March 18th, 2011 by Emergiblog in Humor, Opinion, True Stories
1 Comment »

This is so wrong.
You can’t make this stuff up.
It seems an emergency department in Memphis, Tennessee is now taking online reservations for their services. Yes, you heard that right, you can now hop online and select the time you would like to be seen for your “emergency”. Just pay $15.00 and you can give your chief complaint, your medical history and your list of medications ahead of time, saving you time and trouble when you pop in with your pesky problem!
What if the problem is serious?
The computer won’t let you register and flashes a “Call 911″ sign at you.
But wait! There’s more!
If you are not seen within 15 minutes of your scheduled time, you money is cheerfully refunded!
I’m not kidding. Read more »
*This blog post was originally published at Emergiblog*
March 17th, 2011 by Shadowfax in Health Tips, True Stories
No Comments »

I’ve remarked in the past how rarely I ever learn anything useful from physical exam. It’s one of those irritating things about medicine — we spent all that time in school learning arcane details of the exam, esoteric maneuvers like pulsus paradoxus, comparing pulses, Rovsing’s sign and the like. But in the modern era, it seems like about half the diagnoses are made by history and the other half are made by ancillary testing. Some people interpreted my comments to mean I don’t do an exam, or endorse a half-assed exam, which I do not. I always do an exam, as indicated by the presenting condition. I just don’t often learn much from it. But I always do it.
The other day, for example, I saw this elderly lady who was sent in for altered mental status. There wasn’t much (or indeed, any) history available. She was from some sort of nursing home, and they sent in essentially no information beyond a med list. The patient was non-verbal, but it wasn’t clear if she was chronically demented and non-verbal or whether this was a drastic change in baseline. So I went in to see her. I stopped at the doorway. “Uh-oh. She don’t look so good,” I commented to a nurse. As an aside, this “she don’t look so good” is maybe 90% of my job — the reflexive assessment of sick/not sick, which I suppose is itself a component of physical exam. But I digress. Her vitals were OK, other than some tachycardia*. Her color, flaccidity and apathy, however, really all screamed “sick” to me. Of course, the exam was otherwise nonfocal. Groans to pain, withdraws but does not localize or follow instructions. Seems symmetric on motor exam, from what I can elicit. Belly soft, lungs clear. Looks dry. No rash. Read more »
*This blog post was originally published at Movin' Meat*
March 14th, 2011 by DrWes in Health Policy, Opinion
No Comments »

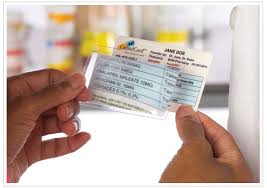 Give me your medication list and I’ll tell you your health problems. It happens every day in emergency rooms across the country as confused elderly patients present for an acute problem unable to describe their past medical history, but equipped with a list of medications in their wallet:
Give me your medication list and I’ll tell you your health problems. It happens every day in emergency rooms across the country as confused elderly patients present for an acute problem unable to describe their past medical history, but equipped with a list of medications in their wallet:
Metformin = Type-2 diabetes
Synthroid = Hypothyroidism
Lipitor + Altace + Lasix + Slo-K = Ischemic cardiomyopathy
Lexapro = A little anxious or depressed
Viagra = Well, you know…
I bet I’d be right better than 90 percent of the time. Now, imagine you’re a pharmaceutical company wanting to target people with those chronic diseases. Where might you find them?
No problem. Just pay the insurers to provide you patients’ drug lists. No names need be exchanged in keeping with HIPAA requirements. But the drugs list attached to folks’ cable TV box? Perfect. You’re in — with no legal strings attached. Then, according to the Wall Street Journal, just fire away with that targeted direct-to-consumer advertising on TV, courtesy of your local healthcare insurance provider.
No wonder our healthcare industry movers and shakers love the electronic medical record. Healthcare privacy? What healthcare privacy?
-WesMusings of a cardiologist and cardiac electrophysiologist.
*This blog post was originally published at Dr. Wes*
March 6th, 2011 by Edwin Leap, M.D. in Opinion, True Stories
1 Comment »

 Here’s my column in the March issue of Emergency Medicine News.
Here’s my column in the March issue of Emergency Medicine News.
Second Opinion: Be Smarter Than Your Brain
“Everyone is a drug seeker. Why does everyone want to be on disability? I’m so tired of lies. Great, another lousy shift. I wonder who will die tonight? I’m so sick of suffering. I’m so weary of misery and loss. I hope this never happens to my family. I’ll probably get sued. Being sued nearly drove me crazy. This job never gets easier, only harder. I have to find something else to do; I can’t go on this way. I think I’m going crazy. I don’t have any more compassion. People hate me now.”
These are only a few of the wonderful thoughts that float through the minds of emergency physicians these days. Sure, not every physician has them. But I know our specialty, I know our colleagues, I hear from doctors around the country and I see that fear, frustration and anxiety are common themes.
Older physicians fantasize about career changes, and younger ones are often blind-sided by the hard realities of practice outside of their training programs (where their work-hours and staffing do not necessarily reflect the world beyond).
We are crushed by regulations and overwhelmed by holding patients, often put in situations where we are set squarely between the devil and the deep blue sea. “Spend more time with your patients; see them faster. Don’t let the ‘psychiatric hold’ patient escape; why are you using so much staff on psychiatric patients? See chest pain immediately; why didn’t you see the board member’s ankle injury as fast as the chest pain?”
In all of this mess of emergency medicine, we often find ourselves frustrated and bitter. But is it only because of our situations? They are admittedly daunting. But is our unhappiness merely the result of the things imposed on us? Or could it be more complex than that? Lately, I have come to wonder if our thoughts are perhaps worse enemies than even lawsuits, regulations, or satisfaction scores. Read more »
*This blog post was originally published at edwinleap.com*
February 26th, 2011 by Steven Roy Daviss, M.D. in Health Policy, Opinion
No Comments »


I read today that Eastern Ontario has started a bed registry to keep track of where open psychiatric beds are available. This is something I’ve long advocated. The United States now has less than 10 percent of the beds it used to have 50 years ago. Granted, treatment has improved and community resources are enhanced. But there are still areas that often do not have a sufficient number of hospital beds for folks needing acute inpatient psychiatric care.
 The Ontario story described in the Ottawa Citizen states that six of the area hospitals have been connected to a computerized “bed board” that provides real-time information on who has an appropriate bed available. This saves time in the ER and gets patients to needed treatment more quickly. Otherwise calls need to be made to each individual hospital, which is very time-consuming.
The Ontario story described in the Ottawa Citizen states that six of the area hospitals have been connected to a computerized “bed board” that provides real-time information on who has an appropriate bed available. This saves time in the ER and gets patients to needed treatment more quickly. Otherwise calls need to be made to each individual hospital, which is very time-consuming.
And it’s not uncommon for all the beds to be full. Last July there was an EMTALA complaint against a hospital in Maryland because a patient sat in the ER all weekend, and this hospital said they had no beds to admit the patient to. The Department of Health and Mental Hygiene (DHMH) investigated the complaint and found that indeed the hospital was full that weekend. The ER’s record indicated that all the hospitals (except the state hospitals) were called that weekend and all indicated their beds were full. So DHMH visited every hospital (about 28, I think) thinking that surely one of them had an empty bed they were hiding. What they discovered was that every single psychiatric bed in the state was full.
Unfortunately, we have no way of determining how often this happens, but we know if happens often enough. A “bed board” like this would be very helpful in quickly finding beds when needed and keeping track of the extent of this problem. Having patients wait in ER for days is unsafe and is even discriminatory. How many people with stroke or uncontrolled diabetes sit in ER for days waiting to find a bed for treatment? I’d like to hear others’ thoughts on how this problem can be addressed.
*This blog post was originally published at Shrink Rap*


















