May 28th, 2010 by Toni Brayer, M.D. in Better Health Network, Health Tips, Research
No Comments »

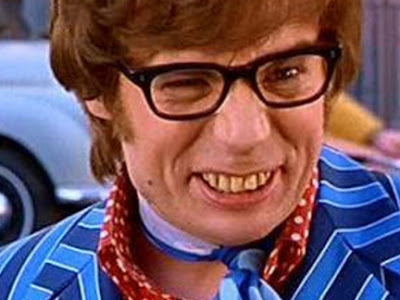
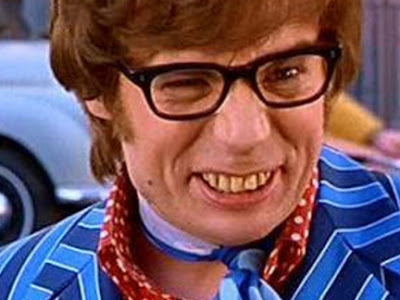 The British Medical Journal reported on a study of toothbrushing and found that people with poor oral hygiene had an increased risk of cardiovascular disease and heart attack.
The British Medical Journal reported on a study of toothbrushing and found that people with poor oral hygiene had an increased risk of cardiovascular disease and heart attack.
We’ve known for the last two decades that inflammation plays an important role in atherosclerosis. Markers of low-grade inflammation like C-reactive protein are also shown to be higher in heart disease.
The Scottish Health researchers looked at the general population and followed a large subset with questions about their oral health. They asked about frequency of dentist visits, toothbrushing, and controlled for many co-variables such as general activity, hypertension, smoking, height and weight. They also collected blood for studies of C-reactive protein as a marker of inflammation. They removed from the analysis participants who had no natural teeth (edentulous) and those with existing cardiovascular disease.
This elaborate and lengthy study showed that toothbrushing is associated with cardiovascular disease, and that subjects who brushed their teeth less than once a day had a 70 percent increase in heart disease compared with people who brushed twice a day. The inflammation that periodontal disease causes is directly related to increased C-reactive protein and increased heart attacks.
Leave it to the Scotts and the Brits to remind us to brush and floss every day.
REFERENCE: British Medical Journal, 2010; 340: c2451.
*This blog post was originally published at EverythingHealth*
May 28th, 2010 by StaceyButterfield in Better Health Network, Health Tips, Humor, Opinion, True Stories
No Comments »

 Want to know the secret to successful care of ICU patients? Think back to the advice your grandmother always gave, joked American Thoracic Society conference speaker Renee Stapleton, M.D., recently:
Want to know the secret to successful care of ICU patients? Think back to the advice your grandmother always gave, joked American Thoracic Society conference speaker Renee Stapleton, M.D., recently:
– Wash your hands.
– You can’t sleep your life away.
– Get some exercise.
– Sit up straight.
– Take your medicine.
– If you can’t remember it, write it down.
*This blog post was originally published at ACP Hospitalist*
May 26th, 2010 by Debra Gordon in Better Health Network, Health Policy, Health Tips, News, Opinion, True Stories
2 Comments »

I just read a Wall Street Journal article about a new web-based service called MedWaitTime that allows patients to check if their doctor is running late before heading to the office for their appointment — kind of like you can check to see if your flight is late before heading to the airport.
Brilliant.
Nothing peeves me more than sitting in a doctor’s office reading 4-month-old tattered magazines on topics I care nothing about (saltwater fishing, seriously?), and not because the doctor had an emergency (when is the last time a dermatologist had to run out to save someone), but because the office staff routinely double books. I can’t count the number of times I walked out (my limit is 30 minutes unless I’m in agony) after giving the front office a targeted piece of my mind. Read more »
*This blog post was originally published at A Medical Writer's Musings on Medicine, Health Care, and the Writing Life*
May 26th, 2010 by DrRob in Better Health Network, Health Policy, Opinion, True Stories
No Comments »

The recent discussion of the appropriateness of bringing patients back to the office has really gotten me thinking about my overall philosophy of practice. What are the rules that govern my time in the office with patients? What determines when I see people, what I order, and what I prescribe? What constitutes “good care” in my practice?
So I decided to make some rules that guide what I think a doctor should be doing in the exam room with the patient. They are as much for my patients as they are for me, but I believe that thinking this out will give clarity in the process.
Rule 1: It’s the Patient’s Visit
The visit is for the patient’s health, not the doctor’s income or ego. This means three things:
- All medical decisions should be made for what is in their interest, including: when they should come in, what medications they are given, what tests are ordered, and what consults are made.
- Patients who request things that are harmful to themselves should be denied. People who ask for addictive drugs or unnecessary tests should not get them. Patients who are doing harmful things to themselves should be warned, but only in a way that is helpful, not judgmental.
- All tests done on the patient should be reported to them in a way that they can understand.
Rule 2: Minimize
Many doctors and patients have a “more is better” mentality. This not only costs more money to the system, but it can cause harm to the patient. Read more »
*This blog post was originally published at Musings of a Distractible Mind*
May 26th, 2010 by KevinMD in Better Health Network, Health Policy, Opinion
No Comments »

Much has been recently made about the bureaucratic obstacles that primary care doctors face. With good reason. The impetus was a recent New England Journal of Medicine paper from Richard J. Baron that I mentioned recently.
The New York Times’ Pauline Chen interviewed Dr. Baron, who shared some interesting insights on what needs to be done. He contrasts the inertia in primary care to drug manufacturing.
If you took the resources that went into drug development, for instance, “and put them into a program like this that achieves meaningful levels of behavior change, a lot more patients could be better off.” In other words, research into new primary care models isn’t taking off because the money isn’t there.
But Dr. Baron also notes that money isn’t everything, since “primary care practitioners have been saying that we either already do or would do certain things if you paid us more. It’s true that you can’t do things consistently, reliably and across scales without additional payment. But payment is not enough. People have to change what they are thinking about when they go to work.” Read more »
*This blog post was originally published at KevinMD.com*
 The British Medical Journal reported on a study of toothbrushing and found that people with poor oral hygiene had an increased risk of cardiovascular disease and heart attack.
The British Medical Journal reported on a study of toothbrushing and found that people with poor oral hygiene had an increased risk of cardiovascular disease and heart attack.



 Want to know the secret to successful care of ICU patients? Think back to the advice your grandmother always gave, joked
Want to know the secret to successful care of ICU patients? Think back to the advice your grandmother always gave, joked 










