November 10th, 2011 by PreparedPatient in Expert Interviews
No Comments »

This interview is the ninth and final of a series of brief chats between CFAH president and founder, Jessie Gruman, and experts—our CFAH William Ziff Fellows—who have devoted their careers to understanding and encouraging people’s engagement in their health and health care.
 Trudy Lieberman is concerned that despite all the rhetoric, choosing the best hospital, the best doctor, the best health plan, is simply not possible. Some of the so-called best might be good for some people but not others, and the information available to inform/guide choices is just too ambiguous.
Trudy Lieberman is concerned that despite all the rhetoric, choosing the best hospital, the best doctor, the best health plan, is simply not possible. Some of the so-called best might be good for some people but not others, and the information available to inform/guide choices is just too ambiguous.
Ms. Lieberman is a CFAH William Ziff Fellow.

Gruman: What has changed in the past year that has influenced people’s engagement in their health and health care?
Lieberman: Costs have risen a lot, and employers and insurers have made consumers pay higher deductibles, co-pays and coinsurance. The theory is, Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
October 11th, 2011 by DavedeBronkart in Health Policy, Opinion
No Comments »

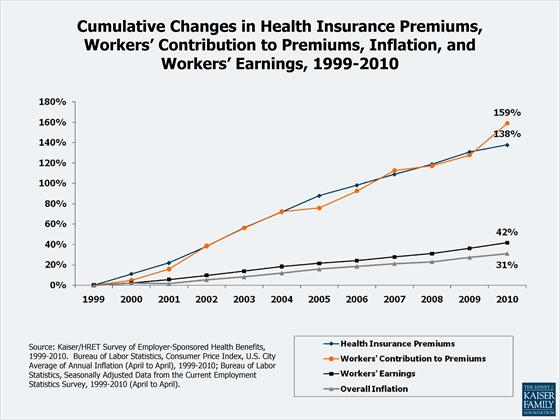
Last week the New York Times reported that some health insurers have applied to regulatory agencies to push premiums sharply higher – usually double-digit increases, while citizens are suffering. This falls on top of the 11 year history reported last year by the Kaiser Family Foundation: wages and inflation are up ~40%, while health costs and worker contributions were up 138% and 159%:
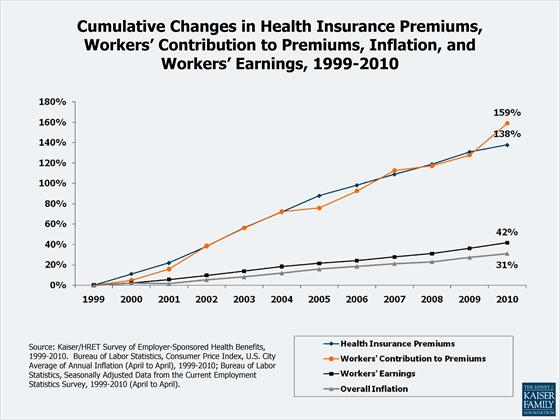
No wonder we feel squeezed. (Last week’s announcement comes on top of this history.)
This has enormous human impact. Read more »
*This blog post was originally published at e-Patients.net*
July 19th, 2011 by PreparedPatient in Opinion
No Comments »

Glenn Laffel, M.D., Ph.D., of Pizaazz hypothesizes about why we often don’t make changes that would benefit our health. He says:
“Somewhere in the course of our daily lives, though, most of us do exhibit behavior that suggests at least some disregard for our health. We don’t change our diet, though we know we should. We don’t floss, take medications as prescribed, or get the screening tests we’re supposed to.”
He knows multiple complex causes exist for this and questions whether being diagnosed with a chronic condition motivates people to improve health behaviors exploring whether the delay between health behaviors and health outcomes contributes to unhealthy behavior. After looking at attrition rates in a diabetes self-management program, he concludes:
“It calls attention to a key distinction behavioral psychologists like to make in explaining human motivation: there’s a difference between awareness of the need to act, and the volition to act.”
Family doctor Kenny Lin, M.D., previously recommended that people “tackle one behavior at a time.” He says: Read more »
*This blog post was originally published at Prepared Patient Forum: What It Takes Blog*
March 2nd, 2011 by Jessie Gruman, Ph.D. in Better Health Network, Opinion
1 Comment »

 The other day I came across this photo of a couple clasping each other in a dramatic tango on the cover of an old medical journal — a special issue from 1999 that was focused entirely on doctor-patient partnership. The tone and subjects of the articles, letters and editorials were identical to those written today on the topic: “It’s time for the paternalism of the relationship between doctors and patients to be transformed into a partnership;” “There are benefits to this change and dangers to maintaining the status quo;” “Some doctors and patients resist the change and some embrace it: Why?”
The other day I came across this photo of a couple clasping each other in a dramatic tango on the cover of an old medical journal — a special issue from 1999 that was focused entirely on doctor-patient partnership. The tone and subjects of the articles, letters and editorials were identical to those written today on the topic: “It’s time for the paternalism of the relationship between doctors and patients to be transformed into a partnership;” “There are benefits to this change and dangers to maintaining the status quo;” “Some doctors and patients resist the change and some embrace it: Why?”
Two questions struck me as I impatiently scanned the articles from 12 years ago: First, why are these articles about doctor-patient partnership still so relevant? And second, why did the editor choose this cover image?
I’ve been mulling over these questions for a couple days, and I think an answer to the second question sheds light on the first. Here are some thoughts about the relationship between patients and doctors (and nurse practitioners and other clinicians) evoked by that image of the two elegant people dancing together:
It takes two to tango. Ever seen one guy doing the tango? Nope. Whatever he’s doing out there on the dance floor, that’s not tango. Without both dancers, there is no tango. The reason my doctor and I come together is our shared purpose of curing my illness or easing my pain. We bring different skills, perspectives and needs to this interaction. When in a partnership, I describe my symptoms and recount my history. I talk about my values and priorities. I say what I am able and willing to do for myself and what I am not. My doctor has knowledge about my disease and experience treating it in people like me; she explains risks and tradeoffs of different approaches and tailors her use of drugs, devices, and procedures to meet my needs and my preferences. Both of us recognize that without the active commitment of the other we can’t reach our shared goal: To help me live as well as I can for as long as I can.
Each dancer adjusts to his or her partner. In tango, each partner has different moves; the lead shifts subtly and constantly between them throughout the dance. In a partnership, when I am really ill, I delegate more decisions to my physicians; when I am well we freely go back and forth, discussing treatment options and making plans. Read more »
*This blog post was originally published at CFAH PPF Blog*
January 6th, 2011 by admin in Research, True Stories
No Comments »

This is a guest post from Dr. Jessie Gruman.
**********
More Can Also Be Less: We Need A More Complete Public Discussion About Comparative Effectiveness Research
When the public turns its attention to medical effectiveness research, a discussion often follows about how this research might restrict access to new medical innovations. But this focus obscures the vital role that effectiveness research will play in evaluating current medical and surgical care.
I am now slogging through chemotherapy for stomach cancer, probably the result of high doses of radiation for Hodgkin lymphoma in the early 1970s, which was the standard treatment until long-term side effects (heart problems, additional cancers) emerged in the late 80s. So I am especially attuned to the need for research that tracks the short and long-term effectiveness — and dangers — of treatments.
Choosing a surgeon this September to remove my tumor shone a bright light for me on the need for research that evaluates current practices. Two of the three surgeons I consulted wanted to follow “standard treatment procedures” and leave a six-centimeter, cancer-free margin around my tumor. This would mean taking my whole stomach out, because of its anatomy and arterial supply.
The third surgeon began our consultation by stating that her aim would be to preserve as much of my stomach as possible because of the difference in quality of life between having even part of one’s stomach versus none. If at all possible, she wanted to spare me life without a stomach.
But what about the six-centimeter margin? “There isn’t really much evidence to support that standard,” she said. “This issue came up and was discussed at a national guidelines meeting earlier in the week. No one seemed to know where it came from. We have a gastric cancer registry at this hospital going back to the mid 1990s and we haven’t seen support for it there, either. A smaller margin is not associated with an increased risk of recurrence.” Read more »
 Trudy Lieberman is concerned that despite all the rhetoric, choosing the best hospital, the best doctor, the best health plan, is simply not possible. Some of the so-called best might be good for some people but not others, and the information available to inform/guide choices is just too ambiguous.
Trudy Lieberman is concerned that despite all the rhetoric, choosing the best hospital, the best doctor, the best health plan, is simply not possible. Some of the so-called best might be good for some people but not others, and the information available to inform/guide choices is just too ambiguous.![]()