March 11th, 2011 by DavedeBronkart in Research, True Stories
No Comments »

 [Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.
[Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.
It’s a good combination: Pat speaks from the heart about her own experience and her passion for community, and Susannah, as usual, speaks as an “internet geologist” — as she once put it, “A geologist doesn’t have opinions about the rocks, she just observes and describes them.” Susannah spoke about her newly-released report “Peer-To-Peer Healthcare,” about which she recently wrote here.
Listener comments begin around 13:00. Examples:
— A woman describes how she started a Facebook group for her painful chronic condition (ankylosing spondylitis) and it’s grown into a website, HurtingButHelpful.org. (Spoonies, take note!) What drove her to create a patient community? “There’s no one else who can understand what I’m talking about.”
— The mother of a newborn with a heart defect found similar parents online. Hearing their stories — and even seeing an upsetting photo — helped her prepare for the surgery.
— On the downside, the daughter of an ovarian cancer patient said her now-cured mom keeps going online to patient communities and getting scared by what she reads. (Host Neal Conan’s observation: “There other parts of the computer that can be addictive, and I guess this one can, too.”)
It’s heartening to hear coverage of online patient communities, including the risks and challenges, in a respected outlet like NPR. (Time covered it, too, a year ago.) And there’s no equal for the reality check of Pew’s data. Some patient activists suggest (and some people fear) that the Internet “frees” patients from doctors, but Pew says that’s not what people are doing. Read more »
*This blog post was originally published at e-Patients.net*
March 1st, 2011 by DavedeBronkart in Health Policy, Opinion
No Comments »

ABCNews.com has posted a great new piece by Dr. Roni Zeiger entitled, “The Biggest Wasted Resource in Health Care? You.” Subtitle: “How Your Internet Research Can Help Your Relationship With Your Doctor.” It’s well reasoned and clearly written, and continues the trend we cited a month ago, when Time posted Dr. Zack Meisel’s article saying that patients who Google can help doctors.
Related notes:
— Dr. Zeiger’s article title parallels what Dr. Charles Safran told the House Ways & Means Subcommittee on Health in 2004: Patients are “the most under-utilitized resource.” He was talking about health IT, quoting his colleague Dr. Warner Slack, who had said it many years earlier. I often quote it in my speeches for the Society for Participatory Medicine, asserting that it applies not just to IT but to all of healthcare.
— Dr. Zeiger is on the editorial board of our Journal of Participatory Medicine and is Chief Health Strategist at Google. He gets the power of patient engagement deeply and clearly. Last fall he posted a prediction that in the future it might be malpractice for doctors not to prescribe a patient community to help you help yourself with your conditions.
Prediction: Googling and patient networks will become essential as we move toward the practice of shared medical decision making (SMDM). I know firsthand that the information my kidney cancer community gave me about coping with treatments went well beyond what my excellent clinicians could offer. (We’re starting a series on SMDM. The first entry was in December.)
*This blog post was originally published at e-Patients.net*
February 1st, 2011 by DavedeBronkart in Better Health Network, Opinion
No Comments »

I have a Google alert for “e-patient,” and sometimes I’m surprised what it catches. [Recently] it was this:
3 Reasons Steve Jobs Will Be The Ultimate e-Patient
Steve Jobs’ medical leave sets the stage for the upcoming revolution in the production and delivery of medical information at time of diagnosis. 3 things you need to know.
So I’m thinking: “Oh, wow: Is the term ‘e-patient’ going mainstream?” That would be a hoot, because indeed the Society for Participatory Medicine is engaged in spreading the word.
*This blog post was originally published at e-Patients.net*
January 21st, 2011 by DavedeBronkart in Health Tips, Opinion
No Comments »

There are several stages in becoming an empowered, engaged, activated patient — a capable, responsible partner in getting good care for yourself, your family, whoever you’re caring for. One ingredient is to know what to expect, so you can tell when things seem right and when they don’t.
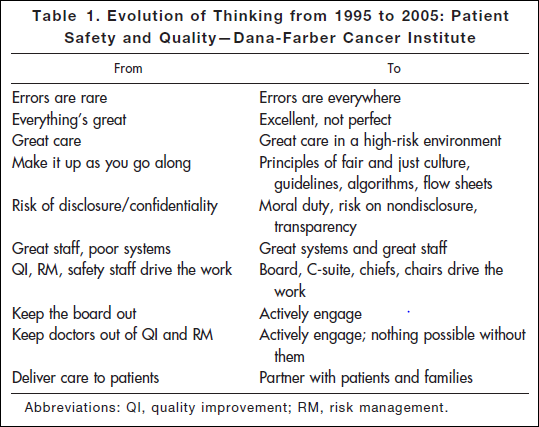
Researching a project today, I came across an article* published in 2006: “Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey.” This table shows the attitude you’ll find in an organization that has realized the challenges of medicine and is dealing with them realistically:
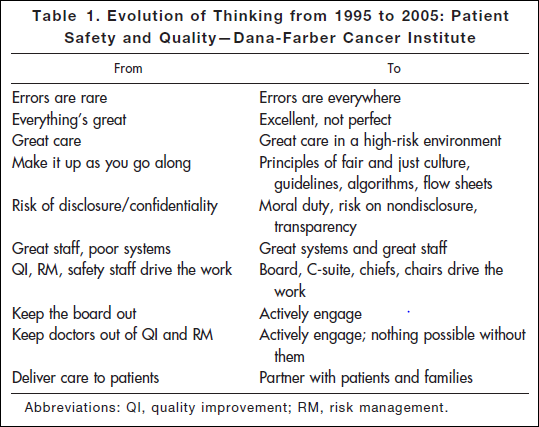
“Errors are everywhere.” “Great care in a high-risk environment.” What kind of attitude is that? It’s accurate.
This work began after the death of Boston Globe health columnist Betsy Lehman. Long-time Bostonians will recall that she was killed in 1994 by an accidental overdose of chemo at Dana-Farber. It shocked us to realize that a savvy patient like her, in one of the best places in the world, could be killed by such an accident. But she was.
Five years later the Institute of Medicine’s report “To Err is Human” documented that such errors are in fact common — 44,000 to 98,000 a year. It hasn’t gotten better: Last November the U.S. Inspector General released new findings that 15,000 Medicare patients are killed in U.S. hospitals every month. That’s one every three minutes. Read more »
*This blog post was originally published at e-Patients.net*
January 16th, 2011 by DavedeBronkart in Health Policy, Opinion
No Comments »

From the Medscape Medical Ethics article entitled “‘Some Worms Are Best Left In The Can’: Should You Hide Medical Errors?“:
Consequences aside, from a strictly ethical perspective, if a patient doesn’t realize that his physician made a mistake, should the physician fess up?
Before you jump to conclusions (as I did), look at the article’s three parts. It’s about a survey. The title is on the inflammatory side; the article is a window into physicians’ views. The introduction continues:
Evidence of the complex prisms through which physicians view these issues was apparent in the replies to four questions asked in Medscape’s exclusive ethics survey. More than 10,000 physicians responded to the survey in 2010.
Subheads:
— Mistakes that don’t harm patients. “Are there times when it’s acceptable to cover up or avoid revealing a mistake if that mistake would not cause harm to the patient?” Sixty percent said “no;” the others split between “yes” and “it depends.”
- I personally can understand this note from a survey respondent: “If there is a mistake that would have no medical effect but would cause extreme, uncalled-for anxiety, then yes,” especially since I know people (some elders, some young) who would indeed freak out, out of proportion. But, that’s a big judgment call.
- I have a harder time accepting this comment: “Why shake the patient’s trust in the doctor for something that is irrelevant?” Irrelevant is a big judgment call, and I’d be really concerned about the natural human tendency to minimize the probable impact of a mistake — especially if a provider thinks it’s all about maintaining a patient’s trust, even when the topic is their own error.
— Mistakes that might harm patients. Ninety five percent said “no;” some still said “yes!” One commented: “If the mistake has not progressed to harmfulness, then it’s essentially a non-issue. Treatment correction takes place and you move on.” Another says if there hasn’t been harm yet, “I think a ‘wait and see’ approach is okay.” Read more »
*This blog post was originally published at e-Patients.net*
![]() [Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.
[Recently] NPR’s popular program “Talk of the Nation” covered something we discuss often: How e-patients find information and find each other online. Featured guests were Pat Furlong, mother of two boys with a rare disease who started an online community, and Susannah Fox of the Pew Internet and American Life Project, a frequent contributor here. The audio is here.