Cartoon: Why Are Hospitals So Noisy?


No matter how sick my grandmother got or what her doctors said, she refused to go to the hospital because she thought it was a dangerous place. To some degree, she was right. Although hospitals can be places of healing, hospital stays can have serious downsides, too.
One that has been getting a lot of attention lately is the development of delirium in people who are hospitalized. Delirium is a sudden change in mental status characterized by confusion, disorientation, altered states of consciousness (from hyperalert to unrousable), an inability to focus, and sometimes hallucinations. It’s the most common complication of hospitalization among older people.
We wrote about treating and preventing hospital delirium earlier this year in the Harvard Women’s Health Watch. In the New York Times “The New Old Age” blog, author Susan Seliger vividly describes her 85-year-old mother’s rapid descent into hospital delirium, and tips for preventing it.
Although delirium often recedes, it may have long-lasting aftereffects. Read more »
*This blog post was originally published at Harvard Health Blog*
Chronically-ill Medicare patients spent fewer days in the hospital and received more hospice care in 2007 than they did in 2003, but their intensity of care increased as well, according to a report by the Dartmouth Atlas Project.
While in the hospital less, patients had many more visits from physicians, particularly specialists, and spent more days in intensive care units, as result of growth in intensive care and specialist capacity, the researchers said.
Intensive interventions can lower a patients’ quality of life and cost more, the researchers noted. About one-fourth of all Medicare spending stems from the last year of life, and much of the growth in Medicare spending is the result of the high cost of treating chronic disease, the authors noted. Following patient preferences for end-of-life care may reduce such spending. Read more »
*This blog post was originally published at ACP Hospitalist*
I read this article about a young child with heterotaxy syndrome with great interest. Not because I find heterotaxy syndrome something of great fascination, but because of the lack of communication — on both ends of the spectrum:
Even though 5 other Dr. all came in and listened to his lungs and said that he didn’t sound like he was wheezing and that his lungs sounded really good. But because this hospital is overly political, process driven, bureaucratic, and in a constant state of litigious fear they are unable to make any conclusions based on actual medicine and patient care. Common sense is blown out the window when you have a system were a hospitalist one year out of medical school has an opinion that is as valuable as a cardiologist with 25+ years experience.
But in fairness, they all had to “really consider her opinion.”
So they went and got a pulmonologist to evaluate him, which Scott and I were very happy about because there was nothing in the world that would’ve made me more happy in that moment than to have her proven wrong. Which she was.
The whole article is a case study in stress, distrust, and legalism. Read more »
*This blog post was originally published at The Happy Hospitalist*
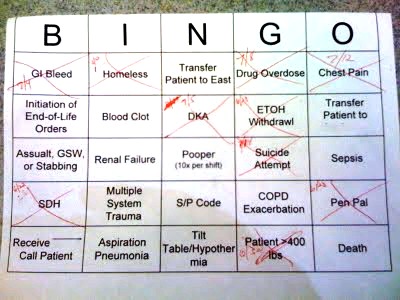
Ever wonder how ICU nurses get through their daily grind? Why, with ICU Bingo, of course.
How does ICU Bingo work? It works just like regular bingo. Every nurse receives their own Bingo card with different ICU diagnoses. And every time they take care of one of these conditions, they get to “x” it out. Fill out a line or any other predetermined design pattern, and you are the ICU Bingo winner, and you win a prize.
This is quite similar to my 2010 March Madness Hospitalist Bracket, only in this case the game is Bingo. As you can see, this nurse has already cared for a GI bleed, a homeless man, a drug overdose, chest pain, DKA, alcohol withrawal, subdural hematoma, a prisoner, and someone with super-morbid obesity. That’s ICU medicine for you.
*This blog post was originally published at The Happy Hospitalist*
It’s no secret that doctors are disappointed with the way that the U.S. healthcare system is evolving. Most feel helpless about improving their work conditions or solving technical problems in patient care. Fortunately one young medical student was undeterred by the mountain of disappointment carried by his senior clinician mentors…
I am proud to be a part of the American Resident Project an initiative that promotes the writing of medical students residents and new physicians as they explore ideas for transforming American health care delivery. I recently had the opportunity to interview three of the writing fellows about how to…
Book Review: Is Empathy Learned By Faking It Till It’s Real?

I m often asked to do book reviews on my blog and I rarely agree to them. This is because it takes me a long time to read a book and then if I don t enjoy it I figure the author would rather me remain silent than publish my…
The Spirit Of The Place: Samuel Shem’s New Book May Depress You

When I was in medical school I read Samuel Shem s House Of God as a right of passage. At the time I found it to be a cynical yet eerily accurate portrayal of the underbelly of academic medicine. I gained comfort from its gallows humor and it made me…
Eat To Save Your Life: Another Half-True Diet Book

I am hesitant to review diet books because they are so often a tangled mess of fact and fiction. Teasing out their truth from falsehood is about as exhausting as delousing a long-haired elementary school student. However after being approached by the authors’ PR agency with the promise of a…