March 10th, 2015 by Dr. Val Jones in Health Policy, Opinion
No Comments »
 The digital revolution in healthcare has transformed most hospitals into EMR-dependent worksites, dotted with computer terminals that receive more attention than the patients themselves. I admit that my own yearning for the “good old days” was beginning to wane, as my memory of paper charting and a patient-focused culture was becoming a distant memory. That is, until I filled in for a physician at a rural hospital where digital mandates, like a bad zombie movie, had bitten their victim but his full conversion to undead status had not been completed. At this hospital in its “incubation period,” electronic records consisted of collated scans of hand-written notes, rather than auto-populated templates. I’m not necessarily recommending the return of the microfiche, but what I experienced in this environment surprised me.
The digital revolution in healthcare has transformed most hospitals into EMR-dependent worksites, dotted with computer terminals that receive more attention than the patients themselves. I admit that my own yearning for the “good old days” was beginning to wane, as my memory of paper charting and a patient-focused culture was becoming a distant memory. That is, until I filled in for a physician at a rural hospital where digital mandates, like a bad zombie movie, had bitten their victim but his full conversion to undead status had not been completed. At this hospital in its “incubation period,” electronic records consisted of collated scans of hand-written notes, rather than auto-populated templates. I’m not necessarily recommending the return of the microfiche, but what I experienced in this environment surprised me.
1. Everyone read my notes. Because everything I wrote was relevant (not just a re-hash of data from another part of the medical record), reading became high-yield. Just as people have adapted to ignoring internet advertising (Does anyone even look at the right hand rails of web pages anymore?), EMR-users have become accustomed to skimming and ignoring notes because the “nuggets” of useful input are so sparse and difficult to find that no has time to do so. The entire team was more informed and up to date with my treatment plan because they could easily read what I was thinking.
2. I was able to draw diagrams again. Sometimes a picture is worth 1000 words – and when given a pen and paper, it is great to have the chance to quickly draw a wound site, or visually capture the anatomical concerns a patient may have, or even add an arrow, underline, or circle for emphasis. Thorough neuro exams are so much easier to document with stick figures and motor scores/reflexes added.
3. I could see at a glance if a consultant had stopped by to see a patient. It used to be customary for specialists to leave a note in the paper record immediately after examining a patient. If they didn’t have time to jot down a full consult, they would at least leave me their summary statement – with critical conclusions and next steps. It was a real time-saver to know when a consulting physician had evaluated a patient and get their key feedback if you missed them in person.
Nowadays consultants often see patients and order tests and medications in the EMR without speaking to the requesting attending physician. It may take days for their notes or dictation to show up in the electronic medical record, and depending on the complexity of the system, they may be nearly impossible to find. The result is redundant phone calling (asking the consultant’s admin, NP, PA etc. if they know if he’s seen the patient and what the plan is), and sometimes missed steps in the timely ordering of tests and procedures. At times I simply resort to asking the patient if Dr. So-And-So has stopped by, and if they know what he was planning to do. This doesn’t inspire confidence on the patient’s part, I can tell you.
4. I could order anything I wanted. EMR order entry systems force you to select from drop down menus that may not reflect your intentions. When you have a pen and paper – imagine this – you can very clearly and accurately capture what you’d like to order for the patient! There is no confusion about drug taper schedules, wound care instructions, weight bearing status, exercise precautions. It’s all as clear as free text. You can even explain why substitutes are not acceptable, thus heading off a follow up pharmacist call.
5. The patient became the focus. Since I didn’t need to spend all my time entering data into a computer system in real time, I was able to focus more carefully and clearly on the patients. My attention was not constantly being distracted by EMR alerts, unimportant drug interaction warnings, or forced entry of irrelevant information in order to complete a task. I felt more relaxed, I had more time to think, and I got more important work done.
In conclusion, it is obvious to me that we have a long way to go in making EMRs fit our natural pre-zombification hospital workflow. At the very least, we should be developing the following tools:
1. We need better ways to separate the signal from the noise. Even something as simple as a different font color for the new information that we doctors enter (in a given progress note) would help the eye latch on to what’s important. There should be a simple, visual way to distinguish between template and free text.
2. We need a pen feature that allows authors to signify emphasis. Wouldn’t it be nice if there could be an overlay that allowed us to circle words or add arrows or underlines? If the TV weather man can do this on his digital map, why can’t EMRs allow this layer? For example, physicians would like to circle lab values that are changing, and indicate the direction of change.
3. We need boxes where we can draw diagrams. A simple tablet function would be easy enough to enable. Sure it would be nice to have a stylus, but I’d settle for mouse or track pad entry. This is not a feature of most EMRs I’ve used, but could easily become one. Perhaps not everyone will want to use this feature, but for the artistic among us, it would be a god-send.
4. We need a Four-Square check in type feature so that physicians immediately know if their patient has been seen by the requested consultants. Their impressions should be quickly accessible (perhaps with a voice text to the ordering MD) while their formal consultation notes are grinding their way through the system days later.
5. We need to pare down the unnecessary EMR alerts, and off load data entry required to meet billing requirements to non-clinical staff. Physicians need to focus on their patient care, not spin their wheels figuring out coding subtleties and CMS documentation requirements that could be completed by others.
6. We need more flexibility in data order entry – so that treatment intentions are captured, not forced into an ill-fitting box. Currently, physicians are finding ways to free text their orders in bizarre “work arounds” just to get them on the record somewhere. This is a recipe for disaster, as lost orders are fairly commonplace when staff aren’t on the same page regarding where to look for free text orders. I feel badly for the nurses, since “note to nurse” seems to be the favored way to enter a complicated pharmacy order.
I am grateful that I got one last look at hospital care as it used to be – so that I can put my finger on why our new digital system is not working well. I just hope that my suggestions help to make processes better for all of us medical zombies in the new digital world.
***
More advice for EMR Vendors here.
Pluses and minuses of EMRs.
April 22nd, 2014 by Dr. Val Jones in Health Policy, Humor, Opinion
1 Comment »
 In my last post I wrote about the communication difficulties caused by electronic medical records systems. The response on Twitter ranged from sentiments including everything from “right on, sister” to “greedy doctors are only complaining about EMRs because of their price tag.” The disconnect between policy wonk’s (and EMR vendor’s) belief in the transformative power of EMRs and exasperated clinician users of these products is jaw-dropping. Physicians are often labeled as obstinate dinosaurs, blocking progress, while policy wonks are considered by physicians to be living in an alternate reality where a mobile phone app could fix all that is wrong with the healthcare system.
In my last post I wrote about the communication difficulties caused by electronic medical records systems. The response on Twitter ranged from sentiments including everything from “right on, sister” to “greedy doctors are only complaining about EMRs because of their price tag.” The disconnect between policy wonk’s (and EMR vendor’s) belief in the transformative power of EMRs and exasperated clinician users of these products is jaw-dropping. Physicians are often labeled as obstinate dinosaurs, blocking progress, while policy wonks are considered by physicians to be living in an alternate reality where a mobile phone app could fix all that is wrong with the healthcare system.
Being on the dinosaur side, I thought I’d try a quick experiment/analogy to demonstrate that EMR dissatisfaction is not a mere cost artifact. To show what happens when a digital intermediary runs medical information through a translator, I selected a random paragraph about the epidemiology of aphasias from an article in Medscape. I copied and pasted it into Google translator and then ran it backwards and forwards a few times in different languages. In the end, the original paragraph (exhibit A) became the second paragraph (exhibit B):
Exhibit A:
“Not enough data are available to evaluate differences in the incidence and clinical features of aphasia in men and women. Some studies suggest a lower incidence of aphasia in women because they may have more bilaterality of language function. Differences may also exist in aphasia type, with more women than men developing Wernicke aphasia.”
Exhibit B:
“Prevalence and characteristics of men and women are expected to afasia is not enough information available. If afasia some studies, women work more, not less, because they show that the spoken language. There may be differences in the type of OST, women and men to develop more of a vernikke afasia, more.”
Although the B paragraph bears some resemblance to A, it is nearly impossible to determine its original meaning. This is similar to what happens to medical notes in most current EMRs (except the paragraph would be broken up with lab values and vital signs from the past week or two). If your job were to read hundreds of pages of B-type paragraphs all day, what do you think would happen? Would you enthusiastically adopt this new technology? Or would you give up reading the notes completely? Would you need to spend hours of your day finding “work-arounds” to correct the paragraphs?
And what would you say if the government mandated that you use this new technology or face decreased reimbursement for treating patients? What if you needed to demonstrate “meaningful use” or dependency and integration of the translator into your daily workflow in order to keep your business afloat? What if the scope of the technology were continually expanded to include more and more written information so that everything from lab orders to medication lists to hospital discharges, nursing summaries, and physical therapy notes, etc. were legally required to go through the translator first? And if you pointed out that this was not improving communication but rather introducing new errors, harming patients, and stealing countless hours from direct clinical care, you would be called “change resistant” or “lazy.”
And what if 68,000 new medical codes were added to the translator, so that you couldn’t advance from paragraph to paragraph without selecting the correct code for a disease (such as gout) without reviewing 150 sub-type versions of the code. And then what if you were denied payment for treating a patient with gout because you did not select the correct code within the 150 subtypes? And then multiply that problem by every condition of every patient you ever see.
Clearly, the cost of the EMR is the main reason why physicians are not willing to adopt them without complaint. Good riddance to the 50% of doctors who say they’re going to quit, retire, or reduce their work hours within the next three years. Without physicians to slow down the process of EMR adoption, we could really solve this healthcare crisis. Just add on a few mobile health apps and presto: we will finally have the quality, affordable, healthcare that Americans deserve.
April 21st, 2014 by Dr. Val Jones in Opinion, True Stories
2 Comments »
 For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
This week I’ve been considering how in-patient doctoring has changed since I was in medical school. Unfortunately, my experience is that most of the changes have been for the worse. While we may have a larger variety of treatment options and better diagnostic capabilities, it seems that we have pursued them at the expense of the fundamentals of good patient care. What use is a radio-isotope-tagged red blood cell nuclear scan if we forget to stop giving aspirin to someone with a gastrointestinal bleed?
At the risk of infecting my readers with a feeling of helplessness and depressed mood, I’d like to discuss my findings in a series of blog posts. Today’s post is about why electronic medical charts have become ground zero for deteriorating patient care.
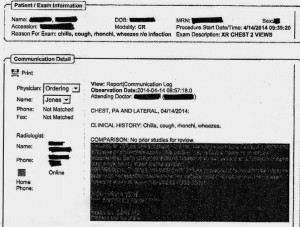
EMR Alert - Featuring radiologist note in illegible font color
1. Medical notes are no longer used for effective communication, but for billing purposes. When I look back at the months of training I received at my alma mater regarding the proper structure of intelligent medical notes, I recall with nostalgia how beautiful they were. Each note was designed to present all the observed and collected data in a cohesive and logical format, justifying the physician’s assessment and treatment plan. Our impressions of the patient’s physical and mental condition, reasons for further testing, and our current thought processes regarding optimal treatments and follow up (including citation of scientific literature to justify the chosen course) were all crisply presented.
Nowadays, medical notes consist of randomly pre-populated check box data lifted from multiple author sources and vomited into a nonsensical monstrosity of a run-on sentence. It’s almost impossible to figure out what the physician makes of the patient or what she is planning to do. Occasional “free text” boxes can provide clues, when the provider has bothered to clarify. One needs to be a medical detective to piece together an assessment and plan these days. It’s both embarrassing and tragic… if you believe that the purpose of medical notes is effective communication. If their purpose is justifying third-party payer requirements, then maybe they are working just fine?
My own notes have been co-opted by the EMRs, so that when I get the chance to free-text some sensible content, it still forces gobbledygook in between. I can see why many of my peers have eventually “given up” on charting properly. No one (except coders and payers interested in denying billing claims) reads the notes anymore. The vicious cycle of unintelligible presentation drives people away from reading notes, and then those who write notes don’t bother to make them intelligent anymore. There is a “learned helplessness” that takes over medical charting. All of this could (I suppose) be forgiven if physicians reverted back to verbal handoffs and updates to other staff/peers caring for patients to solve this grave communication gap. Unfortunately, creating gobbledygook takes so much time that there is less old fashioned verbal communication than ever.
2. No one talks to each other anymore. I’m not sure if this is because of a general cultural shift away from oral communication to text-based, digital intermediaries (think zombie-like teens texting one another incessantly) or if it’s related to sheer time constraints. However, I am continually astonished by the lack of face-to-face or verbal communication going on in hospitals these days. When I first observed this phenomenon, I attributed it to the facility where I was working. However, experience has shown that this is an endemic problem in the entire healthcare system.
When you are overworked, it’s natural to take the path of least resistance – checking boxes and ordering consults in the EMR is easier than picking up a phone and constructing a coherent patient presentation to provide context for the specialist who is about to weigh in on disease management. Nursing orders are easier to enter into a computer system than actually walking over and explaining to him/her what you intend for the patient and why.
But these shortcuts do not save time in the long run. When a consultant is unfamiliar with the partial workup you’ve already completed, he will start from the beginning, with duplicate testing and all its associated expenses, risks, and rabbit trails. When a nurse doesn’t know that you’ve just changed the patient to “NPO” status (or for what reason) she may give him/her scheduled medications before noticing the change. When you haven’t explained to the physical therapists why it could be dangerous to get a patient out of bed due to a suspected DVT, the patient could die of a sudden pulmonary embolism. Depending upon computer screen updates for rapid changes in patient care plans is risky business. EMRs are poor substitutes for face-to-face communication.
In one case I remember a radiology tech expressing amazement that I had bothered to type the reason for the x-ray in the order field. How can a radiologist be expected to rule out something effectively if he isn’t given the faintest hint about what he’s looking for? On another occasion I called to speak with the radiologist on a complicated case where the patient’s medical history provided him with a clue to look for something he hadn’t thought of – and his re-read of the CT scan led to the discovery and treatment of a life-threatening disease. Imagine that? An actual conversation saved a life.
3. It’s easy to be mindless with electronic orders. There’s something about the brain that can easily slip into “idle” mode when presented with pages of check boxes rather than a blank field requiring original input. I cannot count the number of times that I’ve received patients (from outside hospitals) with orders to continue medications that should have been stopped (or forgotten medications that were not on the list to be continued). In one case, for example, a patient with a very recent gastrointestinal bleed had aspirin listed in his current medication list. In another, the discharging physician forgot to list the antibiotic orders, and the patient had a partially-treated, life-threatening infection.
As I was copying the orders on these patients, I almost made the same mistakes. I was clicking through boxes in the pharmacy’s medication reconciliation records and accidentally approved continuation of aspirin (which I fortunately caught in time to cancel). It’s extremely unlikely that I would have hand-written an order for aspirin if I were handling the admission in the “old fashioned” paper-based manner. My brain had slipped into idle… my vigilance was compromised by the process.
In my view, the only communication problem that EMRs have solved is illegible handwriting. But trading poor handwriting for nonsensical digital vomit isn’t much of an advance. As far as streamlining orders and documentation is concerned, yes – ordering medications, tests, and procedures is much faster. But this speed doesn’t improve patient care any more than increasing the driving speed limit from 60 mph to 90 mph would reduce car accidents. Rapid ordering leads to more errors as physicians no longer need to think carefully about everything. EMRs have sped up processes that need to be slow, and slowed down processes that need to be fast. From a clinical utility perspective, they are doing more harm than good.
As far as coding and billing are concerned, I suppose they are revolutionary. If hospital care is about getting paid quickly and efficiently then perhaps we’re making great strides? But if we are expecting EMRs to facilitate care quality and communication, we’re in for a big disappointment. EMRs should have remained a back end billing tool, rather than the hub of all hospital activity. It’s like using Quicken as your life’s default browser. Over-reach of this particular technology is harming our patients, undermining communication, and eroding critical thinking skills. Call me Don Quixote – but I’m going to continue tilting at the hospital EMR* windmill (until they are right-sized) and engage in daily face-to-face meetings with my peers and hospital care team.
*Note: there is at least one excellent, private practice EMR (called MD-HQ). It is for use in the outpatient setting, and is designed for communication (not billing). It is being adopted by direct primary care practices and was created by physicians for supporting actual thinking and relevant information capture. I highly recommend it!
August 15th, 2013 by Dr. Val Jones in Health Policy, Opinion
No Comments »
 As I travel around the country, working in the trenches of various hospitals, I’ve been struck by the number of errors made by physicians and nurses whose administrative burden distracts them from patient care. The clinicians who make the errors are intelligent and competent – and they feel badly when an error is made. However, the volume of tasks required of them in a day (many of which are designed to fulfill an administrative “patient safety” or “quality enhancement” process) makes it impossible for them to complete any task in a comprehensive and thoughtful manner. In the end, administrators’ responses to increased error frequency is to increase error tracking and demand further documentation that leads to less time with patients and more errors overall. It’s a vicious cycle that people aren’t talking about enough.
As I travel around the country, working in the trenches of various hospitals, I’ve been struck by the number of errors made by physicians and nurses whose administrative burden distracts them from patient care. The clinicians who make the errors are intelligent and competent – and they feel badly when an error is made. However, the volume of tasks required of them in a day (many of which are designed to fulfill an administrative “patient safety” or “quality enhancement” process) makes it impossible for them to complete any task in a comprehensive and thoughtful manner. In the end, administrators’ responses to increased error frequency is to increase error tracking and demand further documentation that leads to less time with patients and more errors overall. It’s a vicious cycle that people aren’t talking about enough.
As I receive patient admissions from various referral hospitals, I rarely find a comprehensive discharge summary or full history and physical exam document that provides an accurate and complete account of the patient’s health status. Most of the documentation is poorly synthesized, scattered throughout reams of EMR-generated duplicative and irrelevant minutiae. Interpreting and sifting through this electronic data adds hours to my work day. Most physicians don’t bother to sift – which is why important information is missed in the mad dash to treat more patients per day than can be done safely and thoroughly.
I have personally witnessed many critical misdiagnoses caused by sloppy and rushed medical evaluations. I have had to transfer patients back to their originating surgical hospitals (at some of America’s top academic centers) for further work up and treatment, and have uncovered everything from cancer to brain disorders to medication errors for patients who had been evaluated and treated by many other specialists before me. No one seems to have the time to take a long hard look at these patients, and so they end up undergoing knee-jerk treatments for partially thought through diagnoses. The quality of medical care in which I’ve been engaged (over the past 20 years) has taken a dramatic turn for the worse because of volume overload (fueled by diminishing reimbursement) in the setting of excessive administrative and documentation requirements.
To use an analogy – The solution to the healthcare cost crisis is not to increase the speed of the assembly line belt when our physicians and nurses are already dropping items on the floor. First, stop asking them to step away from the belt to do other things. Second, put a cap on belt speed. Third, insure that you have sufficient staff to handle the volume of “product” on the belt, and support them with post-belt packaging and procedures that will prevent back up.
What we require most in healthcare is time to process our thoughts and engage in information synthesis. We must give physicians the time they need to complete a full, comprehensive, evaluation of each patient at regular intervals. We need nurses to be freed from desk clerk and safety documentation activities to actually inspect and manage their patients and alert physicians to new information.
Until hospitals and administrators recognize that more data does not result in better care, and that intelligent information synthesis (which requires clinician time, not computer algorithms) is the foundation of error prevention, I do not foresee a bright future for patients in this manic assembly line of a healthcare system.
November 24th, 2011 by DavidHarlow in Health Policy, News
1 Comment »

The Wall of Shame welcomes Sutter Health. Another computer with unencrypted protected health information on over 4 million patients – gone. Now, those guys are pretty smart, so why don’t they encrypt all computers with PHI? One of life’s persistent questions. I mean, I can accept the fact that a health plan operator like Cignet Health might have issues with getting a grip on HIPAA compliance, but Sutter Health? What were they thinking? Can’t happen here? Encryption is a drag? It’s an easy way to avoid major egg-on-face and to avoid spending significant coin on PR, credit reporting services, and potentially on court judgments — all in addition to significant administrative fines payable to HHS and state regulators.
So the federales are piloting the HIPAA audit program. I know it’s required by the HITECH Act, but who believes that it will motivate behavior change? Anyone? Sutter Health was clearly not motivated to seek a safe harbor that would have made the loss of 4 million patient records a non-event. I know encryption can be a drag, but I’m not a techie. If you are, I invite you to educate me (and the other non-techies out there) on the question of how miserable it really is to have to deal with encrypted data; if you’re really a techie, write a program to enable light-touch encryption that doesn’t interfere with use of data.
Whether or not encryption is miserable, we should be asking: Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
 The digital revolution in healthcare has transformed most hospitals into EMR-dependent worksites, dotted with computer terminals that receive more attention than the patients themselves. I admit that my own yearning for the “good old days” was beginning to wane, as my memory of paper charting and a patient-focused culture was becoming a distant memory. That is, until I filled in for a physician at a rural hospital where digital mandates, like a bad zombie movie, had bitten their victim but his full conversion to undead status had not been completed. At this hospital in its “incubation period,” electronic records consisted of collated scans of hand-written notes, rather than auto-populated templates. I’m not necessarily recommending the return of the microfiche, but what I experienced in this environment surprised me.
The digital revolution in healthcare has transformed most hospitals into EMR-dependent worksites, dotted with computer terminals that receive more attention than the patients themselves. I admit that my own yearning for the “good old days” was beginning to wane, as my memory of paper charting and a patient-focused culture was becoming a distant memory. That is, until I filled in for a physician at a rural hospital where digital mandates, like a bad zombie movie, had bitten their victim but his full conversion to undead status had not been completed. At this hospital in its “incubation period,” electronic records consisted of collated scans of hand-written notes, rather than auto-populated templates. I’m not necessarily recommending the return of the microfiche, but what I experienced in this environment surprised me.

 In
In  For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “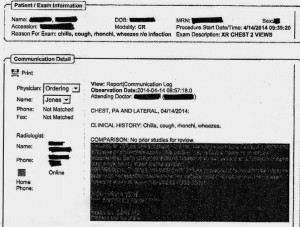
 As I
As I








