April 25th, 2011 by DrWes in Health Policy, Opinion
No Comments »
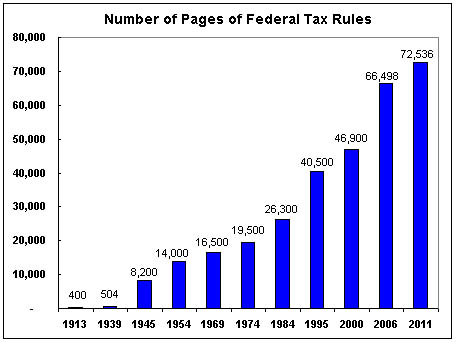
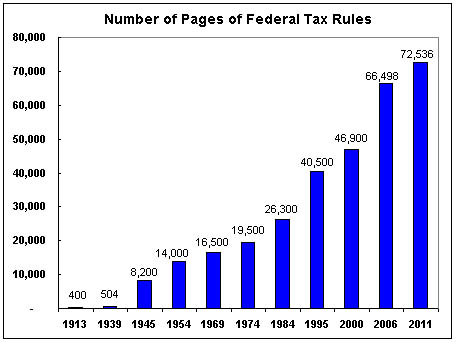
The above graph from the Cato Institute demonstrates the growing complexity of the U.S. tax code over the years. After doing my taxes recently and trying to track the ins and outs of the law for my wife’s private practice, I can attest to the graph’s accuracy.
But then I was reading an interesting editorial in Circulation: Arrhythmia and Electrophysiology by N.A. Mark Estes III, MD and Jonathan Weinstock, MD that reviewed an article by Roos, et al in the same journal that found only 27 of 698 guideline recommendations from the European Society of Cardiology (median 1.2% per guideline [IQR 0.95% to 3.7%]) were correctly referenced as Class I or III Level of Evidence A recommendations, calling into question the accuracy of guideline recommendations. In their editorial, Estes and Weinstock defended the guideline process but also mentioned the following shocking statistic: Read more »
*This blog post was originally published at Dr. Wes*
January 25th, 2011 by DrRich in Health Policy, Opinion
1 Comment »

While DrRich is a conservative American, and has made plain the difficulties he has with the Progressive program in general and with Progressive healthcare reform in particular, at times he is forced to admit that, on occasion, the Progressive way of looking at the world has certain merits. And as DrRich contemplates a question that has been bothering him lately, a question that no doubt plagues many American physicians who (unlike DrRich) are still toiling away in the trenches, he finds that this is one such occasion.
That question is: Just who are the people writing all those clinical guidelines — the “guidelines” physicians are now expected to follow in every particular in every case, on pain of massive fines, loss of career, and/or incarceration?
DrRich is quick to say that the act of creating clinical guidelines is not inherently evil, and indeed, back in the day when guidelines were merely guidelines (instead of edicts or directives that must be obeyed to the last letter), creating clinical guidelines was a rather noble thing to do.
But today, we have physicians clamoring to become GOD (Government Operatives Deliberating) panelists. These aristocrats of medicine will render the rules by which their more inferior fellow physicians, the ones who have actual contact with patients, will live or die. Clearly positions of such authority will be very desirable, and so, as one might predict, they are being vigorously pursued. And we are seeing candidates audition for these panels with efforts ranging from amateurish to ruthless. It puts one in mind of the early-season contestants on “American Idol.” Read more »
*This blog post was originally published at The Covert Rationing Blog*
November 9th, 2010 by GarySchwitzer in Better Health Network, Health Policy, News, Opinion
No Comments »

Take medical uncertainty. Add financial incentive to treat. Voila! Increased utilization. Now take away financial incentive to treat. Guess what you get?
MedPageToday explains, in the case of hormone therapy for prostate cancer:
Medicare accomplished what clinical guidelines and evidence-based medicine couldn’t: it reduced unnecessary use of androgen deprivation therapy (ADT) in prostate cancer.
Inappropriate use decreased by almost 30% from 2003 to 2005, following enactment of the Medicare Modernization Act, which lowered physician reimbursement for ADT. Appropriate use of ADT did not change during the same time period, according to an article in the Nov. 4 issue of the New England Journal of Medicine.
“Our findings suggest that reductions in reimbursement may influence the delivery of care in a potentially beneficial way, with even the modest [reimbursement] changes in 2004 associated with a substantial decrease in the use of inappropriate therapy,” Vahakn B. Shahinian, MD, of the University of Michigan in Ann Arbor, and co-authors wrote in conclusion.
“The corollary is that reimbursement policies should be carefully considered to avoid providing incentives for care for which no clear benefit has been established. The extreme profitability of the use of gonadotropin-releasing hormone (GnRH) agonists during the 1990s probably contributed to the rapid growth in the use of ADT for indications that were not evidence-based.”
*This blog post was originally published at Gary Schwitzer's HealthNewsReview Blog*
June 14th, 2010 by StevenWilkinsMPH in Better Health Network, Health Policy, News, Opinion, Research
1 Comment »

In a recent article, the editors of the Archives of Internal Medicine make the case that too much unneeded care is being delivered in physician’s offices these days. According to the authors, “patient expectations” are a leading cause of this costly problem.
Their solution? Get physicians to share with patients the “evidence” for why their requests are crazy, wrong, ill-informed or just plain stupid. But getting patients to buy into the “less is more” argument is a daunting task as most physicians already know. The problem is complicated by the fact that patients have a lot good reasons for not buying it. Read more »
*This blog post was originally published at Mind The Gap*
June 14th, 2010 by KevinMD in Better Health Network, Health Policy, Health Tips, News, Opinion
No Comments »

Just when I’ve lost hope that mainstream media will stop perpetuating the myth the more medicine equals better care, the Associated Press came up with this excellent piece. The article states, rightly, that “anywhere from one-fifth to nearly one-third of the tests and treatments we get are estimated to be unnecessary,” and that, “it may lead to dangerous side effects.”
Regular readers of this blog should be familiar with those concepts. I wrote recently that patients often reject evidence-based medicine. One reason is that there aren’t enough clinical guidelines available for patients to make an informed decision. Read more »
*This blog post was originally published at KevinMD.com*