April 14th, 2011 by DrWes in True Stories
No Comments »
It was 11:00 pm when the pager vibrated, then beeped: it was the ER, Hospital #3.
“This is Dr. Fisher returning your page?”
“Thank you Dr. Fisher, just a moment for Dr. Frigamafratz.”
A brief pause, then:
“Wes, I think we’ll need your services. Old guy, found down at the nursing home, brought in unconscious, pulse 25 – hooked him up to an external pacer, he’s back with us now.”
“I’m on my way.”
When I arrived, there was the usual cacophony of activity in the Emergency Room. Someone screaming in one corner. Intercom sounding. Ambulance en route to our location. Breathing treatments underway in Bay 5. Room 10 headed to the CT scanner. Has room 12 got a bed? By comparison my patient was easy: his disposition in the eyes of the ER staff had been made: he was on the Express Track to the EP lab.
There he was, chest twitching. Big forceful jerking. He was a big guy, uttering something with purpose but impossible to understand. Next to him, his wife, just arriving and removing her coat. “Is he going to be okay?”
My head scrambled for an answer. “He’s okay for now,” I think I replied. Read more »
*This blog post was originally published at Dr. Wes*
November 27th, 2010 by DavidHarlow in Better Health Network, Health Policy, Health Tips, Medblogger Shout Outs, News
No Comments »
As patients, as family members, as friends, as health care providers, we have all faced end-of-life issues at one time or another, and we will face them again. And again.
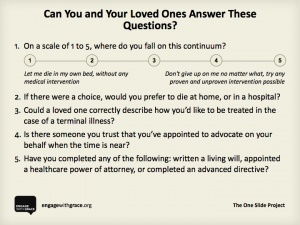
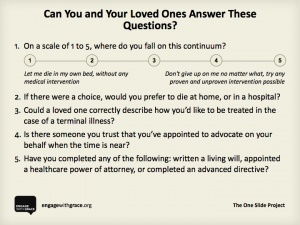
This weekend the “Engage With Grace” message is being broadcast virally, through a “blog rally,” at a time when many people are with family and friends over the long weekend. The point is: We all need to have the potentially uncomfortable conversation with people close to us about what kind of treatment we would want, and they would want, if incapable of making or communicating healthcare decisions. CNN ran a story on “Engage With Grace” yesterday.
End-of-life decision-making has long been an issue of great personal and professional interest to me, and I am proud to have played a role in having out-of-hospital DNR orders recognized in Massachusetts by EMS providers, as an example. Read more »
*This blog post was originally published at HealthBlawg :: David Harlow's Health Care Law Blog*
October 19th, 2009 by CodeBlog in Better Health Network, True Stories
No Comments »

He knew she was angry with him.
“Whenever I come to see her, I reach out and take her hand, but she looks away.”
Husband and wife for well over 50 years, they had been through a lot. They met in another country in another time, and to hear him tell it, it almost seemed fated that they’d end up together. Since then, they’d moved many times, raised a family, supported each other through myriad illnesses. They were growing old together.
Unfortunately, “growing old together” doesn’t always work out like we hope it will. Diseases and illnesses ravage our bodies; dementia ravages our brains. She’d long ago given up on their little garden in the backyard. It was her favorite hobby, but she couldn’t manage it anymore. Read more »
*This blog post was originally published at code blog - tales of a nurse*
August 17th, 2009 by DrRob in Better Health Network, Health Policy, Opinion
2 Comments »
Death panels. They are all the trend these days.
I went to Home Depot to look for some, but couldn’t find any. There was some drywall of doom, tiles of the abyss, and sheet rock of destruction, but no panels. I guess the Obama administration has bought them all.
Honestly, I am not sure what the “death panel” fuss is about. Everyone dies. There are times it is a surprise, but many times it is expected. When it is expected, shouldn’t people plan for it? Shouldn’t we encourage people to plan for it?
The focus of a physician is twofold: to prolong life and to minimize suffering. We practice preventive medicine to keep the person from avoidable pain and/or death. The younger the patient is, the more we call their death things like tragic, pointless, and distressing. We go to great lengths to save the life of someone who has many potential years ahead.
But there is a point when things change. There is a point when the focus shifts from quantity of life to quality of life. There is a time after which a death is no longer tragic, but instead the end of a story. My focus as a physician shifts from trying to find and prevent disease, to maximizing function and minimizing pain. When does this happen? It depends on the health of the patient. But eventually, ignoring one’s inevitable end becomes more tragic than the end itself.
I had a man in my practice who had advanced Alzheimer’s disease. I cared for him before he started his decline, and so had a good chance to know both him and his family. They were people of strong faith, accepting the hard things in life as being from the hand of God. The children took their father’s condition not as a horrible burden, but an opportunity to pay back the man who had given them so much. There was no fear of illness or death.
His wife died fairly soon after I started caring for them. He grieved greatly when she died, but was so surrounded with the love of their children that his grief was short. He spoke often of her in subsequent visits, talking about her as if she was not far away.
As he became increasingly short in his memory, my relationship with their children grew. You can tell a lot about people from their children, and these children were a dazzling crown of honor to these two lovely people.They always came asking good questions, patiently dealing with their father’s confusion, anxiety, and occasional outbursts. Together we worked to maximize his quality of life. When I suggested we stop cholesterol medication and cancer screening tests, they understood. Our focus would not be on the length of life, but the quality of time they could spend with their father.
I was shocked, therefore, when the report of his admission to the hospital came across my desktop. He had chest pains and some difficulty breathing. In the emergency room, a plethora of lab tests, x-rays, and other studies were done. The hospitalist physician on call felt there was a good possibility of heart attack or pulmonary embolism (blood clot to the lung). My patient was sent to the ICU, where he underwent CT angiography, serial lab tests, and even a stress test to rule out heart problems.
I was mystified as I read these reports; the family clearly understood that prolonging his life wasn’t the goal. The patient was ready to die and join his wife, and the children were very comfortable talking about his eventual death. These reports made absolutely no sense with what I knew of this man and his family.
He looked his normal self when he came in to my office for a hospital follow-up. I questioned the daughter about the details of the admission, which she recounted carefully. Then I paused and asked her, “Can I ask you one more thing?”
She smiled at me, “Of course, Dr. Rob” she said gently.
“I was honestly a little surprised when I read about your father’s admission to the hospital. It seems like they pulled out all the stops, even putting him in the ICU. Did they ask you if this is what you wanted? I thought that you wouldn’t want to be that aggressive.”
She thought about what I said and a puzzled expression slowly appeared on her face.
“Did you ask to have everything done, or did you just follow what the doctors at the hospital told you?” I asked.
“They didn’t ask us. We just did what they told us we needed to do.” she said, now scowling slightly.
I explained to her that they need to make their wishes known in advance. If they don’t say anything, the doctors will assume that you agree with what they are doing. As I told her this, she nodded and looked down sadly.
“It’s OK what you did” I reassured her. I patted her father on the shoulder and added, “he looks great now. I am glad I get to see him again. I just want you to know what to do if it happens in the future. You never know what will happen, and I’d hate for him to suffer needlessly.”
This one short hospital stay undoubtedly amassed a bill many times that of all my bills over the 12 years I saw him in my office. My years of care, long conversations, and real personal connection built with this man and his family are worth only a fraction of a few days of unnecessary care. This care was not demanded by the family. It was not done because of denial or ignorance; it was because the family wasn’t prepared for the mechanics of the hospital stay. I never had that conversation with the family until after this event.
Politicians have labeled this merciful conversation as an act of rationing. That is not only ignorant, it is shameful. Talking to people about end-of-life issues will certainly save money. But it’s a contemptible step to imply that this money is saved by killing the elderly. It’s more wrong to make money off of keeping them alive unnecessarily than it is to save money by letting them die when they choose.
This is politics at its ugliest – taking a provision that will reduce suffering and help people and pervert it to be used as a tool to scare the people it will help. The discussion about healthcare has been subverted by those who want poll numbers.
Shame on you.
*This blog post was originally published at Musings of a Distractible Mind*
November 26th, 2008 by Dr. Val Jones in Announcements
4 Comments »
Matthew Holt and Paul Levy have encouraged medical bloggers to join together around a common goal for Thanksgiving: to talk to our loved ones about end-of-life preferences. Now I know this may seem a bit morbid at first blush – but it is really important that each of us create a living will and durable power of attorney document. There’s no better time to discuss this than a holiday where we all get together with our families to enjoy one anothers’ company and our gratitude for what we have.
I used the Suze Orman site templates to create mine (I received a free CD Rom). It was really easy to do. Living Wills provide guidelines about your wishes for care in the event that you are unable to express your opinions. The Durable Power of Attorney document makes it clear whom you’d like to “call the shots” on your care if you’re unable to do so for yourself.
If you haven’t done so already, why not consider the following three steps over Thanksgiving?
1. Discuss the “Engage with Grace” slide with your loved ones.
2. Fill out living will and power of attorney documents at Suze’s site (or find another site online that has a good template that you can use to express your wishes).
3. Get those documents affirmed by a notary public and send a copy to your doctor to add them to your medical record.
Every person at every age needs to have an end-of-life care plan. Why not join with thousands of blog readers in settling this matter for yourself and your loved ones this Thanksgiving?