November 3rd, 2014 by Dr. Val Jones in Health Tips, Opinion
214 Comments »
 Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.
Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.
Because EPIC keeps lists of home meds, discontinued meds, and current meds available for review and reactivation, it takes little more than one misplaced check box to order the wrong dose or type of medication. Physicians who transfer a patient to another service can indicate their intended medication list and keep it “on hold” for the receiving physician to review and approve. Unfortunately, the software’s tab system is so complex that it’s extremely difficult to find that list and activate it. Lost in a sea of admissions tasks and order boxes in different fonts, colors, and drop down menus, one often accidentally reviews and approves discontinued types and doses of medicines. The only protection against such errors is the hospital pharmacist.
With each new admission to the inpatient rehabilitation unit, I had to resort to calling a pharmacist for help. I was terrified that I would accidentally insert medication errors into the patient’s order set by carrying forward discontinued meds. The long-suffering pharmacists explained to me that “most physicians make medication order errors in EPIC with each admission.” They said that they regularly had to talk physicians out of throwing their computer out the window in a state of extreme frustration. They also said that their EPIC user environment looked very different (and less confusing) than what the physicians used, so that they couldn’t even provide real-time phone guidance regarding order entry process.
The scary thing is that EPIC has the largest market share of any EMR in the United States. It is also (in my experience) the most prone to medical errors due to its overly complex medication reconciliation process. I have used other EMRs that have far simpler and more intelligent medication order entry processes. Soarian (Sieman’s EMR, just sold to Cerner) has, for example, an outstanding order entry system. So my complaint is not that “all EMRs are bad” – it’s that some have particularly flawed designs that are causing real harm to untold millions of patients. We just haven’t documented the harm yet. I tremble at the thought of what we’d find.
Until electronic medication reconciliation is made safer, pharmacists will be working overtime to correct records and protect patients from carry over errors. I thank my lucky stars that I have had vigilant, determined pharmacists by my side as I cared for very complex, sick patients who were exceptionally vulnerable to dosing errors. There has never been a more important time to exercise caution when entering hospital medication orders, or to express your appreciation for pharmacists. Without their help we might all be experiencing medication errors of EPIC proportions.
November 20th, 2011 by ErikDavis in News, Quackery Exposed
No Comments »
Hey there skeptifans. Here are the media Fails and Wins you sent me last week.

Edzard Ernst on alternative medicine
After Steve Jobs death, which we now know may have been hurried due to his decision to choose alternative treatments over evidence based ones, Maclean’s chose to run this Q&A with alternative medicine expert Edzard Ernst. Several years ago Dr. Ernst set out to find out if there is evidence to support the most popular alternative treatments. His findings were that the vast majority of alternative medicine is quackery. I hope this interview will help sway some people on the fence about chiropractic and other placebo treatments.
Family Doc Says No To Perilous Chickenpox Pops
Anna spotted this story on NPR. Apparently, there is a mom in Texas selling chicken pox infected lollipops to Read more »
*This blog post was originally published at Skeptic North*
May 11th, 2011 by Stanley Feld, M.D. in Health Policy, Opinion
No Comments »

In an ideal world ACOs should work. There is no evidence that untested and complex organizational structure of ACOs developed by Dr. Don Berwick (head of CMS) will improve quality of care and reduce costs.
ACOs are supposed to provide financial incentives to health care organizations to reduce costs and improve quality. There are too many defects in the ACOs infrastructure to improve the financial and medical outcomes.
At a conceptual level, the incentive for ACOs would be to increase efficiency and avoid overuse and duplication of services, resources, and facilities. In this model, ACO members would share the savings resulting from the increased coordination of care.
I have said over and over again that excessive administrative fees and ineffective management of chronic disease is the main source of waste in the healthcare system. ACOs do not deal with these main drivers of costs.
The only stakeholders who can demand that this waste be eliminated are consumers/patients. Patients must control their healthcare dollars. They will make sure there are competitive prices and will not permit duplication of services. Read more »
*This blog post was originally published at Repairing the Healthcare System*
November 19th, 2009 by Steve Novella, M.D. in Better Health Network, Quackery Exposed
4 Comments »

Homeopathy, as a cultural phenomenon, remains an enigma. In the two centuries since its invention it has failed to garner significant scientific support. In fact, developments in physics, chemistry, biology, and medicine have shown the underlying concepts of homeopathy to be wrong – guesswork and speculation that lept in the wrong direction.
It turns out, like does not cure like. This is nothing more than sympathetic magic – popular at the time but now considered nothing more than superstition without any scientific basis.
It also turns out that diluting a substance does not make it more potent – this nonsensical idea (ridiculed even in the 19th century) violates the laws of thermodynamics, and the chemical principle of mass action. This is especially true when you dilute a substance beyond the point where chance would have even a single molecule of active ingredient left behind. The background noise of chemicals in homeopathic water is orders of magnitude greater than the signal of whatever had previously been diluted in it. Read more »
*This blog post was originally published at Science-Based Medicine*
September 8th, 2009 by Berci in Better Health Network, Humor
No Comments »

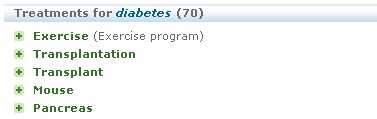
I wanted to write about Healthbase, a new medical search engine, but David Rothman was faster. He found some serious mistakes in the search itself.

Well, the concept to reduce the number of results to a definitive list of categories is a good one. But it leads to some mistakes. First, it searches in databases such as Wikipedia. You cannot find a bigger fan of Wikipedia than me, but still it’s not suitable for such a search engine.
Second, sometimes there are strange things in the results. Only one example below. It seems to suggest that a possible treatment for diabetes is mouse. Of course, it just found articles mentioning mouse models in the research of diabetes treatments, but it cannot deal with the information properly.
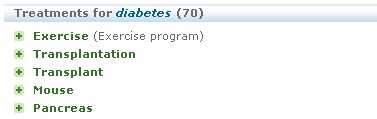
So there are a lot of things to do before becoming the ultimate engine. Until then, my suggestion is Scienceroll Search, the first personalized medical search engine:

*This blog post was originally published at ScienceRoll*
 Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.
Most hospitalized patients and families don’t realize that life-threatening medication errors are regularly thwarted by pharmacists. They are truly the unsung heroes of patient care. I just finished a locum tenens assignment at a hospital that uses EPIC as their electronic medical records system, and I was stunned by the impossibly complex medication reconciliation process. Each time a patient is admitted to the hospital, or transferred to another part of the hospital, a physician must review, approve, and re-order their medications. While this may seem like a good way to insure that medication errors are avoided, it actually has the exact opposite effect.