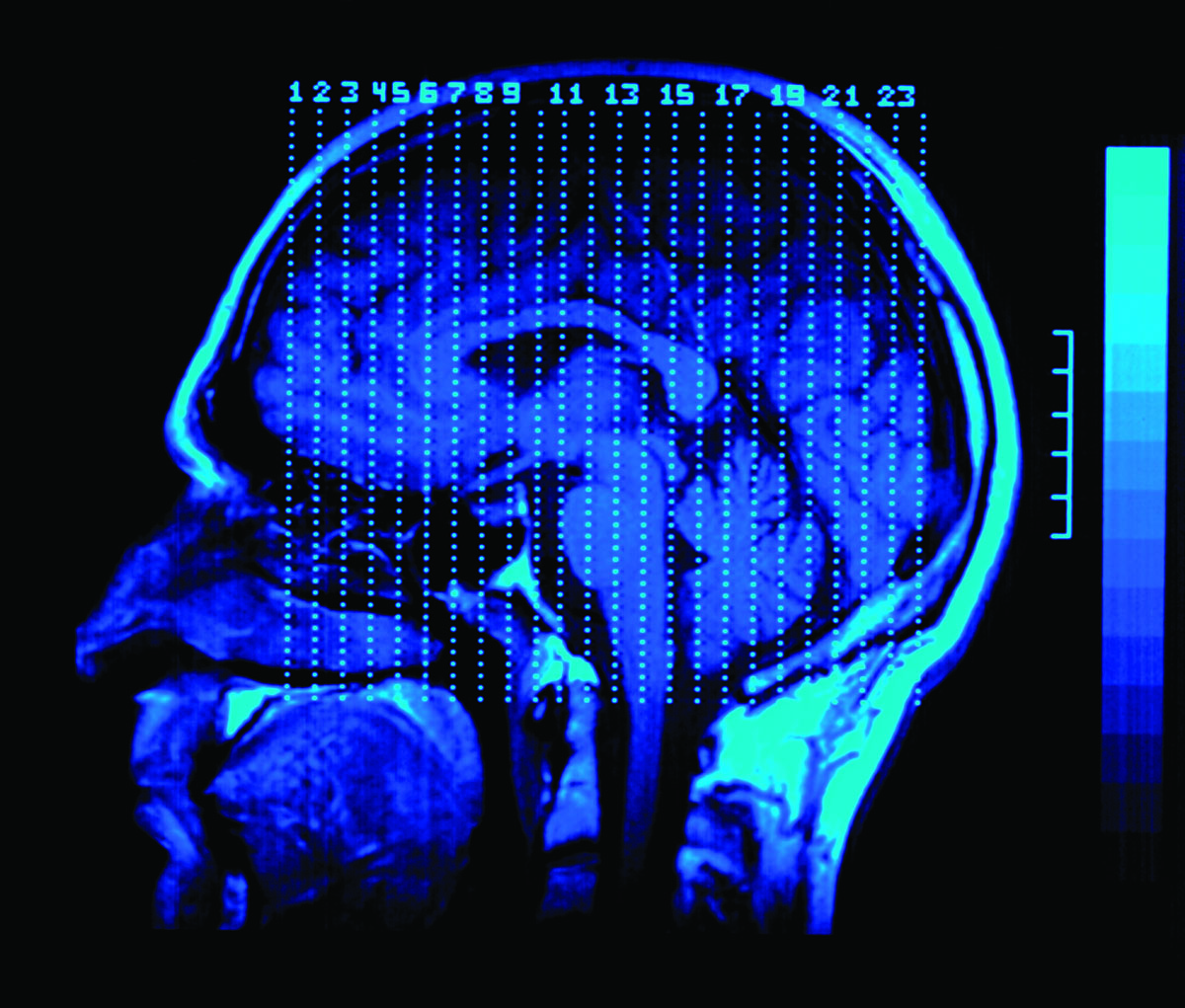
A 17 year-old athlete arrives on the sideline, at your office, or in the emergency department after hitting her head during a collision on the sports field and is complaining that she has a headache and “just doesn’t feel right.”
Can she return to play? If not, when can she safely return to school, sports, and to her normal daily activities? Does she need immediate care, a Head CT or MRI, or just some time to rest?
Do those questions sound familiar?
Each year thousands of young athletes present at emergency departments and in the primary care setting with a suspected sports- and recreation-related concussion. And every day, health care professionals, like us, are challenged with identifying and appropriately managing patients who may be at risk for short- or long-term problems.
As you know, concussion symptoms may appear mild, but this injury can lead to significant, life-long impairment affecting an individual’s ability to function physically, cognitively, and psychologically. Thus, appropriate diagnosis, referral, and education are critical for helping young athletes with concussion achieve optimal recovery and to reduce or avoid significant sequelae.
And that’s where you come in. Health care professionals play a key role in helping to prevent concussion and in appropriately identifying, diagnosing, and managing it when it does occur. Health care professionals can also improve patient outcomes by implementing early management and appropriate referral.
As part of my work at CDC, and as a health care professional, I am committed to informing others about CDC’s resources to help with diagnosing and managing concussion. CDC collaborated with several organizations and leading experts to develop a clinical guideline and tools for the diagnosis and management of patients with concussion, including:
For more information about the diagnosis and management of concussion, please visit www.cdc.gov/Concussion/clinician.html.
Also, learn more about CDC’s TBI activities and join the conversation at: www.facebook.com/cdcheadsup.
February 19th, 2010 by Medgadget in Better Health Network, News, Research
No Comments »

 Have Caltech scientists discovered an area of the brain evolved since the development of currency? The headline effectively suggests that, but the truth is probably a bit more nuanced.
Have Caltech scientists discovered an area of the brain evolved since the development of currency? The headline effectively suggests that, but the truth is probably a bit more nuanced.
The research team responsible for these findings consists of Benedetto de Martino, a Caltech visiting researcher from University College London and first author on the study, along with Caltech scientists Colin Camerer, the Robert Kirby Professor of Behavioral Economics, and Ralph Adolphs, the Bren Professor of Psychology and Neuroscience and professor of biology.
The study involved an examination of two patients whose amygdalae had been destroyed due to a very rare genetic disease; those patients, along with individuals without amygdala damage, volunteered to participate in a simple experimental economics task. Read more »
*This blog post was originally published at Medgadget*




 Have Caltech scientists discovered an area of the brain evolved since the development of currency? The headline effectively suggests that, but the truth is probably a bit more nuanced.
Have Caltech scientists discovered an area of the brain evolved since the development of currency? The headline effectively suggests that, but the truth is probably a bit more nuanced.







