April 4th, 2011 by RyanDuBosar in News, Research
No Comments »

Improving handoffs from the emergency room back to the primary care physician will require changing how electronic health records are used, better reimbursement to both the hospital and ambulatory doctors, and malpractice reform, according to a study. The rising use of hospitalists and larger primary care practice sizes has contributed to the difficulties faced when an ER doctors tries to reach a physician who best knows the patient.
Haphazard communication and poor coordination can undermine effective care, according to a new research conducted by the Center for Studying Health System Change. Researchers conducted 42 telephone interviews between April and October 2010 with 21 pairs of emergency department and primary care physicians, who were case-matched to hospitals so the perspective of both specialties working with the same hospital could be represented.
Among the findings in the report, telephone communication was essential in some cases, but particularly time-consuming. Both emergency and primary care physicians reported successful completion of each telephone call often required multiple pages and lengthy waits for callbacks. While placing and receiving telephone calls might seem straightforward and quick, providers said each small action multiplied across dozens of patients can become a daunting burden, with little immediate reward or reimbursement. Read more »
*This blog post was originally published at ACP Hospitalist*
March 14th, 2011 by DrWes in Health Policy, Opinion
No Comments »

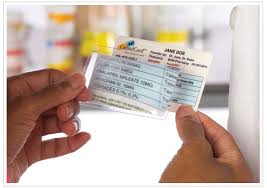 Give me your medication list and I’ll tell you your health problems. It happens every day in emergency rooms across the country as confused elderly patients present for an acute problem unable to describe their past medical history, but equipped with a list of medications in their wallet:
Give me your medication list and I’ll tell you your health problems. It happens every day in emergency rooms across the country as confused elderly patients present for an acute problem unable to describe their past medical history, but equipped with a list of medications in their wallet:
Metformin = Type-2 diabetes
Synthroid = Hypothyroidism
Lipitor + Altace + Lasix + Slo-K = Ischemic cardiomyopathy
Lexapro = A little anxious or depressed
Viagra = Well, you know…
I bet I’d be right better than 90 percent of the time. Now, imagine you’re a pharmaceutical company wanting to target people with those chronic diseases. Where might you find them?
No problem. Just pay the insurers to provide you patients’ drug lists. No names need be exchanged in keeping with HIPAA requirements. But the drugs list attached to folks’ cable TV box? Perfect. You’re in — with no legal strings attached. Then, according to the Wall Street Journal, just fire away with that targeted direct-to-consumer advertising on TV, courtesy of your local healthcare insurance provider.
No wonder our healthcare industry movers and shakers love the electronic medical record. Healthcare privacy? What healthcare privacy?
-WesMusings of a cardiologist and cardiac electrophysiologist.
*This blog post was originally published at Dr. Wes*
February 25th, 2011 by Peggy Polaneczky, M.D. in Opinion, True Stories
No Comments »

A pathologist uses the EMR to find out just a little more about the patient whose cerebro-spinal fluid she has under her microscope — and changes her diagnosis:
This patient had a diagnosis of plasma cell myeloma with recent acute mental status changes. So the lone plasma cell or two I was seeing, among the lymphs and monos, could indicate leptomeningeal spread of the patient’s disease process. I reversed the tech diagnosis to atypical and added a lengthy comment – unfortunately there weren’t enough cells to attempt flow cytometry to assess for clonality of the plasma cells to cinch the diagnosis. But with the information in the EMR I was able to get a more holistic picture on a couple of cells and provide better care for the patient. I cringe to wonder if I might have blown them off as lymphs without my crutch.
The much-hoped-for improvement in quality due to the adoption of EMRs has been elusive to date, so anecdotal experiences like this will be important evidence to consider in judging the impact of the EMR on healthcare outcomes.
Kudos to pathologist Gizabeth Shyner, who writes over at Mothers in Medicine and her own blog, Methodical Madness, for “thinking outside the box.”
*This blog post was originally published at The Blog That Ate Manhattan*
January 18th, 2011 by Michael Kirsch, M.D. in Better Health Network, Opinion
No Comments »

 Whistleblower readers know of my criticisms of the electronic medical record (EMR) juggernaut that is oozing over the medical landscape. Ultimately, this technology will make medical care better and easier to practice. All systems will be integrated, so that a physician will have instant access to his patients’ medical data from other physicians’ offices, emergency rooms and hospitals.
Whistleblower readers know of my criticisms of the electronic medical record (EMR) juggernaut that is oozing over the medical landscape. Ultimately, this technology will make medical care better and easier to practice. All systems will be integrated, so that a physician will have instant access to his patients’ medical data from other physicians’ offices, emergency rooms and hospitals.
In addition, data input in the physician’s office will use reliable voice activated technology, so that some antiquated physician behaviors, such as eye contact, can still occur. Clearly, EMR is in transition. I place it on the 40 yard line, a long way from a touch down or field goal position.
A colleague related a distressing meeting he had at the community hospital he works at. This hospital, like nearly every hospital in Cleveland, is owned by one of the two towering medical behemoths. I’m not a businessman, but I have learned that when something owns you, it’s generally better for the owner than the ownee. This meeting was about the hospital’s upcoming EMR policy. Sometimes, these hospital meetings are ostensibly to seek physician input, but the true purpose is to inform the medical staff about decisions that have already been made.
In the coming months, this hospital will adopt a computerized ordering system for all patients. In theory, this would be a welcome advance. It would create a digital and permanent record of all physician orders that could be accessed by all medical personnel involved in the patients’ care. It would solve the perennial problem of inscrutable physician handwriting, including mine. Read more »
*This blog post was originally published at MD Whistleblower*
December 23rd, 2010 by CodeBlog in Better Health Network, Interviews
No Comments »

Ever wonder how all those hospital systems are created and maintained? (Computer charting, systems to report data to national and state organizations, to name a couple.) Sure, they could hire some IT guy to run them, but everything seems to flow better with a nurse’s touch. After all, we’re the ones using them all the time, right? Jen C, RN, BSN almost MSN gives us a look into the world of nursing informatics.
Jen has been doing this job for two years. She says she “stumbled into it” when she was interviewing for a new job and mentioned that she was starting her master’s in informatics. Although she was hired to be a staff nurse, within four months she was working in informatics.
What do you do all day?
Each day is different. I do a lot of troubleshooting. I go to a lot of meetings. I do system development and upkeep. I listen to the nurses and what their issues are with the various systems. I do education. And I still fill in at the bedside (I’m still a NICU nurse at heart.)
What frustrates you about your job?
Little definition and recognition as to what my job is. I often seem to be a catch-all. I also don’t have a mentor. I’m the only one in my hospital that has formal education in this area and only one or two in the whole hospital. Read more »
*This blog post was originally published at code blog - tales of a nurse*
















