February 2nd, 2015 by Dr. Val Jones in Health Policy, Opinion
1 Comment »
 Electronic medical record systems (EMRs) have become a part of the work flow for more than half of all physicians in the U.S. and incentives are in place to bring that number up to 100% as soon as possible. Some hail this as a giant leap forward for healthcare, and in theory that is true. Unfortunately, EMRs have not yet achieved their potential in practice – as I have discussed in my recent blog posts about “how an EMR gave my patient syphillis,” in the provocative “EMRs are ground zero for the deterioration of patient care,” and in my explanation of how hospital pharmacists are often the last layer of protection against medical errors of EPIC proportions.
Electronic medical record systems (EMRs) have become a part of the work flow for more than half of all physicians in the U.S. and incentives are in place to bring that number up to 100% as soon as possible. Some hail this as a giant leap forward for healthcare, and in theory that is true. Unfortunately, EMRs have not yet achieved their potential in practice – as I have discussed in my recent blog posts about “how an EMR gave my patient syphillis,” in the provocative “EMRs are ground zero for the deterioration of patient care,” and in my explanation of how hospital pharmacists are often the last layer of protection against medical errors of EPIC proportions.
Considering that an EMR costs the average physician up to $70,000 to implement, and hospital systems in the hundreds of millions – it’s not surprising that the main “benefit” driving their adoption is improved coding and billing for reimbursement capture. The efficiencies associated with access to digital patient medical records for all Americans is tantalizing to government agencies and for-profit insurance companies managing the bill for most healthcare. But will this collective data improve patient care and save lives, or is it mostly a financial gambit for medical middle men? At this point, it seems to be the latter.
There are, however, some true benefits of EMRs that I have experienced – and to be fair, I wanted to provide a personal list of pros and cons for us to consider. Overall however, it seems to me that EMRs are contributing to a depersonalization of medicine – and I grieve for the lost hours genuine human interaction with my patients and peers. Though the costs of EMR implementation may be recouped with aggressive billing tactics, what we’re losing is harder to define. As the old saying goes, “What good is it for someone to gain the whole world, yet forfeit their soul?”
| Pros Of EMR |
Cons Of EMR |
| Solves illegible handwriting issue |
Obscures key information with redundancy |
| Speeds process of order entry and fulfillment |
Difficult to recall errors in time to stop/change |
| May reduce redundant testing as old results available |
Facilitates excessive testing due to ease of order entry |
| Allows cut and paste for rapid note writing |
Encourages plagiarism in lieu of critical thinking |
| Improves ease of coding and billing to increase reimbursement |
Allows easy upcoding and overcharging |
| Reminds physicians of evidence-based guidelines at point of care |
Takes focus from patient to computer |
| Improves data mining capabilities for research and quality improvement |
Facilitates data breaches and health information hacking |
| Has potential to improve information portability and inter-operability |
Has potential to leak personal healthcare information to employers and insurers |
| May reduce errors associated with human element |
May increase carry forward errors and computer-generated mistakes |
| Automated reminders keep documentation complete |
May increase “alert fatigue,” causing providers to ignore errors/drug interactions |
| Can be accessed from home |
Steep learning curve for optimal use |
| Can view radiologic studies and receive test results in one place |
Very expensive investment: staff training, tech support, ongoing software updates, etc. |
| More tests available at the click of a button |
Encourages reliance on tests rather than physical exam/history |
| Makes medicine data-centric |
Takes time away from face-to-face encounters |
| Improved coordination of care |
Decrease in verbal hand-offs, causing key information to be lost |
| Accessibility of health data to patients |
Potential for increased legal liability for physicians |
April 21st, 2014 by Dr. Val Jones in Opinion, True Stories
2 Comments »
 For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “locum tenens lifestyle” because I enjoy the challenge of working with diverse teams of peers and patient populations. I believe that this kind of work makes me a better doctor, as I am exposed to the widest possible array of technology, specialist experience, and diagnostic (and logistical) conundrums. During my down times I like to think about what I’ve learned so that I can try to make things better for my next group of patients.
This week I’ve been considering how in-patient doctoring has changed since I was in medical school. Unfortunately, my experience is that most of the changes have been for the worse. While we may have a larger variety of treatment options and better diagnostic capabilities, it seems that we have pursued them at the expense of the fundamentals of good patient care. What use is a radio-isotope-tagged red blood cell nuclear scan if we forget to stop giving aspirin to someone with a gastrointestinal bleed?
At the risk of infecting my readers with a feeling of helplessness and depressed mood, I’d like to discuss my findings in a series of blog posts. Today’s post is about why electronic medical charts have become ground zero for deteriorating patient care.
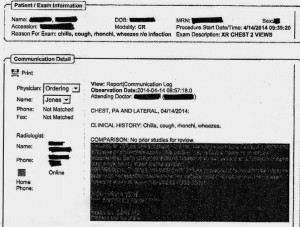
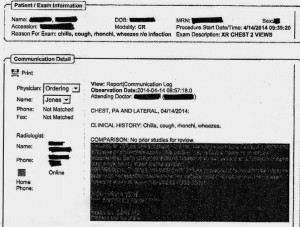
EMR Alert - Featuring radiologist note in illegible font color
1. Medical notes are no longer used for effective communication, but for billing purposes. When I look back at the months of training I received at my alma mater regarding the proper structure of intelligent medical notes, I recall with nostalgia how beautiful they were. Each note was designed to present all the observed and collected data in a cohesive and logical format, justifying the physician’s assessment and treatment plan. Our impressions of the patient’s physical and mental condition, reasons for further testing, and our current thought processes regarding optimal treatments and follow up (including citation of scientific literature to justify the chosen course) were all crisply presented.
Nowadays, medical notes consist of randomly pre-populated check box data lifted from multiple author sources and vomited into a nonsensical monstrosity of a run-on sentence. It’s almost impossible to figure out what the physician makes of the patient or what she is planning to do. Occasional “free text” boxes can provide clues, when the provider has bothered to clarify. One needs to be a medical detective to piece together an assessment and plan these days. It’s both embarrassing and tragic… if you believe that the purpose of medical notes is effective communication. If their purpose is justifying third-party payer requirements, then maybe they are working just fine?
My own notes have been co-opted by the EMRs, so that when I get the chance to free-text some sensible content, it still forces gobbledygook in between. I can see why many of my peers have eventually “given up” on charting properly. No one (except coders and payers interested in denying billing claims) reads the notes anymore. The vicious cycle of unintelligible presentation drives people away from reading notes, and then those who write notes don’t bother to make them intelligent anymore. There is a “learned helplessness” that takes over medical charting. All of this could (I suppose) be forgiven if physicians reverted back to verbal handoffs and updates to other staff/peers caring for patients to solve this grave communication gap. Unfortunately, creating gobbledygook takes so much time that there is less old fashioned verbal communication than ever.
2. No one talks to each other anymore. I’m not sure if this is because of a general cultural shift away from oral communication to text-based, digital intermediaries (think zombie-like teens texting one another incessantly) or if it’s related to sheer time constraints. However, I am continually astonished by the lack of face-to-face or verbal communication going on in hospitals these days. When I first observed this phenomenon, I attributed it to the facility where I was working. However, experience has shown that this is an endemic problem in the entire healthcare system.
When you are overworked, it’s natural to take the path of least resistance – checking boxes and ordering consults in the EMR is easier than picking up a phone and constructing a coherent patient presentation to provide context for the specialist who is about to weigh in on disease management. Nursing orders are easier to enter into a computer system than actually walking over and explaining to him/her what you intend for the patient and why.
But these shortcuts do not save time in the long run. When a consultant is unfamiliar with the partial workup you’ve already completed, he will start from the beginning, with duplicate testing and all its associated expenses, risks, and rabbit trails. When a nurse doesn’t know that you’ve just changed the patient to “NPO” status (or for what reason) she may give him/her scheduled medications before noticing the change. When you haven’t explained to the physical therapists why it could be dangerous to get a patient out of bed due to a suspected DVT, the patient could die of a sudden pulmonary embolism. Depending upon computer screen updates for rapid changes in patient care plans is risky business. EMRs are poor substitutes for face-to-face communication.
In one case I remember a radiology tech expressing amazement that I had bothered to type the reason for the x-ray in the order field. How can a radiologist be expected to rule out something effectively if he isn’t given the faintest hint about what he’s looking for? On another occasion I called to speak with the radiologist on a complicated case where the patient’s medical history provided him with a clue to look for something he hadn’t thought of – and his re-read of the CT scan led to the discovery and treatment of a life-threatening disease. Imagine that? An actual conversation saved a life.
3. It’s easy to be mindless with electronic orders. There’s something about the brain that can easily slip into “idle” mode when presented with pages of check boxes rather than a blank field requiring original input. I cannot count the number of times that I’ve received patients (from outside hospitals) with orders to continue medications that should have been stopped (or forgotten medications that were not on the list to be continued). In one case, for example, a patient with a very recent gastrointestinal bleed had aspirin listed in his current medication list. In another, the discharging physician forgot to list the antibiotic orders, and the patient had a partially-treated, life-threatening infection.
As I was copying the orders on these patients, I almost made the same mistakes. I was clicking through boxes in the pharmacy’s medication reconciliation records and accidentally approved continuation of aspirin (which I fortunately caught in time to cancel). It’s extremely unlikely that I would have hand-written an order for aspirin if I were handling the admission in the “old fashioned” paper-based manner. My brain had slipped into idle… my vigilance was compromised by the process.
In my view, the only communication problem that EMRs have solved is illegible handwriting. But trading poor handwriting for nonsensical digital vomit isn’t much of an advance. As far as streamlining orders and documentation is concerned, yes – ordering medications, tests, and procedures is much faster. But this speed doesn’t improve patient care any more than increasing the driving speed limit from 60 mph to 90 mph would reduce car accidents. Rapid ordering leads to more errors as physicians no longer need to think carefully about everything. EMRs have sped up processes that need to be slow, and slowed down processes that need to be fast. From a clinical utility perspective, they are doing more harm than good.
As far as coding and billing are concerned, I suppose they are revolutionary. If hospital care is about getting paid quickly and efficiently then perhaps we’re making great strides? But if we are expecting EMRs to facilitate care quality and communication, we’re in for a big disappointment. EMRs should have remained a back end billing tool, rather than the hub of all hospital activity. It’s like using Quicken as your life’s default browser. Over-reach of this particular technology is harming our patients, undermining communication, and eroding critical thinking skills. Call me Don Quixote – but I’m going to continue tilting at the hospital EMR* windmill (until they are right-sized) and engage in daily face-to-face meetings with my peers and hospital care team.
*Note: there is at least one excellent, private practice EMR (called MD-HQ). It is for use in the outpatient setting, and is designed for communication (not billing). It is being adopted by direct primary care practices and was created by physicians for supporting actual thinking and relevant information capture. I highly recommend it!
January 3rd, 2012 by Nicholas Genes, M.D., Ph.D. in Opinion
No Comments »

I’ve been using my iPad in the ED, with my white coat’s sewn-in iPad-sized pocket, for some time now — mostly for patient and resident education, and to look up dosages or rashes. Hitting up my Evernote database or Dropbox documents is also useful. Occasionally I’ll use my iPhone, for its LED light (when the otoscope can’t reach to where I need to see) or rarely, its camera (in compliance with my hospital and department photo policy, naturally).
Our ED’s EHR isn’t quite accessible enough via iPad for me to quickly check results or place orders at the bedside — right now it’s just too cumbersome. But there’s been progress — enough so that I start to wonder about the flip side: instead of reviewing iOS medical apps and pining for an optimized EHR experience on the iPad, what if there are features of the iPad that could limit the utility of medical apps?
Well, there are some product design issues, like impact resistance and bacterial colonization, that have been discussed. But the operating system, iOS 5, has some quirks, too. Some have received a lot of attention. Some are maddening in their capriciousness. Read more »
*This blog post was originally published at Blogborygmi*
December 28th, 2011 by RyanDuBosar in Research
No Comments »

The vast majority of U.S. physicians are moderately to severely stressed or burned out on an average day, with moderate to dramatic increases in the past three years, according to a survey.
Almost 87% of all respondents reported being moderately to severely stressed and/or burned out on an average day using a 10-point Likert scale, and 37.7% specifying severe stress and/or burnout.
Almost 63% of respondents said they were more stressed and/or burned out than three years ago, using a 5-point Likert scale, compared with just 37.1% who reported feeling the same level of stress. The largest number of respondents (34.3%) identified themselves as “much more stressed” than they were three years ago.
The survey of physicians conducted by Physician Wellness Services, a company specializing in employee assistance and intervention services, and Cejka Search, a recruitment firm, was conducted across the U.S., and across all specialties, in September 2011. Respondents Read more »
*This blog post was originally published at ACP Hospitalist*
December 26th, 2011 by PeterWehrwein in Research
1 Comment »

We are fast entering the era of the electronic health record, when it will be possible to call up our medical records on our computers and mobile devices. Medication lists, lab results, appointment schedules—they’ll all be available with clicks of your mouse or taps on the screen of your smartphone or tablet.
But one question that’s far from settled is whether the electronic health record should include the notes that doctors make about them. A doctor’s notes can be straightforward, such as a reminder that an additional test might be needed. But they can also include somewhat speculative observations and hunches about a patient and his or her medical conditions. The Open Notes project is a research program designed to test the consequences of giving patients access to doctors’ notes. Harvard-affiliated Beth Israel Deaconess Medical Center is one of the test sites.
The Open Notes project is far from finished. But results of a survey of the expectations that doctors and patients have for note sharing are being reported in today’s Annals of Internal Medicine.
I don’t think there are any great surprises here. More than half of the primary care physicians Read more »
*This blog post was originally published at Harvard Health Blog*
 Electronic medical record systems (EMRs) have become a part of the work flow for more than half of all physicians in the U.S. and incentives are in place to bring that number up to 100% as soon as possible. Some hail this as a giant leap forward for healthcare, and in theory that is true. Unfortunately, EMRs have not yet achieved their potential in practice – as I have discussed in my recent blog posts about “how an EMR gave my patient syphillis,” in the provocative “EMRs are ground zero for the deterioration of patient care,” and in my explanation of how hospital pharmacists are often the last layer of protection against medical errors of EPIC proportions.
Electronic medical record systems (EMRs) have become a part of the work flow for more than half of all physicians in the U.S. and incentives are in place to bring that number up to 100% as soon as possible. Some hail this as a giant leap forward for healthcare, and in theory that is true. Unfortunately, EMRs have not yet achieved their potential in practice – as I have discussed in my recent blog posts about “how an EMR gave my patient syphillis,” in the provocative “EMRs are ground zero for the deterioration of patient care,” and in my explanation of how hospital pharmacists are often the last layer of protection against medical errors of EPIC proportions.

 For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “
For the past couple of years I’ve been working as a traveling physician in 13 states across the U.S. I chose to adopt the “