October 10th, 2009 by Happy Hospitalist in Better Health Network, Opinion
2 Comments »

Here’s an interesting case. A young woman drinks antifreeze to commit suicide, writes a note saying she does not want any medical treatment and calls an ambulance so she can die peacefully with the help of medical support.
I read a lot on Happy Hospitalist about a patient’s right to demand what ever care they feel is necessary to keep them alive and the duty of the physician to provide whatever care the patient feels they require, no matter how costly or how miniscule the benefit. Readers like to say it’s not a physician’s obligation to make quality of life decisions for the patient.
So let’s analyze this situation. Does a patient have the right to demand medical care and the services of physicians to let them die without pain? Does a patient have the right to demand a physician order morphine and ativan to keep a depressed but physically intact patient comfortable as they slip away in a horrible antifreeze death under the care of medical personel? Read more »
*This blog post was originally published at A Happy Hospitalist*
October 4th, 2009 by DrWes in Better Health Network, True Stories
No Comments »

It was midnight and the Emergency Room door opened like a curtain on a Broadway. A lone man sat in blue at the countertop, writing. Behind him, the chorus, working feverishly on the protagonist – the script rehearsed a thousand times before.
Clothes off, Story?, facemask, C-collar, endotracheal tube, breath sounds, telemetry, IV’s, blood work, pulse ox, Stop.
Resume, Pulse?, patches, register, call the lab, Allergies?, epi, atropine, Pressure?, twitching, NG, x-ray, Stop. Pulse?
Resume, pacing wire, max output, capture?, not quite, “potassium?”, not ready, blood gas, foley, Capture! Stop.
Resume, blood gas, no capture, damn, tweak, better, pulse?, yes. Lab?, no, Which meds?, cardiologist, Go.
Vent, hoist, prep, stick, contrast, open, shock, balloon pump, a-line, movement, labs, blood gas, peep, transport, c-spine, CT, Go.
Then intermission. Read more »
*This blog post was originally published at Dr. Wes*
September 22nd, 2009 by EvanFalchukJD in Better Health Network, Health Tips, Opinion
No Comments »

There’s a case for killing Granny? I guess so, or at least according to Evan Thomas’ article in the most recent
Newsweek. Thomas, after sharing the story of his mother’s last days, concludes that
death is the key to health care reform:
Until Americans learn to contemplate death as more than a scientific challenge to be overcome, our health care system will remain unfixable.
Does everything need to have a political spin on it nowadays?
But let’s take Thomas’ advice and talk about death. Not “death panels,” not the politics or the cost of end-of-life care. Just plain old death.
I was reminded recently of how fragile life is. It made me remember something I read after our oldest child was born. I realized that one day she would learn the truth about death. And I thought how bad that was, and how I wanted to protect her from it. But then, by chance, I happened across this interesting little saying.
When your children are young, all you think about is that you don’t want them to die. But when they get older, all they think about is that they don’t want you to die.
It touched me, and it made me think about how my responsibility to protect my children extended even unto and beyond my own death.
It’s a nice philosophical point, but there are very practical things each of us can do to fulfill this responsibility. Here is my list of just a few of the very important things we all should do to plan for our deaths:
Buy life insurance
If you’re young and in reasonably good health you should be able to buy a term life insurance policy for a few hundred dollars a year. You should do this so your family can have your earning potential replaced in the event of your death. Find a good insurance broker and make sure you get coverage that suits your needs. Even if you have a pre-existing condition (like a chronic illness) a good broker should be able to find you some kind of coverage. You won’t be able to buy any coverage at all if you become acutely ill, so don’t wait until it’s too late.
Make a will
This is so much more than just planning for your family’s financial future. For example, if you have children, have you figured out who will take care of them if both you and your spouse die? There are many important and potentially difficult conversations that go along with this kind of planning – but you’re much better off having them now. After you die, those left behind will end up fighting out these issues not knowing your wishes. Find a good lawyer to help you.
Make an advance directive
You need to think about what kind of medical care you want if you become incapacitated and unable to decide on your own. Do you want to live for 30 years on a ventilator, unconscious? Do you want to undergo extensive and painful treatments if you don’t have much hope of a meaningful recovery? Don’t leave your family alone trying to make that decision for you, wondering what you would have wanted. Write down what your wishes are.
Appoint a health care proxy
Pick someone who you trust to make your medical decisions for you if you are unable to do so. Write it down and make clear what you want that person to do, so if the time comes there isn’t any dispute among your family as to who is in charge.
There are many other things you can do, but to me these are four of what I think are the most important things you can do to prepare for your death. Maybe some commenters can add some more that I missed.
Now, with all that said and done, I will still disappoint Mr. Thomas.
Why? Because I still prefer to think of death as a scientific challenge to be overcome. And you know, I’m glad that many other people feel that way, too.
Especially the people who make medical breakthroughs – I’m really glad they feel that way.

*This blog post was originally published at See First Blog*
September 14th, 2009 by Dr. Val Jones in Announcements, Better Health Network, Expert Interviews, Health Policy, News, True Stories, Uncategorized
No Comments »
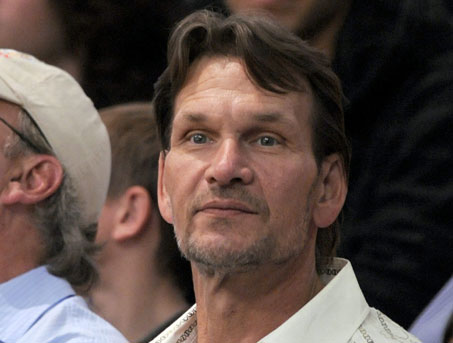
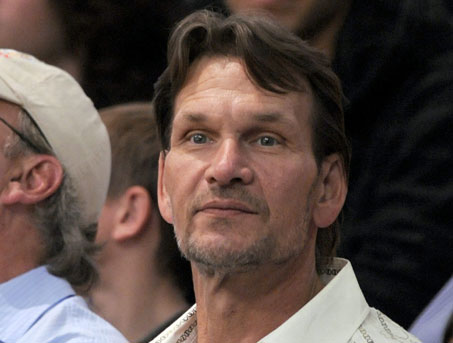 Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Patrick Swayze, the popular actor perhaps known best for his role in the 1987 hit movie “Dirty Dancing,” died today of pancreatic cancer. My thoughts are with his family in this time of grief.
Pancreatic cancer is among the more deadly forms of cancer. I asked GI oncologist, Heinz-Josef Lenz, M.D., professor of medicine and professor of preventive medicine in the Division of Medical Oncology at the Keck School of Medicine at the University of Southern California, to explain why that’s so.
Dr. Val: Why is pancreatic cancer so much more deadly (i.e. less treatable) than many other forms of cancer?
Dr. Lenz: Unfortunately we don’t have very effective drugs for pancreatic cancer, which makes it one of the deadliest cancers of all. The median survival is about 8 months with metastatic disease. Even when the tumor is successfully removed there is a very high risk for tumor recurrence. We need more funding to better understand the risk for pancreatic cancer and identify and develop more effective therapies.
Dr. Val: Can you describe the typical course of metastatic pancreatic cancer?
Dr. Lenz: Unfortunately, the 5 year survival rate for pancreatic cancer is only 15 to 20%. The average survival after diagnosis is 12 to 19 months. The best predictor of long term survival is if the tumor is found and removed before it reaches 3 cm in size. Patients with metastatic pancreatic cancer are usually treated with a combination chemotherapy consisting of gemcitabine, tarceva, xeloda or oxaliplatin. However the response rates are (despite using aggressive combination therapies) low. Large clinical trials recently did not show any benefit from erbitux or avastin, again demonstrating that pancreatic cancer therapy is a difficult clinical challenge.
Dr. Val: Are certain populations at higher risk than others for pancreatic cancer?
Dr. Lenz: Age is the most important risk factor for this cancer. It is most common in individuals over age 50 and increases in frequency with age. Black men and women are slightly more likely to get pancreatic cancer (though the reasons for this are unclear), and men are slightly more likely than women to get the cancer. Other risk factors are smoking, diabetes, and obesity.
Dr. Val: If you suspect that someone is “high risk” for pancreatic cancer, what tests should he/she have?
Dr. Lenz: Patients with a genetic predisposition for breast cancer known as BRCA are also at higher risk for pancreatic cancer. There is also a familial form of pancreatic cancer. These high risk families are being followed up with specific screening plans. However there is not a reliable test for pancreatic cancer. Imaging with CT or MRI can miss pancreatic cancer and there is no reliable blood marker. The most common used is CA 19-9, which can be used for monitoring and diagnosis but is not elevated in all patients.
Dr. Val: What if the cancer is caught very early? Does that increase likelihood of survival?
Dr. Lenz: Absolutely. The best chance of survival is when the cancer is limited to the pancreas, and is surgically removed before it reaches a size of 3 centimeters. There are certainly people who have been cured this way, but unfortunately it’s very rare to catch the cancer at such an early stage since it usually has no symptoms until it’s quite advanced.
***
There is a wonderful advocacy group for those whose lives are touched by pancreatic cancer: PanCAN. One of PanCAN’s founders, Paula Kim, is a friend of mine and was inspired to create the organization after her dad was diagnosed with pancreatic cancer in 1999. At that time there was very little advocacy for this deadly disease. PanCAN helps people with pancreatic cancer find help and support.
September 5th, 2009 by David Kroll, Ph.D. in News
No Comments »

 The Boulder County coroner announced today that the July death of a Boulder teen was indeed due to opioid intoxication from preparation of a poppy pod tea.
The Boulder County coroner announced today that the July death of a Boulder teen was indeed due to opioid intoxication from preparation of a poppy pod tea.
Jeffrey Joseph Bohan, 19, of Boulder, was found dead in his friend’s Boulder home about 6 p.m. July 21 after drinking poppy-pod tea the night before with his brother, according to Boulder police.
Investigators suspected the Fairview High graduate, who was going to Colorado State University, died from the psychoactive tea, which is brewed from the plant that produces opium. But they couldn’t be sure until the Coroner’s Office confirmed Monday that Bohan’s cause of death was morphine overdose, and his manner of death was accident.
Here is also coverage from The Boulder Daily Camera.
This marks the second death in Boulder from young adults mixing up decoctions of seeds or pods from the poppy, Papaver somniferum. We reported in March on the death of CU-Boulder student, Alex McGuiggan, in March.
In a subsequent post, we expanded on a commenter’s story of his own efforts to raise awareness of the dangers of poppy seed tea following the death of his own son. Commenter Tom’s site can be viewed at Poppy Seed Tea Can Kill You (http://poppyseedtea.com).
Extracts from poppy pods can contain up to 10% morphine and 1-5% codeine together with several other benzomorphan compounds. Seeds themselves are intrinsically devoid of morphine but the drug can remain on the seeds in reasonable quantities simply from their processing. The Santa Clara County crime laboratory investigating the death of Tom’s son determined that a tea made with the same seeds he used contained 259 µg/mL of morphine.
Depending on the starting material, however, the extract may also contain thebaine, a natural intermediate used for semi-synthetic opioid synthesis that causes intense nausea, vomiting, and even convulsions.
*This blog post was originally published at Terra Sigillata*