August 22nd, 2009 by GruntDoc in Better Health Network, True Stories
2 Comments »

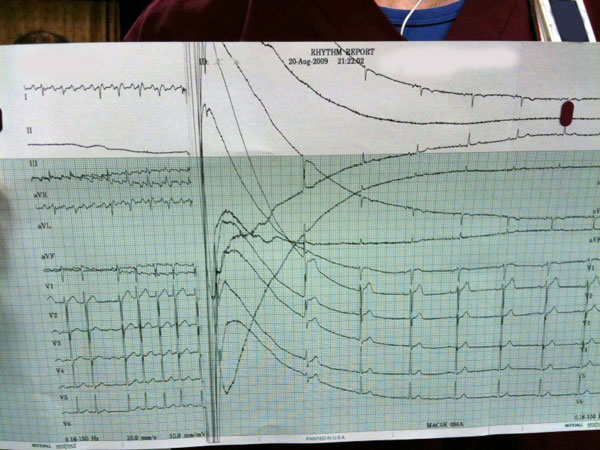
Today’s included the therapeutic application of electricity
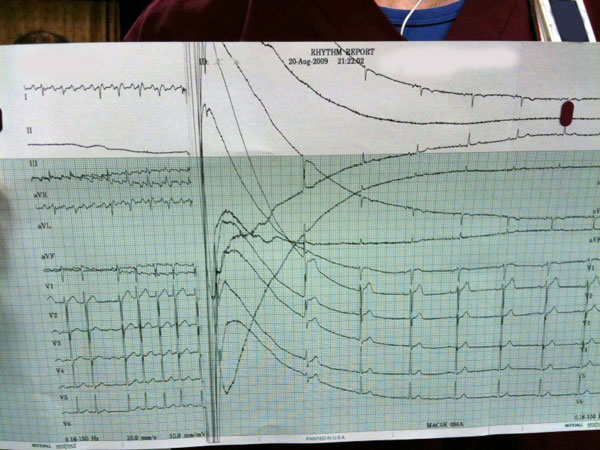
and a real oddity: an adolescent with a potassium of 1.8 (yes, I repeated it).
Emergency Medicine can be mundane occasionally, but days like today make for a really nice change.
*This blog post was originally published at GruntDoc*
August 18th, 2009 by Paul Auerbach, M.D. in Better Health Network
No Comments »

 I’m often asked about technologies that are amenable to research applied in outdoor or wilderness settings. A company called Cantimer has developed and made available one of these technologies.
I’m often asked about technologies that are amenable to research applied in outdoor or wilderness settings. A company called Cantimer has developed and made available one of these technologies.
Cantimer is a privately–held, development–stage company commercializing a patented, proprietary, sensor technology platform based on a convergence of micro electromechanical systems (MEMS) technology and advanced polymer science. According to the website, the Company’s first commercial product will be an innovative, hand–held device for non-invasive measurement and monitoring of human hydration status from the osmolality of saliva.
This past October (2008), there was a press release issued by the Company. To paraphrase:
“Cantimer, Inc. Delivers First Alpha Instruments for Real-Time, Non-Invasive, Incident-Scene Assessment of Dehydration in Firefighters
Devices to be used for field testing in structural fire environments and search and rescue operations.
Cantimer, Inc. announced that it has shipped ten alpha instruments for real-time, non-invasive assessment of human hydration to the U.S. Government’s Technical Support Working Group (TSWG). The units will be used for incident-scene assessment of dehydration in firefighters. Dr. Christina Baxter, from TSWG, commented, ‘The focus over the last several months has been on laboratory work that adds to the body of knowledge regarding salivary osmolality as a useful measure of human hydration or dehydration status. That work has gone very well. We are now looking forward to using these new devices for actual field testing in structural firefighting or search and rescue operations – with more of an emphasis on implementation, ergonomics and the user experience.’
Maintaining an optimal level of hydration is a major health concern for firefighters and other emergency scene first responders. Progressive acute dehydration associated with physical exertion in heat-stressed environments significantly increases the risks of temperature-related health problems, with resulting losses of productivity and, in some cases, death. It has been shown that fluid losses of as little as 2% of total body weight (3.5 pounds in a normally 175 pound individual) can lead to noticeable compromises in physical and cognitive performance.
Dehydration and resulting temperature-related health problems among firefighters are preventable through adequate on-scene hydration management. Cantimer’s devices, incorporating the Company’s proprietary sensing technology, enable convenient, field-deployable, real-time measurement, and therefore management, of hydration status from an easily-obtained sample of saliva.
Although easy to treat if identified early, dehydration is a pervasive condition that contributes to a large number of preventable hospitalizations in the U.S. every year. Cantimer believes that the availability of a hand-held device that aims to make it as easy to determine a person’s state of hydration as it is to take their body temperature will have significant benefits, not only for the health and safety of firefighters and other first-responders, but for military personnel, athletes at all levels, the elderly, the very young and those suffering from a wide range of medical conditions.”
The wilderness and outdoor medicine literature is replete with opinions and arguments about conditions predisposing to dehydration and the determination of hydration status. We presume dehydration in the field by clinical diagnosis (e.g., signs and symptoms), but do not generally deploy an actual quantifiable measurement to determine its presence. So, with the advent of the technology espoused by Cantimer, we may finally have a convenient tool with which to begin to diagnose, as opposed to predict, dehydration, during virtually any activity for which the physical environment will allow its use. This will hopefully also allow us to test different hydration/rehydration strategies, including various fluids, electrolyte concentrations, and so forth.
This post, Spit Test To Determine Hydration Status, was originally published on
Healthine.com by Paul Auerbach, M.D..
August 18th, 2009 by Emergiblog in Better Health Network, Health Policy, True Stories
2 Comments »

She didn’t eat her dinner Friday night.
By 4: 30 am Saturday, the previously healthy 65-year-old female had a fever and lower extremity weakness. A family member heard her repetitive moaning. The patient got up to void, but could barely negotiate the one step up to the hallway. As she negotiated the hallway, she staggered.
By 5:00 am she was in the ER.
*****
The patient was taken to an exam room. Vital signs were taken and it was noted that the patient’s fever was “extremely high”. The doctor came into the room and the temp was re-taken. Extremely high. The patient had no insurance and was not verbal; the doctor discussed options with the family member.
The goal: find the source of the fever and begin treatment. A CBC, Chem 14, a urinalysis, an IV and hydration would be started. No lactate level would be done; the doctor stated it would be pointless to run a test that she already knew would be elevated based on clinical presentation. Blood cultures would be drawn, but not sent immediately. As the doctor explained, they are expensive and it would take days before the test results would be back.
In this facility, payment was expected at the time of treatment and a detailed estimate was provided to the family. The low end of the estimate was the deposit.
*****
By 8:30 am Saturday, the fever was still raging; the lab tests were normal. The patient was in ice packs with a fan in an attempt to lower the fever. An IV antibiotic was initiated; hydration was on-going. An internist and a neurosurgeon were consulted as the patient was experiencing lower back pain in addition to the profound weakness. The patient was admitted.
Further tests were proposed: lumbar x-ray to rule out spondylitis and, given the patient’s age, a chest x-ray to rule out occult pneumonia. The pros and cons of each test were fully explained along with rationale and the cost.
*****
The radiographic exams were normal. A loose bowel movement that morning had been blood-tinged. The patient had been medicated for pain. A second antibiotic was started. The next step would be an abdominal ultrasound, as no obvious source for the fever had been found. The rationale for the test and the cost were discussed and the family gave the go-ahead.
The spleen. Enlarged and mottled on ultrasound. A call was made to the family to discuss needle aspiration to rule out lymphoma.
*****
Monday morning the patient’s fever was down. She was eating. She was voiding. She was still weak, still moved slowly and awkwardly. She would be discharged home on oral antibiotics with the results of her spleen aspirate pending.
*****
It’s been a week now and the patient is acting 100% normally.
The patient was my dog, a 10-year-old, 70 pound Shepherd mix. We still don’t know what nearly killed her last weekend. The spleen aspirate was abnormal, but not lymphoma. The fact that the fever responded to antibiotics (as did the weakness) leaves us with the feeling that it was an infection in such an early stage that the source was not obvious.
I realize veterinary medicine is not human medicine, and a million holes can be found in my attempt to draw a parallel between them. But a few things crossed my mind during this experience:
(a) Tests were not done just for the sake of testing or because a printed standard said they should be. This was not template medicine dictated by any outside organization or government regulations.
(b) The doctor/patient relationship was unencumbered by insurance company approvals, government regulations, billing, coding or the number of patients that had to be seen in a certain time frame.
(c) there was full transparency regarding what each test would cost.
Maybe the human health care system can take a few pointers from what the veterinary world has been doing all along.
(P.S. I just realized you can read this story from the vantage point of ME being the third-party payer standing between the vet and my dog, deciding what would be “covered” – i.e. paid for. Interesting either way….)
*This blog post was originally published at Emergiblog*
August 16th, 2009 by Shadowfax in Better Health Network
3 Comments »


The sense of smell is a very powerful sensation. A distinctive fragrance can stir up a long-forgotten memory, or put you in a place you haven’t been in years. There’s a certain clean, dusty smell that always reminds me of the cottage on Wisconsin’s Lake Koshkonong, which we used to rent every year when I was a kid. There’s a perfume that always reminds me of a girl who I briefly dated in high school. The girl was forgettable but the aroma was not. We all have these triggers and associations.
All this occurred to me last night as I hunched over the face of an intoxicated gentleman who had lost a fight with the pavement. He was unresponsive, and I was painstakingly stitching back together the tattered pieces of his lips and forehead. Every time he exhaled, I was subjected to an intense and pungent smell of dried blood, saliva and alcohol. It’s an acrid scent, sour, with an overlying cloying sweetness. Very distinct and unpleasant.
And that, my friends, is the smell of the ER.
At least for me. I will never be able to smell that in my life without being immediately transported back to this place and activity (repeated so many times over the years). Fortunately, I am unlikely to ever experience this particular smell outside of the ER. Later, after the ER emptied out for the night, I discussed this with a few nurses & others. Not surprisingly, there was quite a diversity of opinion. One nurse insisted that the smell that, for her, screamed “ER” was that of melena (bloody stool from a brisk GI bleed — also very pungent) It can fill the entire department when you have one GI bleeder. You come into work, smell the melena the moment you walk in, and you just know what sort of shift it’s going to be. A tech said that the scent he thinks of as “ER” is the sweet plastic smell of freshly opened oxygen tubing. Another nurse came up with an inventive and hysterical bit of slang that I just can’t bear to repeat for, um, how shall I say it, the ammonia and fishy smell of unclean or diseased lady parts.
Ultimately (of course) we came up with a list of “Smells of the ER”:
- Alcohol, Saliva & Dried Blood
- Fresh Plastic Tubing
- Melena
- Feminine Issues
- A Freshly Incised Abscess
- 80-proof Vomit
- Clostridium Difficile (a GI illness producing a distinctive smelly diarrhea)
- “Hobo Feet”
- Coffee Grounds in a tray (used by nurses to freshen the air and cover some smells)
Surely there are more — perhaps you can contribute some in the comments. It’s gotta be distinctive to the ER, though, or at least a medical setting. Just poop or vomit doesn’t cut it. And, like the plastic tubing, it doesn’t have to smell bad, necessarily.
So what do you think?
*This blog post was originally published at Movin' Meat*
August 12th, 2009 by Gwenn Schurgin O'Keeffe, M.D. in Better Health Network
No Comments »

During a recent emergency room shift, I treated a 12 year old boy for a swimmer’s ear. During the visit, I learned he was from the South and was in the area visiting relatives before starting school in a couple weeks. It turns out he’s been battling this pain for a couple weeks and his mom is convinced it’s because of all the swimming he’s done this summer. Instead of rushing him to his own pediatrician at home, she has been “riding it out” to see if the pain resolved on it’s own.
This was true music to my ears! Most parents rush their kids to the doctor at the first sign of ear pain, even though the current recommendations are to not use antibiotics in this age group unless the pain persists or worsens past the first few days. So, if his exam were abnormal, my decision making process would be much simpler.
What wasn’t music to my ears was learning I was the second physician to see the boy that week. The grandmother took him to see her physician when she had a scheduled appointment a couple days earlier, “just for a curbside” and learned that he did in fact have “an ear infection”. No medications were given or appointment facilitated with a pediatrician or other physician. This was truly just a curbside. The family was left with no alternative but to use the ER.
The ER often ends up being our only option when visiting an area out of town, isn’t it? If staying at a hotel, many do have a cool option that provides a physician call service so a physician will come to you, as I learned a couple year’s back in Disneyland. And, some cities do have free-standing urgent-care centers that can help with these sorts of non-911 situations. But, by and large, the ER is it in most areas and for most people.
What a backwards situation! The majority of sick people have situations that do not need the ER yet find themselves having to because there are simply no other options. Think about how much time and money would have been spared for this family and the system had that first physician just seen the child as an office visit and written the same prescriptions I wrote 2 days later during the ER visit. Think about the healthcare savings to the system and personal savings to families if we had the same theoretical options to the hundreds of thousands of annual after-hours urgent care visits our system sees each year but is current seeing in the wrong setting!
In the big picture, seeing a basic sick visit after hours in the ER is like trying to crack a nut with a sledgehammer. It makes about as much sense, too. The truth is we just have no place for the after hours regular sick people, which, by the way, are the majority of people who get sick after hours, especially if their doctor is in another state!
It’s really not a shock ER wait times are so long…ERs are over loaded with patient’s just like this boy. Until we find a better system, better take along your iPod and a good book should you find yourself heading to the ER. You’ll be in very good company waiting to be seen so may as well come prepared for the wait.
*This blog post was originally published at Dr. Gwenn Is In*







 The sense of smell is a very powerful sensation. A distinctive fragrance can stir up a long-forgotten memory, or put you in a place you haven’t been in years. There’s a certain clean, dusty smell that always reminds me of the cottage on Wisconsin’s Lake Koshkonong, which we used to rent every year when I was a kid. There’s a perfume that always reminds me of a girl who I briefly dated in high school. The girl was forgettable but the aroma was not. We all have these triggers and associations.
The sense of smell is a very powerful sensation. A distinctive fragrance can stir up a long-forgotten memory, or put you in a place you haven’t been in years. There’s a certain clean, dusty smell that always reminds me of the cottage on Wisconsin’s Lake Koshkonong, which we used to rent every year when I was a kid. There’s a perfume that always reminds me of a girl who I briefly dated in high school. The girl was forgettable but the aroma was not. We all have these triggers and associations.










