August 21st, 2010 by Edwin Leap, M.D. in Better Health Network, Humor, True Stories
No Comments »

Here’s my column in the August edition of Emergency Medicine News. A person who seems powerless may hold an entire emergency room hostage!
Magic Words: ‘I Have Chest Pain’
Propped in her bed, frail and weak, the little grandma sighed. Her complaints were legion: weakness, poor appetite, poor sleep, joint pain, cough, dry mouth. Her daughter, eyes rolling, was trying to balance three reasonable emotions. She desperately wanted to go home and rest after spending the day in the ER. She truly wanted to avoid her mother’s admission to the hospital, and she was, graciously, sympathetic to the physician who brought the bad news.
‘Mrs. Adkins, I know you feel poorly, and I’m sorry. But I have to say, I can’t find any reason to admit you to the hospital. You’re right as rain. Isn’t that great?’
‘You mean, I’ve been here all this time, and had a gallon of blood drawn, and all them x-rays and a CAT scan, and there ain’t nothing wrong? I can’t believe that. I feel terrible.’ When she said the word terrible, she smacked her lips and looked away. She propped her hands on her lap and intertwined them; and she managed a subtle, but expressive, sniffle. Read more »
*This blog post was originally published at edwinleap.com*
August 18th, 2010 by Shadowfax in Better Health Network, Health Policy, News, Opinion
No Comments »
An alert reader alerted me to this related piece in Slate: “We Can’t Save You: How To Tell Emergency Room Patients That They’re Dying.” An excerpt:
The ER is not an easy place to come to these realizations or assess their consequences. A handful of physicians are trying to change that. Doctors like Tammie Quest, board-certified in both palliative and emergency medicine, hope to bring the deliberative goal-setting, symptom-controlling ethos of palliative care into the adrenaline-charged, “tube ’em and move ’em” ER. Palliative/emergency medicine collaboration remains rare, but it’s growing as both fields seek to create a more “patient-centered” approach to emergency care for the seriously ill or the dying, to improve symptom management, enhance family support, and ensure that the patient understands the likely outcomes once they get on that high-tech conveyor belt of 21st-century emergency medicine.
Emergency medicine and palliative care-certified? That’s an interesting mix. We have a great palliative care service where I work (in fact, it just won the national “Circle of Life” award.) It makes a lot of sense to have a palliative care nurse stationed in (or routinely rounding) the ER, though. I think I’m going to suggest this to our hospice folks.
*This blog post was originally published at Movin' Meat*
August 15th, 2010 by GruntDoc in Better Health Network, Humor, Opinion, True Stories
No Comments »

 I’ve internalized all the dogma of medicine, for good and bad.
I’ve internalized all the dogma of medicine, for good and bad.
When I was an EMT, green as a twig in an ER, I learned the basics: For any wound with hair employ the razor, and get the hair away from the laceration so the doc could do a good closure.
So, employment week #3: Eyebrow laceration? Shaved that sucker clean off. ER doc freaked out, and I learned some medical dogma: Don’t shave eyebrows, they don’t grow back. Heard it later, too — all the way through training, in fact. Read more »
*This blog post was originally published at GruntDoc*
August 11th, 2010 by RyanDuBosar in Better Health Network, Health Policy, News, Research
No Comments »

Office-based practices are focusing increasingly on patients 45 and older, reports the Centers for Disease Control and Prevention.
In 2008, those 45 and older accounted for 57 percent of all office visits, compared to 49 percent in 1998. Prescriptions, scans and time spent with the doctor also became increasingly concentrated on those middle aged and older, according to data from the CDC’s National Center for Health Statistics.
Also, physician visits increasingly concentrated on medical and surgical specialists and less on care provided by primary care practitioners for those ages 45 and older. Furthermore, for patients ages 65 and older, the percentage of visits to primary care specialists decreased from 62 percent to 45 percent from 1978 to 2008, while the percentage of visits to physicians with a medical or surgical specialty increased from 37 percent to 55 percent. Read more »
*This blog post was originally published at ACP Internist*
August 6th, 2010 by Happy Hospitalist in Better Health Network, Humor
No Comments »

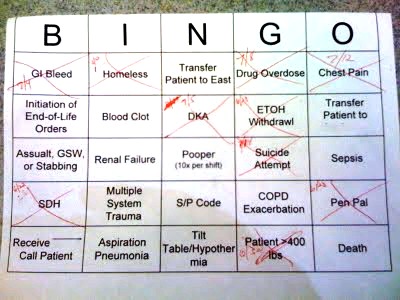
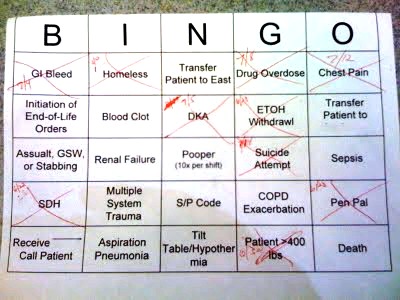
Ever wonder how ICU nurses get through their daily grind? Why, with ICU Bingo, of course.
How does ICU Bingo work? It works just like regular bingo. Every nurse receives their own Bingo card with different ICU diagnoses. And every time they take care of one of these conditions, they get to “x” it out. Fill out a line or any other predetermined design pattern, and you are the ICU Bingo winner, and you win a prize.
This is quite similar to my 2010 March Madness Hospitalist Bracket, only in this case the game is Bingo. As you can see, this nurse has already cared for a GI bleed, a homeless man, a drug overdose, chest pain, DKA, alcohol withrawal, subdural hematoma, a prisoner, and someone with super-morbid obesity. That’s ICU medicine for you.
*This blog post was originally published at The Happy Hospitalist*




 I’ve internalized all the dogma of medicine, for good and bad.
I’ve internalized all the dogma of medicine, for good and bad.