December 23rd, 2011 by Steve Novella, M.D. in Quackery Exposed
No Comments »

 There are many medical pseudosciences that persist despite a utter lack of either plausibility or evidence for efficacy. Some practices emerged out of their culture of origin, or out of the prevailing ideas of a pre-scientific age, while others were manufactured out of the imagination of perhaps well-meaning but highly misguided individual practitioners. They were just made up – homeopathy, for example, or subluxation theory.
There are many medical pseudosciences that persist despite a utter lack of either plausibility or evidence for efficacy. Some practices emerged out of their culture of origin, or out of the prevailing ideas of a pre-scientific age, while others were manufactured out of the imagination of perhaps well-meaning but highly misguided individual practitioners. They were just made up – homeopathy, for example, or subluxation theory.
Iridology belongs to this latter category – a system of diagnosis that was invented entirely by Ignatz Peczely, a Hungarian physician who first published his ideas in 1893. The story goes that Peczely as a boy found an owl with a broken leg. At the time he noticed a prominent black stripe in the iris of one eye of the owl. He nursed the bird back to health and then noticed that the black line was gone, replaced by ragged white lines. From this single observation Peczely developed the notion of iridology.
Peczely’s idea was that the iris maps to the rest of the body in some way, and therefore the flecks of color in the iris reflect the state of health of the various body parts. This basic approach to diagnosis or treatment is called the homonculus approach – the idea that one part of the body maps to the rest of the body, including the organ systems. Reflexology, auricular acupuncture, and even straight chiropractic follow this approach.
This is what might have happened next: Read more »
*This blog post was originally published at Science-Based Medicine*
December 3rd, 2011 by Elaine Schattner, M.D. in Opinion, Research
No Comments »

The latest issue of the Annals of Internal Medicine contains 2 noteworthy papers on cervical cancer screening. The first, a systematic review of studies commissioned by the USPSTF, looked at 3 methods for evaluating abnormalities in women over 30 years:
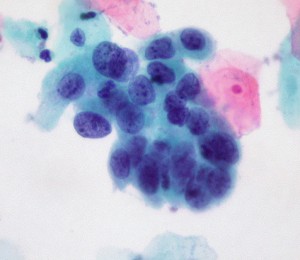
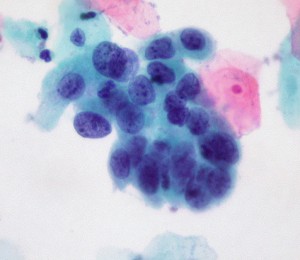
high-grade cervical cell dysplasia (Dr. E. Uthman, Wikimedia Commons)
1. Conventional cytology (as in a Pap smear; the cervix is scraped and cells splayed onto a microscope slide for examination);
2. Liquid-based cytology (for LBC, the NHS explains: the sample is taken as for a Pap test, but the tip of the collection spatula is inserted into fluid rather than applied to slides. The fluid is sent to the path lab for analysis);
3. Testing for high-risk HPV (human papillomavirus). Currently 3 tests have been approved by the FDA in women with atypical cervical cells or for cervical cancer risk assessment in women over the age of 30: Digene Hybrid Capture 2 (manufactured by Quiagen), Cobas 4800 HPV (Roche) and Cervista HR HPV (Hologic); another Roche Diagnostics assay, Amplicor HPV, awaits approval.
These HPV assays use distinct methods to assess DNA of various HPV strains.
There’s a lot of jargon here, and I have to admit some of this was new to me despite my nearly-due diligence as a patient at the gynecologist’s office and my familiarity as an oncologist with the staging, clinical manifestations and treatment of cervical cancer. Who knew so many decisions were made during a routine pelvic exam about which manner of screening? Read more »
*This blog post was originally published at Medical Lessons*
October 16th, 2011 by Elaine Schattner, M.D. in Research
No Comments »

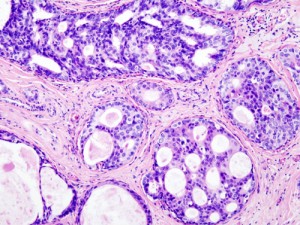
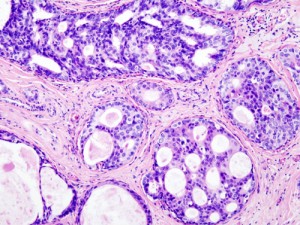
Ductal Carcinoma in Situ (DCIS) in the breast, histopathology w/ hematoxylin & eosin stain, Wiki-Commons image
More, a magazine “for women of style & substance,” has an unusually thorough, now-available article by Nancy F. Smith in its September issue on A Breast Cancer You May Not Need to Treat.
The article’s subject is DCIS (Ductal Carcinoma in Situ). This non-invasive, “Stage 0” malignancy of the breast has shot up in reported incidence over the past two decades. It’s one of the so-called slow-growing tumors detected by mammography; a woman can have DCIS without a mass or invasive breast cancer.
While some people with this diagnosis choose to have surgery, radiation or hormonal treatments, others opt for a watchful waiting strategy. The article quotes several physicians, including oncologists, who consider Read more »
*This blog post was originally published at Medical Lessons*
September 11th, 2011 by Happy Hospitalist in Health Policy, Opinion
No Comments »

Missed Diagnosis Lawsuit and the Dynamics of Age Related to Risk
Years ago I had the opportunity to care for Mr Smith, a 101 year old man who presented to the hospital with chest pain and shortness of breath. Besides having 101 year old heart and lungs that tend to follow their own biological clock, this man also had a massive chest tumor filling 85% of one side of his thorax.
Whoah really? What does that mean in a 101 year old man? Most folks this age have exceeded the normal bell curve distribution of life and disease. When you reach 101 years old, there isn’t a lot of chronic anything you can catch with the expected time you have left on earth.
Every now and then, however, we find patients who are the exception to the rule, such as the 101 year old guy that present with a new cancer diagnosis. That’s where being an internist comes in handy. Read more »
*This blog post was originally published at The Happy Hospitalist*
September 1st, 2011 by AndrewSchorr in Interviews, News
No Comments »


Pat Elliott, me and a HUGE cactus at Banner MD Anderson!
I am just back from the Phoenix-metro area. It’s now the 5th largest in the United States and despite home foreclosures, there is still a feeling of growth in many areas. Gilbert, a nearby suburb, has expanded to over 200,000 people and a growing major medical center. I spent several days interviewing patients and staff about the soon-to-open, Banner MD Anderson Cancer Center. The hope is that by bringing MD Anderson’s world-renowned expertise, clinical trials and processes to this new center, cancer care around Phoenix and the southwest will be improved. Look for my video interviews coming soon.
But, in the meantime, one interview stuck out for me; the one with the Banner Health President and CEO, Peter Fine. Peter is in his late 50s and is a health care industry professional who has been guiding Banner Health and its 23 hospitals well for over a decade. For the past several years, Peter has been strategizing the building of a major cancer center on one of his hospital campuses. Peter knew he would need a renowned partner to make it successful and three years ago he chose MD Anderson Cancer Center, in Houston, consistently ranked as the nation’s #1 cancer center (and where I was treated in a leukemia clinical trial).
Even before the partnership contract was inked, a strange thing happened. Peter found a swollen lymph node in his neck and it didn’t go away. Read more »
*This blog post was originally published at Andrew's Blog*
 There are many medical pseudosciences that persist despite a utter lack of either plausibility or evidence for efficacy. Some practices emerged out of their culture of origin, or out of the prevailing ideas of a pre-scientific age, while others were manufactured out of the imagination of perhaps well-meaning but highly misguided individual practitioners. They were just made up – homeopathy, for example, or subluxation theory.
There are many medical pseudosciences that persist despite a utter lack of either plausibility or evidence for efficacy. Some practices emerged out of their culture of origin, or out of the prevailing ideas of a pre-scientific age, while others were manufactured out of the imagination of perhaps well-meaning but highly misguided individual practitioners. They were just made up – homeopathy, for example, or subluxation theory.