May 1st, 2011 by admin in Opinion
No Comments »

The rise of prophylactic double mastectomy in women with increased risk of breast cancer has been a topic of recent discussion. In particular, this trend has been observed amongst women with the diagnosis of unilateral carcinoma in situ, or pre-invasive breast cancer. While it has been known that in women with genetic cancer syndromes, including BRCA1 and BRCA2, double mastectomy reduces risk, the efficacy of the approach is uncertain in women with other risk profiles, yet more women and surgeons seem to be doing it.
Knowing when to test, treat and act is part of art of medical practice. The ability to convey this information effectively is also an art. Both patients and doctors may have a hard time embracing watchful waiting with respect to many forms of cancer and pre-cancer. In the case of cancer of the cervix, it is known that infection with human papillomavirus (HPV) is causative in cancer development. However, only a small percentage of those infected actually go on to get cancer. Low grade dysplasia, a condition that is early in the cervical cancer development continuum, frequently spontaneously resolves without treatment. Fortunately, in the case of cervical cancer, there is now a vaccine to prevent high risk HPV infection.
“Watchful waiting” has been most discussed as a treatment strategy for prostate cancer. Read more »
*This blog post was originally published at ACP Internist*
April 25th, 2011 by DrWes in Health Policy, Opinion
No Comments »


The above graph from the Cato Institute demonstrates the growing complexity of the U.S. tax code over the years. After doing my taxes recently and trying to track the ins and outs of the law for my wife’s private practice, I can attest to the graph’s accuracy.
But then I was reading an interesting editorial in Circulation: Arrhythmia and Electrophysiology by N.A. Mark Estes III, MD and Jonathan Weinstock, MD that reviewed an article by Roos, et al in the same journal that found only 27 of 698 guideline recommendations from the European Society of Cardiology (median 1.2% per guideline [IQR 0.95% to 3.7%]) were correctly referenced as Class I or III Level of Evidence A recommendations, calling into question the accuracy of guideline recommendations. In their editorial, Estes and Weinstock defended the guideline process but also mentioned the following shocking statistic: Read more »
*This blog post was originally published at Dr. Wes*
March 31st, 2011 by admin in Health Policy, Health Tips, Research
No Comments »
By Richard C. Hunt, MD, FACEP
Centers for Disease Control and Prevention
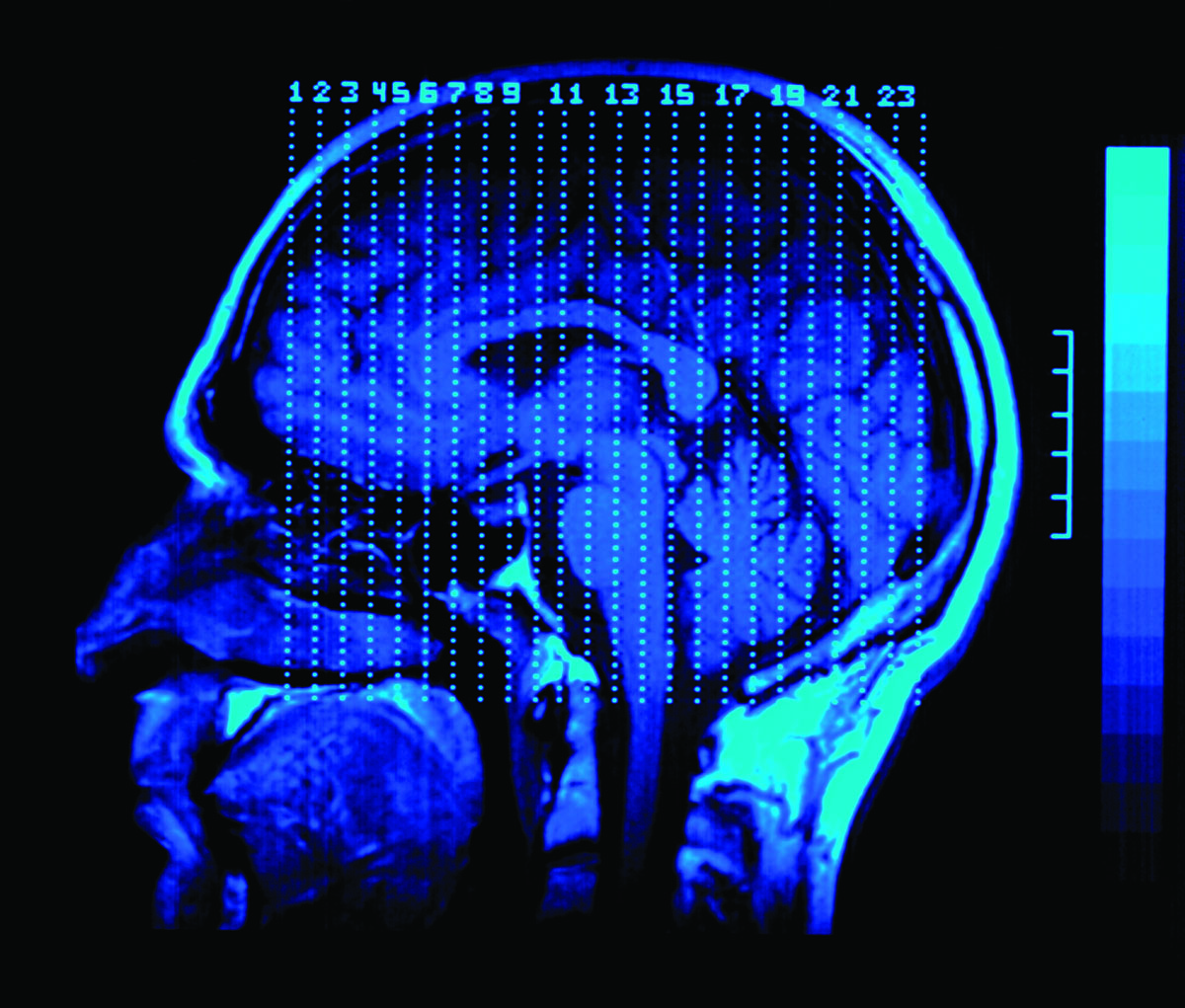
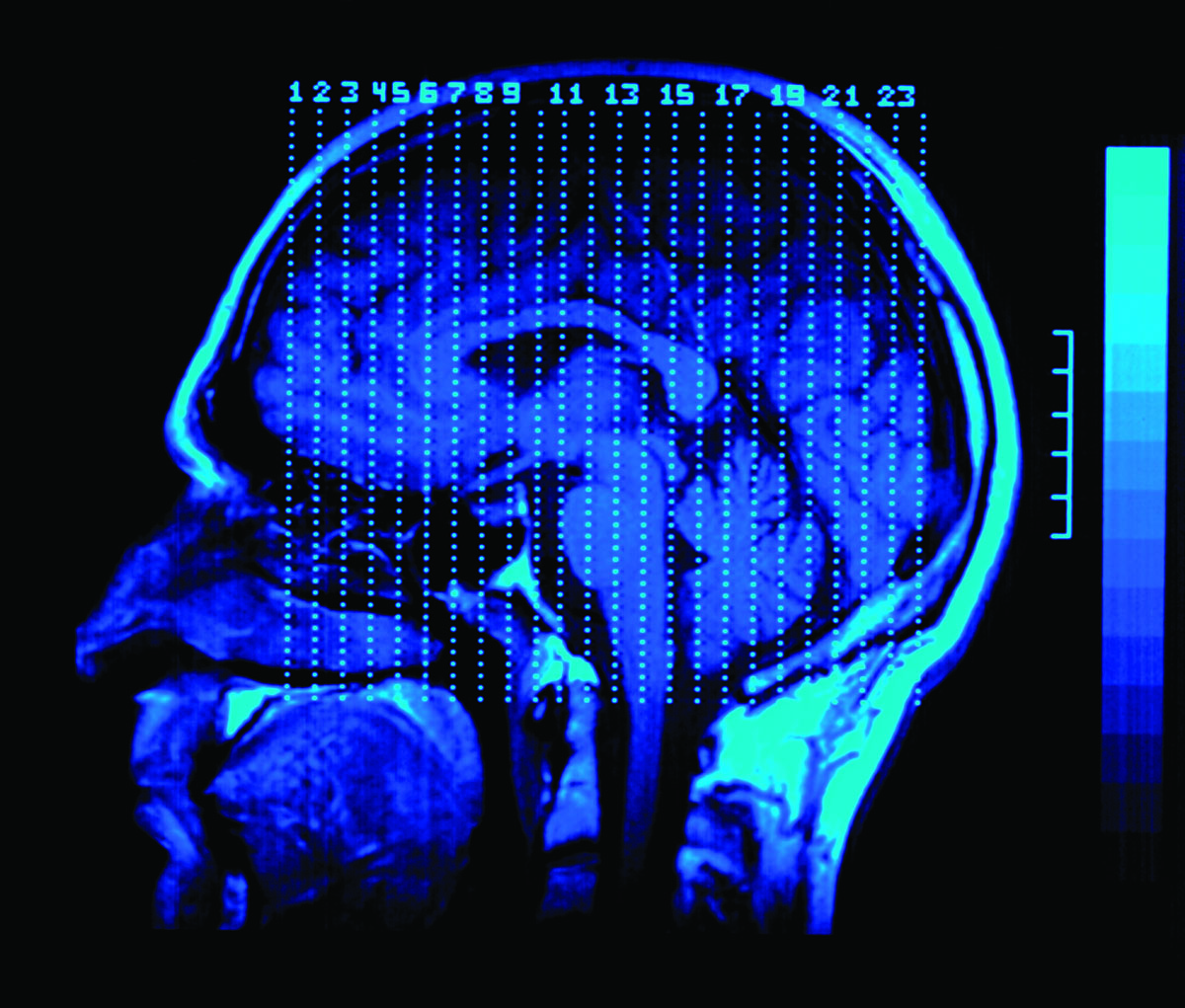
A 17 year-old athlete arrives on the sideline, at your office, or in the emergency department after hitting her head during a collision on the sports field and is complaining that she has a headache and “just doesn’t feel right.”
Can she return to play? If not, when can she safely return to school, sports, and to her normal daily activities? Does she need immediate care, a Head CT or MRI, or just some time to rest?
Do those questions sound familiar?
Each year thousands of young athletes present at emergency departments and in the primary care setting with a suspected sports- and recreation-related concussion. And every day, health care professionals, like us, are challenged with identifying and appropriately managing patients who may be at risk for short- or long-term problems.
As you know, concussion symptoms may appear mild, but this injury can lead to significant, life-long impairment affecting an individual’s ability to function physically, cognitively, and psychologically. Thus, appropriate diagnosis, referral, and education are critical for helping young athletes with concussion achieve optimal recovery and to reduce or avoid significant sequelae.
And that’s where you come in. Health care professionals play a key role in helping to prevent concussion and in appropriately identifying, diagnosing, and managing it when it does occur. Health care professionals can also improve patient outcomes by implementing early management and appropriate referral.
As part of my work at CDC, and as a health care professional, I am committed to informing others about CDC’s resources to help with diagnosing and managing concussion. CDC collaborated with several organizations and leading experts to develop a clinical guideline and tools for the diagnosis and management of patients with concussion, including:
For more information about the diagnosis and management of concussion, please visit www.cdc.gov/Concussion/clinician.html.
Also, learn more about CDC’s TBI activities and join the conversation at: www.facebook.com/cdcheadsup.
March 28th, 2011 by DrWes in Health Policy
No Comments »

In case people are wondering if our governmental overlords really care about the latest and greatest treatment guidelines published by our professional health care organizations, take note.
CMS (Center for Medicare and Medicaid Services) is still using guidelines for defibrillator implantation from 2005 to justify payment for services in their national coverage decision, whereas the latest guidelines published by the Heart Rhythm Society published in 2008 carry signficiant differences in their recommendations for appropriate patients for this technology.
So which set of guidelines should doctors use?
The answer is obvious: if you use the latest data to decide who should receive a defibrillator, you might be subject to a Department of Justice investigation.
So much for using updated guidelines.
-WesMusings of a cardiologist and cardiac electrophysiologist.



*This blog post was originally published at Dr. Wes*
July 28th, 2010 by Davis Liu, M.D. in Better Health Network, Health Policy, News, Opinion, Research
2 Comments »

 The American College of Obstetricians and Gynecologists (ACOG) recently reiterated their position that Pap smears should be performed on healthy women starting at age 21. This is different from the past which recommended screening for cervical cancer at either three years after the time a woman became sexually active or age 21, whichever occurred first.
The American College of Obstetricians and Gynecologists (ACOG) recently reiterated their position that Pap smears should be performed on healthy women starting at age 21. This is different from the past which recommended screening for cervical cancer at either three years after the time a woman became sexually active or age 21, whichever occurred first.
How will the public respond to this change?
Over the past year there have been plenty of announcements from the medical profession regarding to the appropriateness of PSA screening for prostate cancer and the timing of mammogram screening for breast cancer. Understandably, some people may view these changes in recommendations as the rationing of American healthcare. Read more »
*This blog post was originally published at Saving Money and Surviving the Healthcare Crisis*