March 27th, 2017 by Dr. Val Jones in Health Policy, True Stories
No Comments »
 We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
Take for example, the elderly woman who was leading an active life in retirement. She was the chairman of the board at a prestigious company, was an avid Pilates participant, and the caregiver for her disabled son. A new physician at her practice recommended a higher dose of diuretic (which she dutifully accepted), and several days later she became delirious from dehydration. She was admitted to the local hospital where it was presumed, due to her age, that she had advanced dementia. Hospice care was recommended at discharge. All she needed was IV fluids.
I recently cared for an attorney in her 70’s who had a slow growing brain tumor that was causing speech difficulties. She too, was written off as having dementia until an MRI was performed to explore the reason for new left-eye blindness. The tumor was successfully removed, but she was denied brain rehabilitation services because of her “history of dementia.”
Of course, I recently wrote about my 80-year-old patient, Jack, who was presumed to be an alcoholic when he showed up to his local hospital with a stroke.
Hospitalized patients are often very different than their usual selves. As we age, we become more vulnerable to medication side-effects, infections, and delirium. And so, the chance of an elderly hospitalized patient being acutely impaired is much higher than the general population. Unfortunately, many hospital-based physicians and surgeons — and certainly nurses and therapists — have little or no prior knowledge of the patient in their care. The patient’s “normal baseline” must often be reconstructed with the help of family members and friends. This takes precious time, and often goes undone.
Years ago, a patient’s family doctor would admit them to the hospital and care for them there. Now that the breadth and depth of our treatments have given birth to an army of sub-specialists, we have increased access to life-saving interventions at the expense of knowing those who need them. This presents a peculiar problem – one in which we spend enormous amounts of resources on diagnostic rabbit holes, because we aren’t certain if our patients’ symptoms are new or old. Was Mrs. Smith born with a lazy eye, or is she having a brain bleed? We could ask a family member, but we usually order an MRI.
My plea is for healthcare staff to be very mindful of the tendency to profile seniors. Just because Mr. Johnson has behavioral disturbances in his hospital room doesn’t mean that he is like that at home. Be especially suspicious of reversible causes of mental status changes in the elderly, and presume that patients are normally functional and bright until proven otherwise.
Last month I hit a new age record at my rehab hospital – I admitted a charming, active, 103-year-old woman after a small stroke caused her some new weakness. She was highly motivated in therapy, improved markedly and was discharged to an independent living center. I bet she will live many more years. When I joked that she didn’t look a day over 80, she winked and told me she had stopped counting birthdays years ago. She said, “It doesn’t matter how old you are, it matters what you can do. And I can do a lot.”
February 20th, 2016 by Dr. Val Jones in Opinion
6 Comments »
 Hope is a tricky thing. On the one hand, false hope can lead patients to opt for painful, futile treatments at the end of life. On the other, unnecessarily bleak outlooks can lead to depression and inaction. When health is at stake, presenting information with the right amount of hope can guide patients away from both suffering needlessly and/or succumbing to treatable disease.
Hope is a tricky thing. On the one hand, false hope can lead patients to opt for painful, futile treatments at the end of life. On the other, unnecessarily bleak outlooks can lead to depression and inaction. When health is at stake, presenting information with the right amount of hope can guide patients away from both suffering needlessly and/or succumbing to treatable disease.
I was reading a sad story about a patient whose physician had made her feel hopeless. She was an elderly widow with some real, but not immediately life-threatening, medical conditions. His attitude led her to believe that she was sick and useless – with little to look forward to but ongoing testing, disease progression and eventual death. His professional opinion held special weight for her, coloring her entire outlook. It wasn’t until a friend reminded her of the doctor’s fallibility that she began to question her diagnoses, treatment options, and even prognosis.
When faced with concerning new medical diagnoses, even the most educated among us tend to imagine the worst case scenario. Knowing this, physicians should take care to offer reassurance and optimism whenever it is warranted. Hope provides the energy to course correct, to fight battles that can be won, and to hold on to trust in a brighter future. Why be stingy with it when it is so easily given?
As a rehab physician I have regularly encountered bias on the part of healthy people in regards to certain injuries. I hear them whisper, “I wouldn’t want to go on living if I couldn’t walk” or “That poor man’s life must be ruined.” And yet, these feelings are not shared by those fighting the battles. In many cases, losing an ability focuses the mind on what’s important – and on all the things that can still be achieved and enjoyed. Life is a gift, and while we all still have breath – we can make meaningful contributions.
It breaks my heart to see patients lose hope, and it is sadder still when physicians facilitate the loss. What we say carries psychological weight, and we should recognize the duty we have to deliver information with kindness and respect – focusing on the possible, dispelling unreasonable fears, and emphasizing that inner peace is attainable no matter the circumstance.
In healthcare we ought to always have hope – not for perfect health, or longer life – but in our ability to overcome obstacles, to make good come from bad, and to have a positive impact on others. The choice to live our best life is ours to make, no matter the disease or condition. Never let a doctor steal your hope, but adopt the rehab mission: to add life to years.
September 30th, 2015 by Dr. Val Jones in Opinion
No Comments »
 Hospital culture is largely influenced by the relationship between administrative and clinical staff leaders. In the “old days” the clinical staff (and physicians in particular) held most of the sway over patient care. Nowadays, the approach to patient care is significantly constricted by administrative rules, largely created by non-clinicians. An excellent description of what can result (i.e. disenfranchisement of medical staff, burn out, and joyless medical care) is presented by Dr. Robert Khoo at KevinMD.
Hospital culture is largely influenced by the relationship between administrative and clinical staff leaders. In the “old days” the clinical staff (and physicians in particular) held most of the sway over patient care. Nowadays, the approach to patient care is significantly constricted by administrative rules, largely created by non-clinicians. An excellent description of what can result (i.e. disenfranchisement of medical staff, burn out, and joyless medical care) is presented by Dr. Robert Khoo at KevinMD.
Interestingly, a few hospitals still maintain a power shift in the other direction – where physicians have a strangle hold on operations, and determine the facility’s ability to make changes. This can lead to its own problems, including unchecked verbal abuse of staff, inability to terminate bad actors, and diverting patients to certain facilities where they receive volume incentive remuneration. Physician greed, as Michael Millenson points out, was a common feature of medical practice pre-1965. And so, when physicians are empowered, they can be as corrupt as the administrations they so commonly despise.
As I travel from hospital to hospital across the United States (see more about my “living la vida locum” here), I often wonder what makes the pleasant places great. I have found that prestige, location, and generous endowments do not correlate with excellent work culture. It is critically important, it seems, to titrate the balance of power between administration and clinical staff carefully – this is a necessary part of hospital excellence, but still not sufficient to insure optimal contentment.
In addition to the right power balance, it has been my experience that hospital culture flows from the personalities of its leaders. Leaders must be carefully curated and maintain their own balance of business savvy and emotional I.Q. Too often I find that leaders lack the finesse required for a caring profession, which then inspires others to follow suit with bad behavior. Unfortunately, the tender hearts required to lead with grace are often put off by the harsh realities of business, and so those who rise to lead may be the ones least capable of creating the kind of work environment that fosters collaboration and kindness. I concur with the recent article in Forbes magazine that argues that poor leaders are often selected based on confidence, not competence.
The very best healthcare facilities have somehow managed to seek out, support and respect leaders with virtuous characters. These people go on to attract others like them. And so a ripple effect begins, eventually culminating in a culture of carefulness and compassion. When you find one of these gems, devote yourself to its success because it may soon be lost in the churn of modern work schedules.
Perhaps your hospital work environment is toxic because people like you are not taking on management responsibilities that can change the culture. Do not shrink from leadership because you’re a kind-hearted individual. You are desperately needed. We require emotionally competent leaders to balance out the financially driven ones. It’s easy to feel helpless in the face of a money-driven, heavily regulated system, but now is not the time to shrink from responsibility.
Be the change you want to see in healthcare.
January 21st, 2015 by Dr. Val Jones in Opinion, True Stories
1 Comment »
 In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
In my last blog post I discussed how harmful physician “thought leaders” can be when they are dismissive of the value of other specialists’ care. I must have touched a nerve, because a passionate discussion followed in the comments section. It seems that physicians (who spend most of their time involved in clinical work) are growing tired of the leadership decisions of those who engage in little to no patient care. Clinicians urge lawmakers to turn to practicing physicians for counsel, because those who are out of touch with patients lack real credibility as advisers.
Interestingly, the credibility question was raised in a different light when I was recently contacted by a prestigious medical organization that was seeking expansion of its board membership. I presumed that this was a personal invitation to join the cause, but soon realized that the caller wanted to use my influence to locate “more credible” candidates with academic gravitas.
When I asked what sort of candidate they wanted my help to find, the response was:
“A physician with an academic appointment at a name brand medical school. Someone who isn’t crazy – you know, they have to be respected by their peers. Someone at Harvard or Columbia would be great. You must know someone from your training program at least.”
While I appreciated the honesty, I began thinking about the age-old “town versus gown” hostilities inspired by academic elitism. In medicine, as with many other professions, it is more prestigious to hold an academic position than to serve in a rural community. But why do we insist on equating credibility with academics?
Another facet of credibility lies in physicians’ tendencies to admire only those at the top of their specific specialty. Dr. Lucy Hornstein described this phenomenon in her powerful essay on “How To Drive Doctors To Suicide:”
“Practice that condescending look and use it at hospital staff events. Make it a point to ignore newcomers. Concentrate on talking just with your friends and laughing at inside jokes, especially when others are around. Don’t return their calls, and don’t take their calls if you can possibly help it. If you accidentally wind up on the phone with the patient’s primary physician, just tell them you’ve got it all under control, and that he (and the patient) are so lucky you got involved when you did.”
A reader notes:
“And perhaps those of us who do see patients should get some self esteem and stop fawning all over [physician thought leaders] at conferences like needy interns.”
And finally, there seems to be an unspoken pecking order among physicians regarding the relative prestige of various specialties. How this order came about must be fairly complicated, as dermatology and neurosurgery seem to by vying for top spots these days. I find the juxtaposition almost amusing. Nevertheless, it’s common to find physicians in the more popular specialties looking down upon the worker bees (e.g. hospitalists and family physicians) and oddballs (e.g. physiatrists and pathologists).
While I try very hard not to take offense at my peers’ dismissiveness of my career’s value, it becomes much more concerning when funding follows prejudicial lines in the medical hierarchy. As a sympathetic family physician writes:
“I have observed the inequitable distribution of resources from the less glamorous to the sexy sub specialties despite obvious patient needs. Unfortunately, the administridiots who usually lack any medical training, opt to place resources where they are most likely to attract headlines.”
Yes, caring for the disabled (PM&R) is “less glamorous” than wielding a colonoscope (GI) (again, not sure who made that decision?) but it should not be less credible, or become a target for budget cuts simply because people aren’t informed about how rehab works.
It is time to stop specialty prejudice and honor those who demonstrate passion for patients, regardless of which patient population, body part, or organ system they serve. Excellent patient care may be provided by academics, generalists, or specialists, by those who practice in rural areas or in urban centers. The best “thought leaders” are those who bring unity and an attitude of peer respect to the medical profession. With more of them, we may yet save ourselves from mutually assured destruction.
 We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.
We’ve all heard the saying, “age is just a number.” Nowhere is that more important than in the hospital setting. Over the years I’ve become more and more aware of ageism in healthcare – a bias against full treatment options for older patients. Assumptions about lower capabilities, cognitive status and sedentary lifestyle are all too common. There is a kind of “senior profiling” that occurs among hospital staff, and this regularly leads to inappropriate medical care.

 Hope is a tricky thing. On the one hand, false hope can lead patients to opt for painful, futile treatments at the end of life. On the other, unnecessarily bleak outlooks can lead to depression and inaction. When health is at stake, presenting information with the right amount of hope can guide patients away from both suffering needlessly and/or succumbing to treatable disease.
Hope is a tricky thing. On the one hand, false hope can lead patients to opt for painful, futile treatments at the end of life. On the other, unnecessarily bleak outlooks can lead to depression and inaction. When health is at stake, presenting information with the right amount of hope can guide patients away from both suffering needlessly and/or succumbing to treatable disease. Hospital culture is largely influenced by the relationship between administrative and clinical staff leaders. In the “old days” the clinical staff (and physicians in particular) held most of the sway over patient care. Nowadays, the approach to patient care is significantly constricted by administrative rules, largely created by non-clinicians. An excellent description of what can result (i.e. disenfranchisement of medical staff, burn out, and joyless medical care) is presented
Hospital culture is largely influenced by the relationship between administrative and clinical staff leaders. In the “old days” the clinical staff (and physicians in particular) held most of the sway over patient care. Nowadays, the approach to patient care is significantly constricted by administrative rules, largely created by non-clinicians. An excellent description of what can result (i.e. disenfranchisement of medical staff, burn out, and joyless medical care) is presented 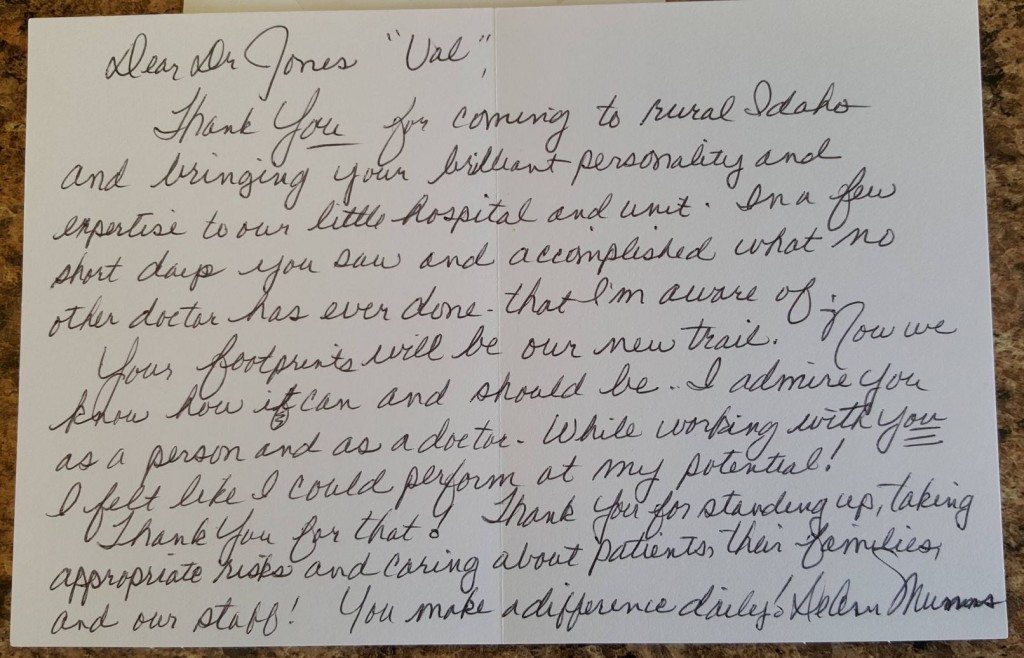
 In my
In my







